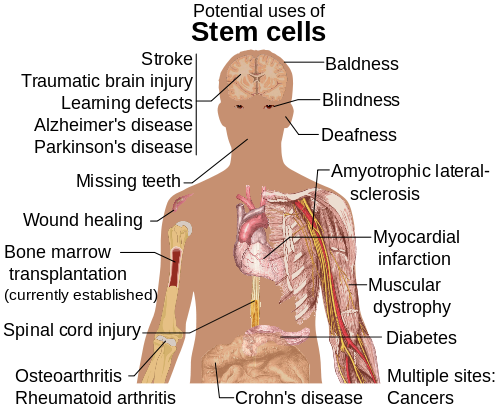
Science is probably overcoming a major milestone in patient-specific stem cell technology that will likely pave the way for cell-based therapies for life-threatening and/or chronic diseases, such as diabetes, Alzheimer’s, Parkinson’s, etc., scientists from NYSCF and Columbia University reported in the journal Nature.
Dieter Egli, Scott Noggle and team have derived embryonic stem cells from patients themselves by adding the nuclei of adult skin cells from diabetes type 1 patients to unfertilized donor oocytes. An oocyte is a female germ cell that is in the process of development – it is produced in the ovary by an oogonium (an ancestral cell) and gives rise to the egg (ovum) which can be fertilized. Put simply – an oocyte is an egg before maturation.
These patient-specific stem cells can be transplanted into the patient to replace diseased or damaged cells without being rejected by the person’s immune system. These cells look extremely promising for usage in cell-replacement medicine, the authors wrote excitedly. However, they stressed that further studies are necessary.
Senior scientist, Dr. Egli, said:
“The specialized cells of the adult human body have an insufficient ability to regenerate missing or damaged cells caused by many diseases and injuries. But if we can reprogram cells to a pluripotent state, they can give rise to the very cell types affected by disease, providing great potential to effectively treat and even cure these diseases. In this three-year study, we successfully reprogrammed skin cells to the pluripotent state.
Our hope is that we can eventually overcome the remaining hurdles and use patient-specific stem cells to treat and cure people who have diabetes and other diseases.”
NYSCF (New York Stem Cell Foundation) CEO Susan L. Solomon, said:
“The ultimate goal of this study is to save and enhance lives by finding better treatments and ventually cures for diabetes, Alzheimer’s, Parkinson’s and other debilitating diseases and injuries affecting millions of people across the US and the globe.
This research brings us an important step closer to creating new healthy cells for patients to replace their cells that are damaged or lost through injury.”
The researchers managed to transfer the nucleus from a patient’s adult skin cell into an oocyte without taking out the nucleus of that oocyte – this resulted in reprogramming of the adult nucleus to the pluripotent state. Pluripotent stem cells can divide and form cells indistinguishable from it – they can turn into virtually any kind of cell. They are also known as human embryonic stem cells.
In this study, embryonic stem cell lines where then derived from the oocyte containing the individual’s genetic material.
These pluripotent stem cells cannot be used for therapy on humans because they also have a copy of the oocyte chromosome – they have too many chromosomes. Future studies will work on engineering the stem cells so that they only have the patient’s DNA.
The scientists in this study reprogrammed the skin cells of patients with type 1 diabetes as well as healthy patients (control group) – and derived pluripotent stem cells. The pluripotent stem cells could, in theory, become insulin-producing beta cells. If this occurred, the patient with diabetes type 1 would be cured.
People with diabetes type 1 do not have beta cells, hence they cannot produce insulin.
Study collaborator, Rudolph L. Leibel, MD, co-director of Columbia’s Naomi Berrie Diabetes Center, said:
“This is an important step toward generating stem cells for disease modeling and drug discovery, as well as for ultimately creating patient-specific cell-replacement therapies for people with diabetes or other degenerative diseases or injuries.”
Robin Goland, MD, co-director of the Naomi Berrie Diabetes Center, said that this study could pave the way for the usage of somatic cell reprogramming to create stem cell banks which could be useful for patients with a wide range of diseases and conditions.
Goland said:
“In theory, stem cell lines could be matched to a particular patient, much as we do now when we screen an individual for compatibility with a kidney transplant.”
Co-author, Mark V. Sauer, MD, said:
“This project is a great example of how enormous strides can be achieved when investigators in basic science and clinical medicine collaborate. I feel fortunate to have been able to participate in this important project.”
Zach W. Hall, PhD, said:
“This work represents a major advance toward the production of patient-specific stem cells for therapeutic use by demonstrating that the nucleated oocyte has the ability to completely reprogram the nucleus of an adult human cell.”
Hall used to be Director of the National Institute of Neurological Disorders and Stroke, he was also President of the California Institute of Regenerative Medicine.
Written by Christian Nordqvist