Kevzara is a brand-name prescription medication. It’s used to treat moderate to severe rheumatoid arthritis (RA) in adults who have tried one or more disease modifying antirheumatic drugs (DMARDs). The DMARD must not have worked for them, or they had to have had a reaction to the medication.
RA is a condition in which your immune system (your body’s defense against infection) mistakenly attacks your joints.
Drug details
Kevzara contains the drug sarilumab, which belongs to a class of drugs called monoclonal antibodies. (A class of drugs is a group of medications that work in a similar way.)
Kevzara is available as a prefilled syringe and a prefilled pen. The drug is given as an injection just under your skin (subcutaneous). A healthcare professional may show you or your caregiver how to give injections at home.
Effectiveness
In a clinical study, people with RA took 200 mg of Kevzara with another drug called methotrexate (Trexall) or a placebo (no active drug) and methotrexate. After 16 weeks, 57.4% of people who took Kevzara and methotrexate had an improvement in their physical function (ability to move). In comparison, 42.5% of people who took a placebo and methotrexate had an improvement in movement.
FDA approval
In 2017, the Food and Drug Administration (FDA) approved Kevzara to treat RA.
Kevzara is available only as a brand-name medication. It contains the active drug sarilumab.
Kevzara isn’t currently available in biosimilar form.
A biosimilar is a medication that’s similar to a brand-name drug. A generic medication, on the other hand, is an exact copy of a brand-name drug. Biosimilars are based on biologic medications, which are made from living sources such as proteins or DNA. Generics are based on regular medications, which are made from chemicals. Biosimilars and generics also usually cost less than brand-name drugs.
Kevzara can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Kevzara. These lists don’t include all possible side effects.
For more information on the possible side effects of Kevzara, talk with your doctor or pharmacist. They can give you tips on how to deal with any side effects that may be bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs it has approved. If you would like to report to the FDA a side effect you’ve had with Kevzara, you can do so through MedWatch.
More common side effects
The more common side effects of Kevzara can include:
- redness, rash, or itching at the injection site
- upper respiratory infections, such as a cold
- urinary tract infections
- increased levels of cholesterol or triglycerides (a type of fat)
Most of these side effects may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk with your doctor or pharmacist.
Serious side effects
Serious side effects from Kevzara aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include the following:
- Blood disorders, such as neutropenia (decreased levels of white blood cells) or thrombocytopenia (decreased levels of platelets, a type of blood cell that helps blood clot). Symptoms can include:
- fever
- diarrhea
- shortness of breath
- belly pain
- bleeding easily
- Increases in levels of liver enzymes (a type of protein). Symptoms can include:
- yellow tint to your skin or the whites of your eyes
- belly pain
- nausea
- vomiting
- feeling tired
- Gastrointestinal perforations (tears in the lining of your intestines or stomach). Symptoms can include:
- fever
- severe belly pain
- chills
- nausea
- vomiting
- Certain types of cancer, such as skin cancer or lymphoma. Symptoms can include:
- feeling tired
- fever
- unexplained weight loss
- swollen lymph nodes (swelling or lumps in your neck or armpits)
Other serious side effects, explained in more detail below in “Side effect details,” include:
- allergic reactions
- serious infections* such as tuberculosis (TB)
* Kevzara has a
Side effect details
You may wonder how often certain side effects occur with this drug, or whether certain side effects pertain to it. Here’s some detail on several of the side effects this drug may or may not cause.
Allergic reaction
As with most drugs, some people can have an allergic reaction after taking Kevzara. Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (warmth and redness in your skin)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
Call your doctor right away if you have a severe allergic reaction to Kevzara. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency.
In clinical trials, there were some reports of allergic reactions. About 0.3% of people who took Kevzara stopped treatment because of allergic reactions. No one in the placebo (no treatment) study stopped treatment because of an allergic reaction.
Rash
It’s possible to develop a rash at the injection site after a Kevzara injection. In clinical studies, about 4% of people who took 200 mg of Kevzara along with a disease modifying antirheumatic drug (DMARD) had redness at the injection site. In comparison, about 0.9% of people who took a placebo (no active drug) with a DMARD had redness.
If you develop a rash that’s bothersome to you, talk with your doctor about ways to treat it. Sometimes a rash can be a sign of an allergic reaction. If your rash gets worse or if you have other symptoms with your rash, such as trouble breathing, see your doctor right away.
Injection site reactions
A reaction at the site of a Kevzara injection can occur. A reaction can include redness or itching. In clinical trials, about 7% of people who received 200 mg of Kevzara had an injection site reaction. In comparison, only 1% of people who received a placebo had an injection site reaction.
Most of the reactions were mild. Only 0.2% of people stopped taking Kevzara in clinical trials because of reactions at the injection site. It’s not known if anyone in the placebo (no treatment) group stopped taking the medication because of injection site reactions.
If you have an injection site reaction that’s bothersome to you, talk with your doctor or pharmacist. They can suggest ways to help ease your symptoms.
Blood disorders
Certain blood disorders may occur while taking Kevzara.
Neutropenia
One of these disorders is neutropenia, which is a decrease in the level of neutrophils. Neutrophils are a type of white blood cell that help you fight infections. When you have a low level of neutrophils, you may have a higher risk for infections.
In clinical trials, 6% of people who took 200 mg of Kevzara had a decrease in neutrophil levels less than 1,000/mm3. In comparison, no one who took a placebo had a decrease in neutrophil levels less than 1,000/mm3. However, the decreased levels of neutrophils in people who took Kevzara weren’t linked to an increased risk of infections.
Before you start taking Kevzara, your doctor will do some blood tests to check your neutrophil counts. They’ll check your blood again 4 to 8 weeks after you start Kevzara treatment and then every 3 months after that. Based on your levels, your doctor may change your dose of Kevzara.
Thrombocytopenia
Another blood disorder that may occur while taking Kevzara is thrombocytopenia, a decrease in the level of platelets. Platelets are blood cells that help clot your blood so that you stop bleeding.
In clinical trials of people who took 200 mg of Kevzara, 1% had platelet counts less than 100,000/mm3. In comparison, no one who took a placebo had a decrease in their platelet count less than 100,000/mm3. However, the decreased platelet counts in people who took Kevzara wasn’t linked to an increased risk of bleeding.
Before you start to take Kevzara, your doctor will test your platelet levels. They’ll check your levels again 4 to 8 weeks after you start taking Kevzara, and then every 3 months after that. Your doctor may change your dose of Kevzara based on your platelet levels.
Serious infections
Serious infections* have occurred in people who took Kevzara. These infections included ones caused by bacteria, viruses, and fungi. Some infections required people to go to the hospital or led to death.
In clinical trials, the most common types of serious infections were pneumonia, which affects the lungs, and a skin infection called cellulitis.
In the studies, the rate of serious infections of people who took 200 mg of Kevzara with a DMARD was 3.8 serious infections per 100 patient years. This means that if 100 people took Kevzara for 1 year, about four of them would develop a serious infection. In comparison, the rate of serious infections in people who took a placebo with a DMARD was 2.5 serious infections per 100 patient years.
Symptoms of a serious infection can include:
- fever or chills
- muscle aches
- weight loss
- painful or warm skin sores
- diarrhea
- burning when you urinate
- trouble breathing
- spitting up blood
- feeling tired
If you have any signs of infection, such as fever or trouble breathing, it’s very important that you call your doctor right away. They may have you stop taking Kevzara until your infection clears up.
* Kevzara has a
Weight gain (not a side effect)
Weight gain isn’t a side effect that was seen in clinical trials of Kevzara. However, people with rheumatoid arthritis (RA) may have more trouble staying at a steady weight. RA may make it harder for you to move and exercise. RA may also make you more tired, so that you don’t feel like exercising.
If you’re taking prednisone (Deltasone) for your RA, that drug may cause weight gain as well. Prednisone can increase your appetite, making you want to eat more food.
If you gain weight, talk with your doctor about what may be causing it and how to prevent it.
As with all medications, the cost of Kevzara can vary. The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
Your insurance company may require you to get prior authorization before they approve coverage for Kevzara. This means that your doctor will need to send a request to your insurance company asking them to cover the drug. The insurance company will review the request and let you and your doctor know if your plan will cover Kevzara.
If you’re not sure if you’ll need to get prior authorization for Kevzara, contact your insurance company.
Financial and insurance assistance
If you need financial support to pay for Kevzara, or if you need help understanding your insurance coverage, help is available.
Sanofi-Aventis U.S. LLC, the manufacturer of Kevzara, offers the KevzaraConnect Copay Card. KevzaraConnect nurse educators may also be able to help. For more information and to find out if you’re eligible for support, call 844-538-9272 or visit the program website.
The Kevzara dosage your doctor prescribes will depend on several factors. These include:
- whether you have side effects from Kevzara
- other medical conditions you may have
Typically, your doctor will start you on a low dosage. Then they’ll adjust it over time to reach the amount that’s right for you. Your doctor will ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to suit your needs.
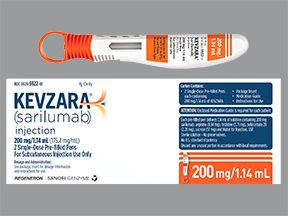
Drug forms and strengths
Kevzara is given as an injection just under your skin (subcutaneous). A healthcare professional will give you your first dose. After that, they can show you or your caregiver how to give injections at home.
Kevzara is available as a prefilled syringe and a prefilled pen. It may be easier for you to use one form over the other, so ask your doctor which form is best for you. Both the syringe and pen come in two strengths: 150 mg/1.14 mL or 200 mg/1.14 mL.
Kevzara may be used by itself or with a disease modifying antirheumatic drug (DMARD), such as methotrexate.
Dosage for rheumatoid arthritis
The recommended dosage of Kevzara for rheumatoid arthritis (RA) is one 200-mg injection every 2 weeks.
Your doctor may change your dose in some situations, such as if you:
- have neutropenia, which is a decreased level of white blood cells
- have thrombocytopenia, a condition in which you have a decreased level of platelets (a type of blood cell that helps blood clot)
- have an increase in your levels of liver enzymes (a type of protein)
- develop an infection* while you’re taking Kevzara
* Kevzara has a
What if I miss a dose?
If you miss your dose of Kevzara, take it as soon as you remember, as long as it’s not almost time for your next dose. If you miss your dose, ask your doctor when you should have your next injection.
To help make sure that you don’t miss a dose, try setting a reminder on your phone. You can also put your injection schedule in a calendar.
Will I need to use this drug long term?
Kevzara is meant to be used as a long-term treatment for your RA. If you and your doctor determine that Kevzara is safe and effective for you, you’ll likely take it long term.
The Food and Drug Administration (FDA) approves prescription drugs such as Kevzara to treat certain conditions.
Kevzara is approved by the FDA to treat moderate to severe rheumatoid arthritis (RA) in adults. Kevzara should be used only after the person has tried at least one disease modifying antirheumatic drug (DMARD). The DMARD must not have worked for them or they had to have had a reaction to the medication.
Sometimes Kevzara is used by itself for RA. Other times Kevzara can be taken along with disease modifying antirheumatic drugs (DMARDs), such as methotrexate (Trexall).
RA is a condition in which your immune system attacks your joints. (Your immune system is your body’s defense against infection.) RA usually causes swelling and pain in your hands, wrists, and feet. The condition may also affect your shoulders, elbows, knees, and ankles. According to the Arthritis Foundation, about 1.5 million people in the United States are living with RA.
Effectiveness for rheumatoid arthritis
In a clinical study, people with RA took 200 mg of Kevzara with another drug called methotrexate (Trexall) or a placebo (no active drug) and methotrexate. After 16 weeks, 57.4% of people who took Kevzara and methotrexate had an improvement in their physical function (ability to move). In comparison, 42.5% of people who took a placebo and methotrexate had an improvement in movement.
After 1 year of clinical trials, 55.6% of people who took 200 mg of Kevzara with methotrexate had no worsening of joint damage. (Joint damage can often occur with RA.) In comparison, 38.7% of people who took a placebo along with methotrexate had no worsening of joint damage.
Other drugs are available that can treat rheumatoid arthritis (RA). Some may be better suited for you than others. If you’re interested in finding an alternative to Kevzara, talk with your doctor. They can tell you about other medications that may work well for you.
Note: Some of the drugs listed here are used off-label to treat these specific conditions. Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.
Alternatives for rheumatoid arthritis
Examples of other drugs that may be used to treat RA include:
- hydroxychloroquine (Plaquenil)
- leflunomide (Arava)
- methotrexate (Trexall)
- sulfasalazine (Azulfidine)
- azathioprine (Imuran)
- adalimumab (Humira)
- tocilizumab (Actemra)
- etanercept (Enbrel)
- infliximab (Remicade)
- certolizumab (Cimzia)
- abatacept (Orencia)
- anakinra (Kineret)
- golimumab (Simponi)
- rituximab (Rituxan)
- tofacitinib (Xeljanz)
You may wonder how Kevzara compares to other medications that are prescribed for similar uses. Here we look at how Kevzara and Actemra are alike and different.
Kevzara contains the drug sarilumab. Actemra contains the drug tocilizumab.
Uses
The Food and Drug Administration (FDA) has approved Kevzara for use in adults with moderate to severe rheumatoid arthritis (RA). Kevzara should be used only after the person has tried at least one disease modifying antirheumatic drug (DMARD). The DMARD must not have worked for them, or they had to have had a reaction to the medication.
Actemra is also FDA-approved for use in adults with moderate to severe RA. Like Kevzara, Actemra is approved for use in people who have already tried at least one DMARD. The DMARD must not have worked for them, or they had to have had a reaction to the medication.
In addition, Actemra is approved to treat the following conditions:
- giant cell arteritis in adults
- chimeric antigen receptor (CAR) T-cell-induced severe (or life-threatening) cytokine release syndrome in adults and children ages 2 years and older
- polyarticular juvenile idiopathic arthritis in children age 2 years and older
- systemic juvenile idiopathic arthritis in children ages 2 years and older
Drug forms and administration
Here’s some information about the forms of each drug and how you take them.
Kevzara
Kevzara is given as an injection just under your skin (subcutaneous) once every 2 weeks. A healthcare professional may show you or your caregiver how to give injections at home.
Kevzara is available as a prefilled syringe and a prefilled pen. Both the syringe and pen come in two strengths: 150 mg/1.14 mL or 200 mg/1.14 mL.
Kevzara can be used by itself or with a disease modifying antirheumatic drug (DMARD), such as methotrexate.
Actemra
Actemra can be given in two different ways. The medication can be given as an intravenous (IV) infusion by a healthcare professional in a doctor’s office or a clinic. (An IV infusion is an injection into your vein that’s given over a period of time.) Actemra infusions take about 60 minutes and are given every 4 weeks.
Actemra can also be given as an injection under the skin. These injections are given once every week or every other week. The dosage depends on your weight and how your body responds to the medication. A healthcare professional will give you your first dose. After that, they can show you or your caregiver how to give injections at home.
Actemra is available in three forms:
- a vial of solution given as an IV infusion, which comes in three strengths: 80 mg/4mL, 200 mg/10 mL, and 400 mg/20 mL
- a prefilled single-use syringe that comes in one strength: 162 mg/0.9 mL
- a prefilled single-use autoinjector that comes in one strength: 162 mg/0.9 mL
Like Kevzara, Actemra can be used alone or with a DMARD medication, such as methotrexate.
Side effects and risks
Kevzara and Actemra both contain medications to treat RA. Therefore, both medications can cause very similar side effects. Below are examples of these side effects.
More common side effects
These lists contain examples of more common side effects that can occur with Kevzara, with Actemra, or with both drugs (when taken individually).
- Can occur with Kevzara:
- Can occur with Actemra:
- headache
- increased blood pressure
- Can occur with both Kevzara and Actemra:
- increased levels of cholesterol or triglycerides (a type of fat)
- upper respiratory infections, such as a cold
- redness, rash, or itching at the injection site
Serious side effects
These lists contain examples of serious side effects that can occur with Kevzara, with Actemra, or with both drugs (when taken individually).
- Can occur with Kevzara:
- few unique serious side effects
- Can occur with Actemra:
- nerve disorders, such as multiple sclerosis or demyelinating polyneuropathy
- serious liver injury
- Can occur with both Kevzara and Actemra:
- serious infections* such as tuberculosis (TB)
- gastrointestinal perforations (tears in the lining of your intestines or stomach)
- increases in levels of liver enzymes (a type of protein)
- blood disorders, such as neutropenia (decreased levels of white blood cells) or thrombocytopenia (decreased levels of platelets, a type of blood cell that helps blood clot)
- allergic reactions
- certain types of cancer, such as lymphoma or skin cancer
* Kevzara has a
Effectiveness
Kevzara and Actemra have different FDA-approved uses, but they’re both used to treat moderate to severe RA in adults who have already tried at least one other DMARD.
Separate studies of the two drugs were compared in a larger review of studies. Researchers looked at how effective Kevzara and Actemra are.The comparison showed that Actemra used alone or with methotrexate was more likely to ease RA symptoms when compared to Kevzara.
Costs
Kevzara and Actemra are both brand-name drugs. There are currently no biosimilar forms of either drug. Brand-name medications usually cost more than biosimilars.
A biosimilar is a medication that’s similar to a brand-name drug. A generic medication, on the other hand, is an exact copy of a brand-name drug. Biosimilars are based on biologic medications, which are made from living sources such as proteins or DNA. Generics are based on regular medications, which are made from chemicals. Biosimilars and generics also usually cost less than brand-name drugs.
Kevzara generally costs less than Actemra. The actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
Like Actemra (above), the drug Humira has uses similar to those of Kevzara. Here’s a comparison of how Kevzara and Humira are alike and different.
Kevzara contains the drug sarilumab. Humira contains the drug adalimumab.
Uses
The Food and Drug Administration (FDA) has approved Kevzara for use in adults with moderate to severe rheumatoid arthritis (RA). Kevzara should be used only after the person has tried at least one disease modifying antirheumatic drug (DMARD). The DMARD must not have worked for them, or they had to have had a reaction to the medication.
Humira is FDA-approved to be used in people with moderate to severe RA. Humira is also approved to treat the following conditions:
- juvenile idiopathic arthritis in children ages 2 years and older
- psoriatic arthritis in adults
- ankylosing spondylitis in adults
- Crohn’s disease in adults as well as children ages 6 years and older
- ulcerative colitis in adults
- plaque psoriasis in adults
- hidradenitis suppurativa in adults as well as children ages 12 years and older
- uveitis in adults as well as children ages 2 years and older
Drug forms and administration
Here’s some information about the forms of each drug and how you take them.
Kevzara
Kevzara is given as an injection just under your skin (subcutaneous) once every 2 weeks. A healthcare professional may show you or your caregiver how to give injections at home.
Kevzara is available as a prefilled syringe and a prefilled pen. Both the syringe and pen come in two strengths: 150 mg/1.14 mL or 200 mg/1.14 mL.
Kevzara can be used by itself or with a DMARD, such as methotrexate.
Humira
Humira is also given as an injection under your skin. To treat RA, you’d usually get one injection every 2 weeks. Sometimes, depending on your response to the medication, Humira may be given once every week.
Humira is available in three forms:
- a single-use prefilled syringe in 10-mg, 20-mg, 40-mg, and 80-mg strengths
- a single-use prefilled pen in 40-mg and 80-mg strengths
- a single-use vial (given as an injection only by a healthcare professional) in a 40-mg strength
Humira can also be used by itself or with a DMARD, such as methotrexate.
Side effects and risks
Kevzara and Humira both contain medications to treat RA. Therefore, both medications can cause very similar side effects. Below are examples of these side effects.
More common side effects
These lists contain examples of more common side effects that can occur with Kevzara, with Humira, or with both drugs (when taken individually).
- Can occur with Kevzara:
- few unique serious side effects
- Can occur with Humira:
- nausea
- headache
- Can occur with both Kevzara and Humira:
- upper respiratory infections, such as a cold
- increased levels of cholesterol or triglycerides (a type of fat)
- redness, rash, or itching at the injection site
Serious side effects
These lists contain examples of serious side effects that can occur with Kevzara, with Humira, or with both drugs (when taken individually).
- Can occur with Kevzara:
- gastrointestinal perforations (tears in the lining of your intestines or stomach)
- Can occur with Humira:
- reactivation of hepatitis B virus, which means if you’ve had hepatitis B in the past, the virus could become active again
- nerve-related diseases, such as multiple sclerosis or optic neuritis
- anemia (decreased number of red blood cells)
- Can occur with both Kevzara and Humira:
- serious infections* such as tuberculosis (TB)
- certain types of cancer, such as lymphoma or skin cancer
- allergic reactions
- blood disorders, such as neutropenia (decreased levels of white blood cells) or thrombocytopenia (decreased levels of platelets, a type of blood cell that helps blood clot)
- increases in levels of liver enzymes (a type of protein)
* Kevzara has a
Effectiveness
Kevzara and Humira have different FDA-approved uses, but they’re both used to treat RA.
Kevzara and Humira were directly compared in a
In this study, Kevzara was more effective than Humira at easing RA symptoms. In the group who took Kevzara, 71.7% of people had RA that responded to treatment. “Response” meant that their RA symptoms eased by at least 20%. In the group who took Humira, 58.4% of people responded to treatment.
Costs
Kevzara and Humira are both brand-name drugs. Kevzara isn’t currently available in biosimilar form. But Humira has four biosimilars: Cyltezo, Amjevita, Hyrimoz, and Hadlima. They may cost less than Kevzara and Humira.
A biosimilar is a medication that’s similar to a brand-name drug. A generic medication, on the other hand, is an exact copy of a brand-name drug. Biosimilars are based on biologic medications, which are made from living sources such as proteins or DNA. Generics are based on regular medications, which are made from chemicals. Biosimilars and generics also usually cost less than brand-name drugs.
Kevzara generally costs less than Humira. The actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
Here are answers to some frequently asked questions about Kevzara.
Can I take Kevzara with another biologic drug for RA?
No, it’s not recommended. Although Kevzara hasn’t been studied with other biologic drugs, you should avoid using Kevzara with other biologic medications for RA. A biologic is a drug that’s made from living sources such as proteins or DNA. Kevzara itself is biologic.
Many biologics can weaken your immune system and increase your risk for infection. (Your immune system is your body’s defense against infections.) So by taking two biologics, your risk for serious infections* increases even more.
Other types of biologic drugs used for RA include a group of medications called tumor necrosis factor (TNF) blockers. These drugs block a protein called TNF, causing a decrease in inflammation (swelling). Examples of TNF blockers that you should avoid while taking Kevzara include:
- adalimumab (Humira)
- etanercept (Enbrel)
- infliximab (Remicade)
- golimumab (Simponi)
If you’re taking a biologic drug or aren’t sure, talk with your doctor before using Kevzara.
* Kevzara has a
Can Kevzara cause hair loss?
Hair loss isn’t a side effect that was seen in clinical trials of people taking Kevzara. However, hair loss may be connected to other medications that are used to treat rheumatoid arthritis (RA).
Certain medications used for RA can cause hair loss, especially methotrexate. Methotrexate helps decrease inflammation (swelling) by stopping cells from growing as quickly. These cells can include ones in your hair follicles (sacs under your skin that hold the roots of your hair). If these cells stop growing, your hair may fall out. According to the Arthritis Foundation, hair loss occurs in 1% to 3% of people who take methotrexate.
Methotrexate can also decrease the level of folic acid in your body. Folic acid helps keep your hair healthy.
So if you’re using methotrexate along with Kevzara, methotrexate may be the cause of your hair loss. Other medications for RA that can cause hair loss include leflunomide (Arava), etanercept (Enbrel), and adalimumab (Humira).
If you’re concerned about hair loss or how to prevent it while taking Kevzara, talk with your doctor.
How can I prevent infections while taking Kevzara?
Kevzara can weaken your immune system and decrease your body’s ability to fight infections.* That’s why it’s so important to work to prevent infections while taking the drug.
The best way to prevent infection is by washing your hands often with soap and water. You also should try to stay away from people who are currently sick, even with a cold. Catching their germs can make you ill. You should avoid eating any raw eggs, cheese, or meat as well. Any bacteria in the raw food may also make you sick.
Symptoms of infection can include:
- fever
- diarrhea
- cough
- trouble breathing
- burning when you urinate
If you notice any of these symptoms, talk with your doctor right away. The faster you start treating an infection, the easier your body can fight it.
* Kevzara has a
Will I need any tests before and during my Kevzara treatment?
Before you start taking Kevzara, your doctor will give you some tests to make sure the medication is safe for you. For example, you’ll be tested for the lung disease tuberculosis (TB). If your test comes back positive, you’ll be treated for TB before you take Kevzara.
Your doctor will also do blood tests. Kevzara can decrease the levels of neutrophils, a type of white blood cell, and platelets, a type of blood cell that helps blood clot. Kevzara can also increase your levels of liver enzymes (a type of protein). Your doctor will check all these levels.
You’ll also have blood testing done while you’re taking Kevzara. This helps makes sure that the medication doesn’t decrease your neutrophils or platelets to unsafe levels. In addition, your doctor will check that your liver enzyme levels aren’t too high.
You’ll have blood tests before your first dose of Kevzara, and then 4 to 8 weeks after your first dose. After that, you’ll have blood tests once every 3 months to monitor your levels. If levels change too much, your doctor may decrease your dose of Kevzara or have you stop taking the medication.
Should I avoid any vaccines while taking Kevzara?
You shouldn’t get any live vaccines while you’re taking Kevzara. Live vaccines contain weakened pieces of a virus. This helps your body build up an immunity to (defense against) the virus. However, taking Kevzara may weaken your immune system. This means that your body may not be strong enough to fight the weakened virus in the vaccine, so you could become sick.
Examples of live vaccines that should be avoided while you’re taking Kevzara include:
- measles, mumps, rubella (MMR)
- intranasal flu (nasal spray version of the flu vaccine)
- smallpox
- chickenpox
- rotavirus
- yellow fever
- certain typhoid vaccines
Before you take Kevzara, ask your doctor if you’re up-to-date on your vaccines. Your doctor may recommend that you get any live vaccines before you start treatment with Kevzara.
However, inactive vaccines, such as a flu shot, are generally safe to get while you’re taking Kevzara. But be sure to talk with your doctor before getting any vaccines during your Kevzara treatment.
You should take Kevzara according to your doctor’s or another healthcare professional’s instructions.
Kevzara is available as a prefilled pen or prefilled syringe that you use only one time. (You should never reuse a pen or syringe.) It may be easier for you to use one form, so ask your doctor which form is best for you.
The drug is administered as an injection just under your skin (subcutaneous). A healthcare professional may show you or your caregiver how to give Kevzara injections at home. This way, you won’t have to go to your doctor’s office for your injections.
The Kevzara website has helpful step-by-step videos that show how to inject your Kevzara.
When to take
Usually, you’ll have a Kevzara injection once every 2 weeks. Be sure to take the rest of your doses on the same day of the week, at the same time. For example, if you have your first dose on a Monday morning, you should take your next dose in 2 weeks on Monday morning.
To help make sure that you don’t miss a dose, try setting a reminder on your phone. You can also put your injection schedule in a calendar.
There are no known interactions between Kevzara and alcohol. But some studies have shown that alcohol may make rheumatoid arthritis (RA) worse, especially in women. If you drink alcohol, talk with your doctor. They can tell you how much is safe for you to drink during your Kevzara treatment.
Also, keep in mind that you shouldn’t consume alcohol and use other medications that treat RA. These include methotrexate (Trexall), nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil) or naproxen (Aleve), and acetaminophen (Tylenol). If you’re taking any of these medications, talk with your doctor before drinking alcohol. Some of these drugs can interact with alcohol and cause serious side effects such as liver damage or bleeding in the stomach.
Kevzara can interact with several other medications. It’s not known to interact with supplements or foods.
Different interactions can cause different effects. For instance, some interactions can interfere with how well a drug works. Other interactions can increase the number of side effects or make them more severe.
Kevzara and other medications
Below is a list of medications that can interact with Kevzara. This list doesn’t contain all drugs that may interact with Kevzara.
Before taking Kevzara, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Kevzara and theophylline or aminophylline
Kevzara can decrease the level of the drugs theophylline (Theochron) and aminophylline (Norphyl) in your body. This means that theophylline or aminophylline may not work as well. Your doctor may monitor your levels of medication by doing a blood test. Based on the results, your doctor may increase your dose of theophylline or aminophylline.
Kevzara may still affect your theophylline or aminophylline levels for several weeks after you stop taking Kevzara.
If you’re taking theophylline or aminophylline, talk with your doctor before taking Kevzara.
Kevzara and warfarin
Kevzara can decrease the level of warfarin (Coumadin) in your body. This can make the warfarin less effective. Your doctor will do extra blood testing to see how well warfarin is working for you. Depending on the results of your blood tests, your doctor may increase your dose of warfarin.
After you stop taking Kevzara, your level of warfarin may be affected for several weeks.
If you’re taking warfarin, it’s important to talk with your doctor before using Kevzara.
Kevzara and oral contraceptives
Kevzara can make your oral contraceptive medication less effective. This means that your birth control may not work as well or at all. Kevzara may also prevent your oral contraceptive from working for several weeks after you stop taking Kevzara.
Examples of some common oral contraceptive medications include:
- levonorgestrel/ethinyl estradiol (Lessina, Levora, Seasonique)
- desogestrel/ethinyl estradiol (Apri, Kariva)
- norethindrone/ethinyl estradiol (Balziva, Junel, Loestrin, Loestrin Fe, Microgestin, Microgestin Fe)
- norgestrel (Ovrette)
- norgestrel/ethinyl estradiol (Cryselle, Lo/Ovral)
- drospirenone/ethinyl estradiol (Loryna, Yaz)
- norgestimate/ethinyl estradiol (Ortho Tri-Cyclen, Ortho Tri-Cyclen Lo, Sprintec, Tri-Sprintec, TriNessa)
- mestranol/norethindrone (Ortho-Novum 1/50)
- norethindrone (Micronor)
If you take an oral contraceptive medication, talk with your doctor or pharmacist before taking Kevzara.
Kevzara and certain cholesterol medications
Kevzara can make your cholesterol medications less effective. If you’re taking a statin medication for your cholesterol along with Kevzara, the statin medication may not work as well. Kevzara may stop your cholesterol medication from working for several weeks even after you stop taking Kevzara.
Examples of statin medications include:
- atorvastatin (Lipitor)
- fluvastatin (Lescol)
- lovastatin (Mevacor)
- simvastatin (Zocor)
Clinical trials looked at people who took Kevzara and simvastatin. One week after having a Kevzara injection, people’s levels of simvastatin decreased by about 45%. This decrease could make simvastatin much less effective in lowering cholesterol levels.
If you take a statin medication for your cholesterol, talk with your doctor before taking Kevzara.
Kevzara and other monoclonal antibodies
Kevzara belongs to a class of drugs called biologics. (A class of drugs is a group of medications that work in a similar way.) Biologics are drugs made from living sources such as proteins or DNA. Specifically, Kevzara is a type of biologic called a monoclonal antibody. Monoclonal antibodies decrease the amount of inflammation (swelling) in the joints of people with rheumatoid arthritis (RA). However, monoclonal antibodies may also weaken your immune system. Your immune system is your body’s defense against infection.
If you’re taking multiple monoclonal antibodies at once, your immune system can be even more weak. The side effects of the medications may add up and make you sick. You’d be at an increased risk for infection* and other side effects caused by the medications. Examples of monoclonal antibodies include:
- adalimumab (Humira)
- etanercept (Enbrel)
- golimumab (Simponi)
- infliximab (Remicade)
- rituximab (Rituxan)
Researchers haven’t really studied the use of these medications together. So it’s best to avoid taking multiple monoclonal antibodies at one time because of the increased risk of side effects. If you’re already taking a monoclonal antibody, talk with your doctor about how to switch to Kevzara or which medication is best for you.
* Kevzara has a
Kevzara and live vaccines
You shouldn’t get any live vaccines while you’re taking Kevzara.
Live vaccines contain weakened pieces of a virus. This helps your body build up an immunity to (defense against) the virus. However, taking Kevzara may weaken your immune system. This means that your body may not be strong enough to fight the weakened virus in the vaccine, so you could become sick.
Live vaccines that you should avoid while you’re taking Kevzara include:
- measles, mumps, rubella (MMR)
- intranasal flu (nasal spray version of the flu vaccine)
- smallpox
- chickenpox
- rotavirus
- yellow fever
- certain typhoid vaccines
Talk with your doctor about what live vaccines you may need before taking Kevzara. They can help make sure that you’re caught up on your vaccines before beginning treatment.
Kevzara and herbs and supplements
There aren’t any herbs or supplements that have been specifically reported to interact with Kevzara. However, you should still check with your doctor or pharmacist before using any of these products while taking Kevzara.
Kevzara can be used along with other medications that treat rheumatoid arthritis (RA) called disease modifying antirheumatic drugs (DMARDs).
One such DMARD is methotrexate (Trexall). Usually, you’ll start taking methotrexate or a different DMARD first. If these medications aren’t effective enough alone, your doctor may add Kevzara to your treatment plan. Other examples of DMARDs include:
- azathioprine (Imuran)
- hydroxychloroquine (Plaquenil)
- leflunomide (Arava)
- sulfasalazine (Azulfidine)
Rheumatoid arthritis (RA) is a condition in which your immune system attacks your joints and can make it hard for you to move them. (Your immune system is your body’s defense against infection.) Specifically, your immune system attacks the synovium, which is the lining of your joints.
With RA, your joints can become swollen, painful, and stiff. RA usually affects your hands, wrists, and feet. But it may also affect your shoulders, elbows, knees, or ankles. Over time, untreated RA can cause your joints to become deformed.
Kevzara is a type of medication called a monoclonal antibody. Monoclonal antibodies work by binding to a specific protein in your body. This process stops your immune system from damaging your joints. Kevzara works by binding to a protein called interleukin-6 (IL-6). IL-6 causes swelling and joint pain in people with RA. Once Kevzara binds to IL-6, the drug stops IL-6 from working. This leads to less joint pain and swelling in people with RA.
How long does it take to work?
In some people, Kevzara may start working within the first 2 weeks of treatment. However, other people may take up to 3 months to see any changes due to Kevzara.
It’s not known if Kevzara is safe to take during pregnancy. Kevzara is a type of medication called a monoclonal antibody. Monoclonal antibodies pass from a pregnant person to their developing baby, especially in the third trimester (last 3 months of pregnancy). Therefore, a baby will likely be exposed to Kevzara if a pregnant person takes it.
One study looked at pregnant animals who were given Kevzara. Researchers found no change in the growth or development of the offspring up to 1 month after birth. However, there was a noticeable decrease in the level an antibody called IgG in the offspring. (An antibody is a protein in your blood that’s part of your immune system. And your immune system is your body’s defense against infection.) The decrease in the IgG level may mean that infants could have a weakened immune system because of their exposure to Kevzara.
Animal studies also showed that Kevzara can lead to a delay in labor and delivery. However, animal studies don’t always predict what happens in humans.
To better understand the effects of Kevzara during pregnancy, a pregnancy registry was created for the drug. A pregnancy registry collects data on how pregnant people and their babies are affected by a medication. If you’re pregnant and are taking Kevzara, you or your doctor can call 877-311-8972 to register. You can also visit the MotherToBaby website to learn more about the registry and sign up for it.
If you’re pregnant or planning to become pregnant, talk with your doctor before taking Kevzara. They’ll talk with you about the risks and benefits of taking the drug while pregnant.
It’s not known if Kevzara is safe to take during pregnancy. Keep in mind that Kevzara can make oral contraceptive medication less effective. This means that your birth control may not work as well or at all. It can even stop the birth control from working for several weeks after you stop taking Kevzara. (For more information, see “Kevzara and oral contraceptives” in the “Kevzara interactions” section above.)
If you or your sexual partner can become pregnant, talk with your doctor about your birth control needs while you’re using Kevzara. Be sure to have this talk before taking Kevzara.
It’s not known if Kevzara is safe to take while you’re breastfeeding. There are no human or animal studies showing whether Kevzara can get into breast milk and pass to a child. It’s also not known if Kevzara can affect milk production of the person taking it.
If you’re breastfeeding, talk with your doctor before taking Kevzara. They can discuss the best medication and child feeding options with you.
This drug comes with several precautions.
FDA warning: Serious infections
This drug has a
Serious infections have occurred in people taking Kevzara. These infections included ones caused by bacteria, viruses, and fungi. Some infections required people to go to the hospital or led to death.
If you get a serious infection, tell your doctor right away. You may need to stop taking Kevzara until your infection clears up.
Your doctor may also test you for the lung disease tuberculosis (TB) before you start to take Kevzara. If you test positive for TB, you’ll be treated for TB before starting Kevzara treatment. Your doctor will monitor how you feel and check for any signs of infection during the time you’re taking Kevzara.
Other precautions
Before taking Kevzara, talk with your doctor about your health history. Kevzara may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Allergic reactions. You shouldn’t take Kevzara if you had an allergic reaction to the medication in the past or to arginine, histidine, polysorbate 20, or sucrose, which are all in the medication.
- Pregnancy. It’s not known if Kevzara is safe to take during pregnancy. For more information, please see the “Kevzara and pregnancy” section above.
- Breastfeeding. It is not known if Kevzara is safe to take while you’re breastfeeding. For more information, please see the “Kevzara and breastfeeding” section above.
- Gastrointestinal diseases, such as diverticulitis or ulcers. If you have a history of diverticulitis (swelling in your intestines) or ulcers (sores) in your stomach or intestines, tell your doctor. Kevzara can increase the risk for gastrointestinal perforations, which are tears in the lining of your stomach or intestines and can be very serious.
- Use of nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids. Taking Kevzara with certain drugs can increase your risk for tears in the lining of your stomach or intestines. These drugs include nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil) or naproxen (Aleve), and corticosteroids such as prednisone (Deltasone). If you’re taking Kevzara and any of these drugs, tell your doctor right away if you develop stomach pain or a fever that doesn’t go away.
- Live vaccines. You shouldn’t get any live vaccines while you’re taking Kevzara. (See the “Kevzara interactions” section above to learn more.) Ask your doctor if you need any live vaccines before taking Kevzara.
- Liver disease. If you have liver disease, you shouldn’t use Kevzara. The medication can increase levels of liver enzymes and make your liver disease worse. Ask your doctor what other drug would be better for you.
- Tuberculosis or other infections. Kevzara can weaken your immune system (your body’s defense against infection) and cause an infection to get worse. So you shouldn’t take Kevzara when you have an infection. This includes fungal, viral, or bacterial infections, as well as TB. Your doctor will need to treat the infection before you start taking Kevzara.
- Cancer. If you’ve had any type of cancer in the past, taking Kevzara may increase your risk for developing cancer such as lymphoma or skin cancer. The drug may also increase your risk for the cancer you had to come back. If you have a history of cancer, be sure to tell your doctor. They may recommend a different medication for you.
Note: For more information about the potential negative effects of Kevzara, see the “Kevzara side effects” section above.
Using more than the recommended dosage of Kevzara can lead to serious side effects. It’s important to have only one injection every 2 weeks or as recommended by your doctor.
Overdose symptoms
There were no cases of overdose in clinical trials. It’s not known what symptoms may occur if you take too much Kevzara.
What to do in case of overdose
If you think you’ve taken too much of this drug, call your doctor. You can also call the American Association of Poison Control Centers at 800-222-1222 or use their online tool. But if your symptoms are severe, call 911 or go to the nearest emergency room right away.
When you get Kevzara from the pharmacy, the pharmacist will add an expiration date to the label on the box. This date is typically 1 year from the date they dispensed the medication.
The expiration date helps guarantee the effectiveness of the medication during this time. The
Storage
How long a medication remains good can depend on many factors, including how and where you store the medication.
You should store Kevzara in the refrigerator between 36°F and 46°F (2°C to 8°C). It should be protected from light, so be sure to keep it in the original carton. Never freeze or shake Kevzara. You’ll take Kevzara out of the refrigerator 30 minutes before a dose so it can warm up.
You can store Kevzara syringes and pens at a room temperature of up to 77°F (25°C) for a maximum of 14 days. Keep them in the original carton to protect them from light. If you don’t use a syringe or pen within 14 days at room temperature, you must throw it out.
Disposal
If you no longer need to take Kevzara and have leftover medication, it’s important to dispose of it safely. This helps prevent others, including children and pets, from taking the drug by accident. It also helps keep the drug from harming the environment.
The
Don’t put used Kevzara syringes or pens in your regular trash. You also should never reuse them. Dispose of your used syringes or pens in an FDA-approved sharps container. For more information on how to properly get rid of your syringe or pen, see the
The following information is provided for clinicians and other healthcare professionals.
Indications
Kevzara is indicated for use in adult patients with moderate to severe rheumatoid arthritis (RA) who have active disease. It should only be used in patients who have a poor response or are not tolerant to at least one disease modifying antirheumatic drug (DMARD). It is not approved for use in children.
Mechanism of action
Kevzara is an interleukin-6 (IL-6) antagonist, which binds to and blocks signaling through IL-6 mediated receptors. Because IL-6 is a pro-inflammatory cytokine, it contributes to inflammation, joint pain, and fatigue. By blocking IL-6 signaling, Kevzara can help reduce pain and inflammation in the joints of patients with RA.
Pharmacokinetics and metabolism
The median time to maximum plasma concentration is 2 to 4 days after a dose of Kevzara. Steady state occurred after 14 to 16 weeks of treatment. The volume of distribution at steady state was 7.3 L.
Because Kevzara is a monoclonal antibody, it is believed to degrade in the same way as endogenous IgG. It is likely broken down into small peptides and amino acids through catabolic paths. However, the exact method of Kevzara metabolism has not yet been determined.
Due to the nature of the monoclonal antibody, it is not excreted by renal or hepatic pathways. Elimination is dependent on drug concentration. At high concentrations, elimination is mediated by non-saturable, linear proteolytic pathways. In contrast, when Kevzara is at lower concentrations, it is eliminated via saturable, nonlinear target-mediated pathways.
The half-life of Kevzara is dependent on drug concentration. At the recommended dose of 200 mg every 2 weeks, half-life is about 10 days in patients at steady state. The median time to non-detectable concentration of Kevzara in the body is 43 days after the last dose when the medication is at steady state and dosed at 200 mg.
Contraindications
Kevzara is contraindicated for use in patients who have experienced a past hypersensitivity to Kevzara or any of the ingredients in Kevzara, including arginine, histidine, polysorbate 20, or sucrose.
Storage
Kevzara should be refrigerated at a temperature between 36°F and 46°F (2°C to 8°C). It should be kept in its original carton in order to protect it from light. Never freeze or shake the medication.
Kevzara syringes or pens can be stored at room temperature up to 77°F (25°C) for up to a maximum of 14 days. They must be stored in the original carton to protect them from light at room temperature as well. If a syringe or pen isn’t used within 14 days at room temperature, it must be disposed of.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.