Colonic tissue samples taken during flexible sigmoidoscopy or colonoscopy can be used to predict whether or not a patient will develop Parkinson’s disease, researchers from Rush University Medical Center reported. The scientists reported findings from two studies in Movement Disorders.
As background information, the authors explain that nearly 5 million people globally are affected with Parkinson’s disease. This number is set to double over the next two decades.
Alpha-synuclein, a protein, collects in the cells of Parkinson’s patients. Alpha-synuclein has been found to be a pathologic hallmark of Parkinson’s disease. These protein aggregates form Lewy bodies, a structure typically found in the brains of patients with Parkinson’s after they died (at autopsy).
In a communiqué issued by Rush University, the authors wrote: “Identification of the role of alpha-synuclein aggregation in neuronal dysfunction and death has broadened understanding of how Parkinson’s disease develops and introduced a valuable tool for tracking its progress.”
The authors have shown that alpha-synuclein is also detectable in the nerve cells that lie in the intestinal walls in their research participants with early Parkinson’s – the protein is not present in healthy subjects.
Dr. Kathleen M. Shannon and team collected intestinal wall samples from 10 participants with early Parkinson’s – flexible sigmoidoscopy was used; a technique similar to colonoscopy in which a flexible scope is threaded into the lower intestine. No colon preparation or anesthesia are required with flexible sigmoidoscopy; the scope only goes in about 8 inches. The whole procedure takes no more than 10 minutes to complete.
In an online communiqué, Rush University wrote “Now, a group of Rush scientists has become the first to demonstrate alpha-synuclein aggregation in biological tissue obtained before onset of motor symptoms of Parkinson’s disease.”
The team analyzed colonoscopy examination samples that had occurred two to five years before Parkinson’s signs and symptoms appeared in three subjects. In all three cases, alpha-synuclein aggregation had been detected in the samples taken from the wall of the lower intestine.
Shannon said:
“Recent clinical and pathological evidence supports the notion that Parkinson’s disease may begin in the intestinal wall then spread through the nerves to the brain. Clinical signs of intestinal disease, such as constipation, Parkinson’s disease diagnosis by more than a decade. These studies suggest it may one day be possible to use colonic tissue biopsy to predict who will develop motor Parkinson’s disease.
Such tissue could be obtained at the time of screening colonoscopy, a procedure routinely applied for colon cancer surveillance beginning at age 50, and repeated every three to 10 years in adults of middle age.”
For Parkinson’s to be properly diagnosed today, doctors rely on certain hallmark signs, such as gait problems, rigidity, slowed movement and tremor. Early on in the disease, clinical diagnosis can be hard. The authors say that from 10% to 20% of early Parkinson’s patients are probably misdiagnosed.
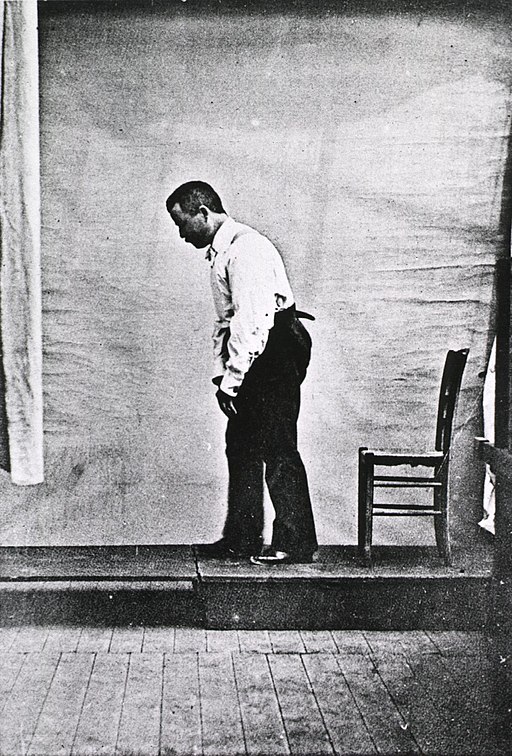
Doctors today rely on some hallmark Parkinson’s signs when making a diagnosis, such as an unusual gait
According to previous studies, in the majority of cases 60% to 80% of dopamine-producing cells in the brain are destroyed by the time primary Parkinson’s signs and symptoms start to appear.
The authors wrote:
“In view of a multi-billion-dollar translational research effort that aims to identify agents that slow or stop the progression of Parkinson’s disease, the need for accurate and timely diagnostic biomarkers, including the potential for pre-motor diagnosis, is particularly acute.
We believe that alpha-synuclein in the colonic submucosa may be a pre-motor biomarker that easily can be studied in cohorts at increased risk of developing Parkinson’s disease (relatives of Parkinson’s disease subjects, subjects with anosmia [inability to smell], rapid eye movement sleep behavior disorder and others).”
The authors emphasized that further studies are required in other populations, including cohort groups, as well as patients with other neurodegenerative disorders to replicate their findings and determine what the safest and most effective biomarker sites are.
Written by Christian Nordqvist