While symptoms of rheumatoid arthritis (RA) typically affect the joints, it can also affect other parts of the body, such as the eyes, lungs, and heart.
Rheumatoid arthritis (RA) causes a person’s immune system to attack healthy tissue. Without treatment, RA can have wide-ranging effects.
RA affects the joints, but also the skin, brain, heart, and other areas. Meanwhile, medication for RA can also cause side effects throughout the body.
In this article, we look at the diverse range of changes associated with RA. We also describe the long-term effects of RA on the body and the likely outcomes.
RA is an autoimmune disease. Doctors also classify it as a systemic disease because it can have effects throughout the body.
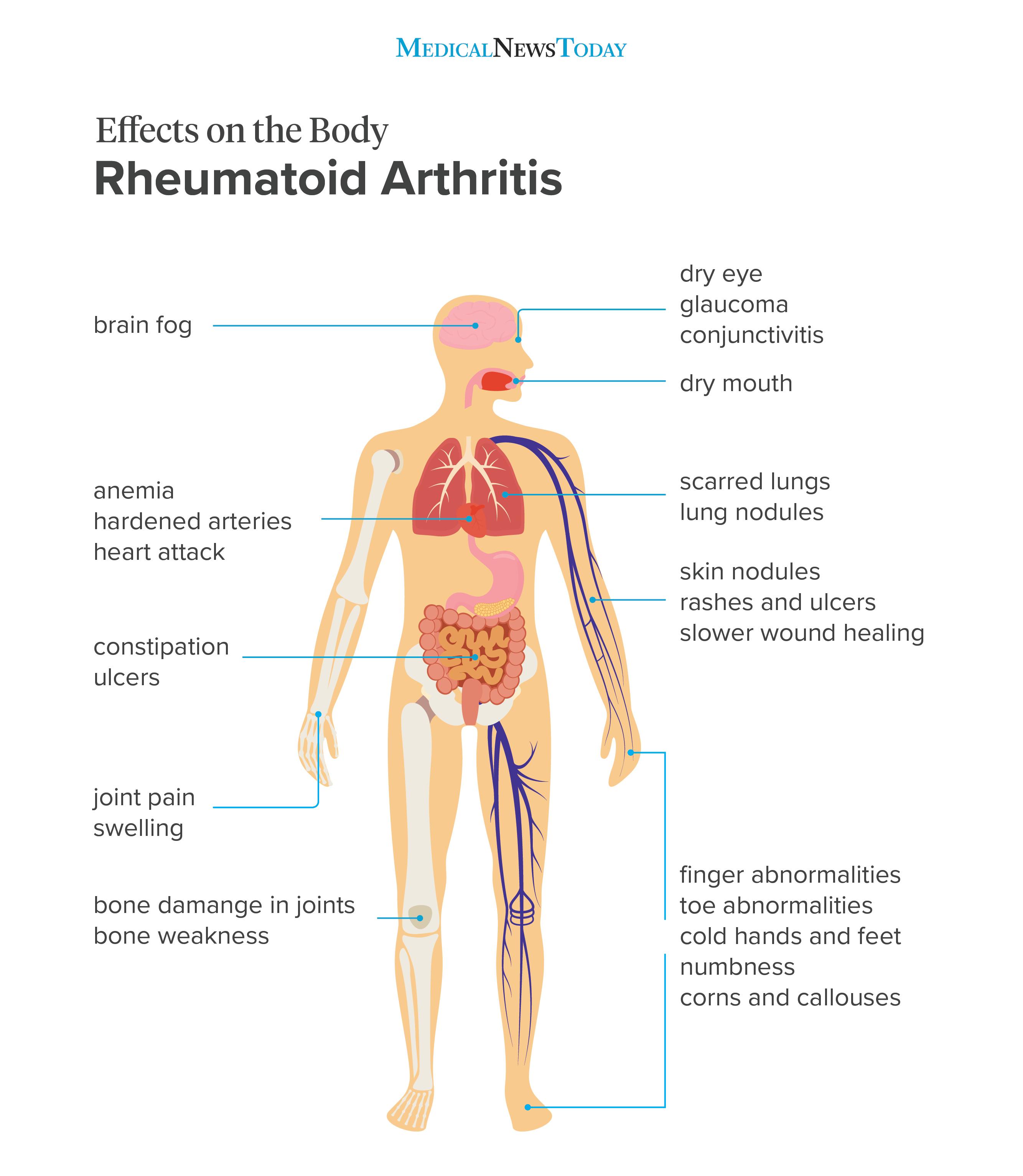
Image credit: Stephen Kelly, 2018
The joints
RA can affect almost any joint in the body, and it commonly develops in the fingers, hands, and feet. It usually affects the same joint on both sides, for example, both knees. RA does not affect the sacroiliac joints, which join the spine to the pelvis. In the spine, it only affects two joints in the neck.
The condition primarily targets the lining of the joints, called the synovium. In RA, the synovium becomes inflamed, swollen, and thick, due to cell proliferation. This it can lead to stiffness, pain, and a loss of mobility. Joint pain and stiffness in the morning can be an early sign of RA.
The skeleton
The joints contain cartilage, which prevents the bones in the joint from rubbing together. Over time, inflammation from RA can cause the cartilage to break down.
If the bones rub together, it can permanently damage the joint. This is a significant cause of pain and stiffness in people with advanced RA.
RA can also cause the bones to lose density, leading to osteoporosis, which involves the bones becoming thinner and more brittle. Research from 2020 describes osteoporosis as a common complication of RA and suggests that it may happen because similar immune and inflammatory features play a role in both conditions. A loss of bone increases the risk of breaks and fractures.
People who use corticosteroids to manage RA have a higher risk of developing osteoporosis, and so experts recommend using the lowest possible dosage.
The skin
Up to 20% of people with RA develop rheumatoid nodules near the joints and pressure points. These are small, firm bumps made of inflammatory tissue.
Rheumatoid nodules develop under the skin, over bony areas. While they are often painless and generally not a cause for concern, they can cause discomfort if a person places pressure on them, such as when kneeling. In some cases, infection and ulcers can occur. The most common places for nodules are the fingers and elbows, which people often rest on the arms of a chair.
RA can also cause inflammation in the skin, sometimes leading to:
- red patches
- swelling
- infection
- ulcers, in some cases
Ulceration in RA is usually a sign of vasculitis, which involves inflammation of the blood vessels. If ulcers develop, this could indicate that the person has more active disease affecting their whole system.
RA can also cause:
- thin, wrinkled skin that bruises easily
- dry skin
- discoloration of the palms of the hands
- brittleness, splitting, or thickening of the nails
- in rare cases, papules, nodules, plaques, lesions, and ulcers
Wounds may also take longer to heal in someone with RA. Many factors related to the disease, including vasculitis, can have this effect.
In addition, some RA medications can cause skin rashes.
The mouth
People with RA may experience xerostomia, or dry mouth.
Having RA increases the risk of developing Sjögren’s disease, which causes dryness in the eyes and mouth, among other symptoms. Like RA, Sjögren’s disease is an inflammatory autoimmune disorder.
RA can also cause saliva ducts to narrow or close, leading to an uncomfortable feeling of dryness and difficulty eating and swallowing. Chronic dry mouth can contribute to gingivitis and tooth decay.
The eyes
RA can also cause inflammation in the eyes, as well as dry eye syndrome, which can lead to ongoing irritation and eventually damage the cornea.
The effects of RA on the eyes can include:
- dry eyes, a feature of Sjögren’s
- scleritis, or inflammation of the whites of the eyes
- uveitis, or inflammation of the inner eye
- retinal vascular occlusion, or blocked blood vessels in the eye
- glaucoma, which damages the optic nerve
- cataracts, which results from inflammation in the optic lens
The lungs
In around 80% of people with RA, the disease affects the lungs. This may cause no symptoms, but prolonged inflammation in the lungs can lead to pulmonary fibrosis, which can cause scarring and breathing difficulties.
Rheumatoid nodules can also form in the lungs, though these are not usually a significant cause for concern.
Some RA medications can make the immune system less effective. This can make people more vulnerable to respiratory infections, including pneumonia and tuberculosis.
The heart
Inflammation from RA can damage the heart and blood vessels. In some cases, the consequences are life threatening.
RA can cause the following complications:
- Anemia: Inflammation can lead to low level of red blood cells, resulting in symptoms such as headaches and fatigue.
- Atherosclerosis:Chronic inflammation can damage the walls of the blood vessels. This can cause the body to absorb more cholesterol, which can cause plaque to build up inside the arteries.
- Heart attack or stroke:These can result if plaque builds up and blocks an artery or another blood vessel.
- Pericarditis: RA can cause inflammation in the lining of the heart, the pericardium, leading to chest pain.
The nerves
RA causes inflammation and swelling, and it can lead to peripheral neuropathy — nerve pain throughout the body. Symptoms include pain, numbness, and burning and tingling sensations. These may develop in the hands and feet.
According to some research, peripheral neuropathy may affect almost
When RA develops in the wrist, it can lead to carpal tunnel syndrome. This occurs when inflamed tissue in the wrist squeezes a nerve that extends from the forearm.
The feet
If RA affects the feet, it can limit the person’s mobility. Because the feet bear the weight of the body, the pain can become severe.
RA often develops in the joints of the toes and, less commonly, the ankles. The condition can also lead to:
- inflamed bursae, which are painful, fluid-filled sacs that appear on the balls of the feet
- nodules on the pad of the heel, the Achilles tendon, and other bony areas, at pressure points
- corns and calluses, patches of hard, thick skin that develop as the shape of the foot changes
- ulcers, if the person does not receive treatment
- nerve compression, when RA damages a joint
- circulatory problems, if inflammation in the blood vessels and joint damage block the flow of blood to the feet
If RA causes circulatory problems, their feet or toes may become numb easily or develop a bluish tinge.
The mind and brain
- depression
- problems with thinking and reasoning, including “brain fog“
- behavioral changes
These issues may occur:
- as side effects of RA medication
- in response to chronic pain
- as a result of blocked arteries in the brain
- due to a lack of exercise
- as a result of inflammation, which may be low-level
The
The kidneys and liver
Prescription medications for RA can cause complications, including liver and kidney damage. This can result from the long-term use of pain relief or anti-inflammatory medications.
RA is a progressive disease that usually worsens gradually, though medication can help slow its progress.
Over time, symptoms may become more severe or start to affect other joints or parts of the body if the treatment is not effective enough. For people with more advanced cases, surgery or joint replacements can help.
RA can be unpredictable. In the long term, people with RA may notice:
- changes in the severity and frequency of symptoms
- periods in which symptoms flare up, which can become more or less frequent
- periods of remission that vary in length
When RA progresses, symptoms occur more frequently, and pain often grows worse. Below are common indications that RA is progressing:
- pain and swelling increase
- pain and swelling occur more regularly
- other symptoms arise more frequently and last longer
- symptoms appear in new areas
- blood tests show higher levels of inflammatory markers and other biomarkers of RA
Anyone who notices new symptoms or symptoms that worsen or appear more frequently should contact a doctor.
People with RA often benefit from a tailored treatment plan. Guidelines published by the
What is the outlook for RA, and does it affect life expectancy?
RA is an inflammatory condition that causes pain and swelling in the joints and can also affect other areas, including the skin, eyes, brain, and cardiovascular system. It can increase the risk of other health problems, such as a heart attack or stroke.
Symptoms tend to fluctuate, worsening and improving periodically. Treatments can help manage the symptoms, slow the progression of the disease, and reduce the risk of permanent damage.
