Lialda is a brand-name oral tablet prescribed for mild or moderate ulcerative colitis. Lialda contains the active drug mesalamine and belongs to the aminosalicylate drug class.
Lialda is FDA-approved to induce (cause) and maintain remission of ulcerative colitis in adults and certain children. Remission refers to having few or no symptoms.
You’ll find key information about Lialda below.
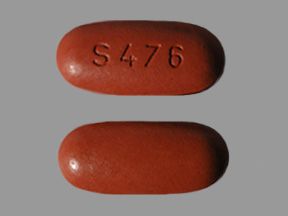
- Drug form: delayed-release oral tablet (delayed-release means the drug is released into your body after it passes through your stomach)
- Generic available? Yes
- Prescription required? Yes
- Controlled substance? No
- Year of FDA approval: 1987
Lialda is a brand-name drug that contains the active drug mesalamine. This active drug is also available in generic forms. A generic drug is an exact copy of the active drug in a brand-name medication.
Generics are considered as safe and effective as the original drug. Generics tend to cost less than brand-name drugs.
If you’re interested in using a generic form of Lialda, talk with your doctor. They can tell you if it comes in forms and strengths suitable for your condition.
Other brand-name versions of mesalamine are also available. These include Apriso, Delzicol, and Pentasa. If you’d like to know about these other drugs and find out possible dosage conversions (how to convert from taking one drug to taking the other), ask your doctor.
Lialda can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Lialda. These lists do not include all possible side effects.
Most of the drug’s side effects are not long term. However, some can be long lasting. These include certain liver problems and kidney problems. See the “Serious side effects” list below to learn more.
For more information on the possible side effects of Lialda, talk with your doctor or pharmacist. They can give you tips on how to manage any side effects that may concern or bother you.
Note: The Food and Drug Association (FDA) tracks side effects of drugs they have approved. If you would like to report to the FDA a side effect you’ve had with Lialda, you can do so through MedWatch.
Mild side effects
Below is a partial list of mild side effects of Lialda. To learn about other mild side effects, talk with your doctor or pharmacist, or view Lialda’s prescribing information.
Mild side effects of Lialda can include:
- flatulence (passing gas)
- abnormal liver function test results, which could be a sign of liver problems
- abdominal pain
- diarrhea
- headache
- hair loss
- itchiness
- upset stomach
- back pain or joint pain
- fatigue
- mild allergic reaction*
Most of these side effects may go away within a few days to a couple of weeks. However, if they become more severe or do not go away, talk with your doctor or pharmacist.
* For more information about allergic reaction and Lialda, see “Allergic reaction” below.
Serious side effects
Serious side effects from Lialda are not common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include:
- Liver problems, including liver failure in people who already have liver problems. Symptoms can include:
- jaundice (yellowing of your skin or the whites of your eyes)
- pain in the right side of your upper abdomen
- Mesalamine-induced acute intolerance syndrome. Symptoms can be hard to tell apart from a flare-up of ulcerative colitis. They may include:
- abdominal pain or cramping
- bloody diarrhea
- fever
- headache
- rash
- Kidney problems, including kidney failure and kidney stones. Symptoms can include:
- passing less urine than usual
- swollen ankles, feet, or legs
- shortness of breath
- nausea
- pain in your abdomen, back, or pelvis
- frequent need to urinate, but passing only small amounts of urine
- blood in your urine
- Pancreatitis (inflammation of your pancreas). Symptoms can include:
- nausea and vomiting
- diarrhea
- abdominal swelling and tenderness
- fever
- Skin rashes, including severe rashes from Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and drug reaction with eosinophilia and systemic symptoms (DRESS). Symptoms can include:
- rash that peels or has blisters
- fever
- body aches
- Severe allergic reaction.*
* For more information about allergic reaction and Lialda, see “Allergic reaction” below.
Side effects in children
Lialda treats active ulcerative colitis in children who weigh at least 24 kilograms. (This is about 53 pounds.) Lialda’s side effects in children are generally similar to those in adults.
More common side effects of Lialda in children may include:
- abdominal pain
- infection, such as upper respiratory infection
- vomiting
- headache
- anemia (low red blood cell level)
These side effects are usually mild. If they occur, they should ease within a few days or a couple of weeks. But if they’re severe or don’t go away, talk with your child’s doctor.
ALLERGIC REACTIONAs with most drugs, some people can have an allergic reaction after taking Lialda. This side was rare in clinical trials of this drug.
Symptoms of a mild allergic reaction can include:
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
Allergic reactions that affect the heart have also been reported with Lialda. These include myocarditis (inflammation of the heart muscle) or pericarditis (inflammation of the lining of your heart). Symptoms can include:
- abnormal heart rate
- chest pain
- trouble breathing
Call your doctor right away if you have an allergic reaction to Lialda, as the reaction could become severe. Call 911 or your local emergency number if your symptoms feel life threatening or if you think you’re having a medical emergency.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to suit your needs.
Drug form and strengths
Lialda comes as a delayed-release oral tablet. Delayed release means it has a special coating that allows it to pass through the stomach before dissolving.
The tablets are available in one strength: 1.2 grams (g).
Dosage for induction of ulcerative colitis remission in adults
Induction of ulcerative colitis remission means treating your symptoms until they get better or go away.
The usual dosage for inducing remission is two to four Lialda tablets taken once per day with a meal. So, your doctor may prescribe 2.4–4.8 g daily, for you to take with food.
Dosage for maintenance of ulcerative colitis remission in adults
Maintaining ulcerative colitis remission involves taking Lialda long term, even when you don’t have symptoms. This helps manage your symptoms and prevent them from coming back.
The usual dose for maintenance of remission is two Lialda tablets taken once a day with a meal. So, your prescribed dosage would be 2.4 g daily, taken with food.
Children’s dosage
Recommended dosages of Lialda for children are based on body weight. Doctors prescribe this drug for children who can swallow tablets whole and weigh at least 24 kilograms (kg). This is about 53 pounds (lb).
For the first 8 weeks, the typical recommended daily dosage of Lialda for children is as follows:
- For children weighing 24 kg to 35 kg, their daily dose is 2.4 g.
- For children weighing more than 35 kg to 50 kg, their daily dose is 3.6 g.
- For children weighing more than 50 kg, their daily dose is 4.8 g.
After 8 weeks of treatment, your child’s doctor will likely reduce the dosage of Lialda as follows:
- For children weighing 24 kg to 35 kg, their daily dose is 1.2 g.
- For children weighing more than 35 kg to 50 kg, their daily dose is 2.4 g.
- For children weighing more than 50 kg, their daily dose is 2.4 g.
Your child should take Lialda with food.
Your child will continue taking the prescribed dose each day for as long as their doctor recommends.
About taking Lialda
Below you’ll find information about key dosage issues.
- When to take: You can take Lialda at any time of day but try to take it at the same time each day. Taking the medication around the same time of day helps keep a steady level of the drug in your body. This helps Lialda work effectively.
- If you miss a dose: If you forget to take a dose of Lialda at your usual time, take it as soon as you remember. However, if it’s almost time for your next dose, skip the missed dose. Then, take your next dose at your usual time. Never take two doses at once to make up for a missed dose. Doing this can increase your risk of certain side effects.
- Taking Lialda with food: You should take Lialda with food, such as a meal or snack.
- Crushing, splitting, or chewing Lialda: You should swallow Lialda tablets whole with a drink. Do not crush, split, chew, or try to dissolve the tablets.
- Length of use: Lialda is meant to be used as a long-term treatment. If you and your doctor determine that Lialda is safe and effective for you, you’ll likely take it long term.
- Length of time to work: Lialda will start to reduce the inflammation in your bowel as soon as you start taking it. However, it may take a few weeks before your symptoms improve.
Lialda overdose
Taking more than the recommended dosage of Lialda can lead to serious side effects. Do not take more Lialda than your doctor recommends.
Overdose symptoms
Symptoms of an overdose can include:
- ringing in the ears
- spinning sensation
- headache
- confusion
- seizures
- fast breathing
- trouble breathing
- nausea
- vomiting
- damage to the kidneys or liver
What to do in case of overdose
If you think you’ve taken too much of this drug, call your doctor. You can also call America’s Poison Centers at 800-222-1222 or use their online tool. However, if your symptoms are severe, call 911 or your local emergency number, or go to the nearest emergency room right away.
Other drugs are available that can treat ulcerative colitis. Some may be a better fit for you than others. If you’re interested in finding an alternative to Lialda, talk with your doctor. They can tell you about other medications that may work well for you.
The following drugs are similar to Lialda:
- other aminosalicylates taken by mouth, such as:
- balsalazide (Colazal)
- sulfasalazine (Azulfidine)
- other forms of mesalamine (Delzicol, Pentasa)
- aminosalicylates taken rectally, such as:
- mesalamine (Rowasa, sfRowasa, Canasa)
- corticosteroids taken by mouth, such as:
- budesonide (Uceris)
- hydrocortisone (Cortef)
- methylprednisolone (Medrol)
- prednisone (Rayos)
- corticosteroids administered rectally, such as:
- budesonide (Uceris rectal foam)
- hydrocortisone (Colocort, Cortenema)
- biologic therapies, such as:
- adalimumab (Humira)
- golimumab (Simponi)
- vedolizumab (Entyvio)
As with all medications, the cost of Lialda can vary. The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
Drug coupons: You can visit Optum Perks* for price estimates of Lialda. These estimates are based on the use of Optum Perks coupons. Note: You cannot use Optum Perks coupons with any insurance copays or benefits.
Financial and insurance assistance: If you need financial support to pay for Lialda, or if you need help understanding your insurance coverage, help is available.
A program called Help at Hand is available for Lialda. For more information and to find out if you’re eligible for support, call 800-830-9159 or visit the program website.
To learn more about saving money on prescriptions, check out this article.
Generic version: Lialda is available in generic forms. A generic drug is an exact copy of the active drug in a brand-name medication. The generic is considered to be as safe and effective as the original drug. And generics tend to cost less than brand-name drugs. To find out how the cost of generic mesalamine compares to the cost of Lialda, talk with your doctor or pharmacist.
* Optum Perks is a sister site of Medical News Today.
The Food and Drug Administration (FDA) approves prescription drugs such as Lialda to treat certain conditions. Lialda may also be prescribed off-label for other conditions. Off-label use is when a drug that’s approved to treat one condition is prescribed to treat a different condition.
Lialda for induction of ulcerative colitis remission in adults
Lialda is approved for inducing remission of active mild to moderate ulcerative colitis in adults. (When the disease is active, you have lots of symptoms.) Inducing remission means treating your symptoms until they get better or go away.
With ulcerative colitis, you have inflammation in your colon. This can cause diarrhea, abdominal pain, severe urges to use the bathroom, and other symptoms. You can learn more about ulcerative colitis in our inflammatory bowel disease (IBD) hub.
Lialda for maintenance of ulcerative colitis remission in adults
Lialda is also approved for maintaining mild to moderate ulcerative colitis remission in adults.
Maintenance of remission means taking Lialda on a long-term basis, even when you don’t have symptoms. This helps prevent any symptoms from returning or worsening.
Lialda and children
Lialda is FDA-approved to treat mild to moderately active ulcerative colitis in children who:
- can swallow tablets whole, and
- weigh at least 24 kilograms, which equals about 53 pounds
You may wonder how Lialda compares to other medications that doctors prescribe for ulcerative colitis. Here we look at how Lialda, Apriso, and Asacol HD are alike and different.
Note: Asacol HD has been discontinued and is no longer available in the United States.
| Lialda | Apriso | Asacol HD | |
| Active drug | mesalamine | mesalamine | mesalamine |
| Form | delayed-release* oral tablet | oral tablet that’s both extended-release and delayed-release* | delayed-release* oral tablet |
| Uses | • cause remission (a period of few or no symptoms) of mild to moderate ulcerative colitis • maintain remission of mild to moderate ulcerative colitis | • maintain remission of ulcerative colitis | • cause remission of moderate ulcerative colitis |
Since these medications all contain the same active drug, all three drugs can cause very similar side effects.
To learn more about these drugs, including their side effects, you can refer to the prescribing information for Lialda, Apriso, and Asacol HD. You can also talk with your doctor or pharmacist.
* Delayed release means the tablets have a special coating that allows them to pass through the stomach before dissolving. Extended release means the drug gets released into the body slowly over time.
Here are answers to some frequently asked questions about Lialda.
Is Lialda a biologic?
No, Lialda is not a biologic. Biologic medications are made using living cells. They’re designed to act on specific substances in your immune system. Biologics for ulcerative colitis target the substances that are causing the inflammation in your bowel. They tend to be used for more severe forms of ulcerative colitis when other drugs have not worked.
Lialda is a type of medication called an aminosalicylate. It’s made from chemicals, not from living cells. Lialda also reduces bowel inflammation, but it does this in a less targeted way than biologics.
You can talk with your doctor or pharmacist for details about how Lialda compares with biologics for your condition.
Is Lialda a blood thinner or an NSAID?
No, Lialda is not a blood thinner or a nonsteroidal anti-inflammatory drug (NSAID).
Instead, Lialda is an aminosalicylate medication that reduces inflammation in your colon and rectum.
Lialda contains the active drug mesalamine. This drug is structurally related to aspirin, which is a blood thinner and an NSAID. However, Lialda works differently in your body than aspirin.
Very rarely, Lialda may cause a decrease in the number of platelets (a type of cell) in your blood. This could make you bruise or bleed more easily because platelets usually help your blood to clot. However, Lialda is not used as a blood thinner.
If you have questions about how Lialda compares with other types of drugs, you can ask your doctor or pharmacist.
Can Lialda be used for Crohn’s disease or IBS?
No. Lialda isn’t FDA-approved for Crohn’s disease or irritable bowel syndrome (IBS). Instead, Lialda is approved to treat mild to moderate ulcerative colitis.
Crohn’s disease and ulcerative colitis are the two main types of inflammatory bowel disease (IBD). Some drugs, such as adalimumab (Humira), can be used to treat either type of IBD. But Lialda isn’t one of them. According to a review of separate studies, mesalamine (the active drug in Lialda) is not as effective as other treatments for Crohn’s disease.
People often confuse IBD with IBS, but they are different conditions. IBS is a gut disorder that causes changes in your bowel movements, among other symptoms.
Some people with IBS may have some low-grade inflammation in their bowel. Mesalamine is being investigated as a possible treatment for this type of IBS. However, more studies are needed before it’s known if mesalamine is effective for IBS.
If you have IBS or Crohn’s disease, talk with your doctor about your treatment options.
If you can become pregnant, consider the following information about pregnancy, birth control, and breastfeeding.
Lialda and pregnancy
It’s unknown whether Lialda is safe to take during pregnancy. But some studies and reviews of studies have shown that Lialda might be safe for use during pregnancy.
It’s important to note that there are risks associated with having unmanaged ulcerative colitis while pregnant. (Lialda is used for managing ulcerative colitis.)
The American Gastroenterological Association (AGA) recommends that you can take mesalamine (the active drug in Lialda) during pregnancy to help maintain remission (having few or no symptoms). Current evidence suggests that the benefits of taking mesalamine to help keep ulcerative colitis in remission outweigh the possible risks.
If you’re pregnant, planning a pregnancy, or can become pregnant, talk with your doctor about treatment options for ulcerative colitis during pregnancy. Together, you can consider the risks and benefits of your treatment options and decide whether you should take Lialda during pregnancy.
You can also refer to this article for details about ulcerative colitis and pregnancy.
Lialda and birth control
It’s unknown if Lialda is safe to take during pregnancy. If you’re sexually active and you or your partner can become pregnant, talk with your doctor about your birth control needs while you’re taking Lialda.
Lialda and breastfeeding
It’s unknown whether you should take Lialda while breastfeeding. Mesalamine, the active drug in Lialda, can pass into breast milk in small amounts. Diarrhea has been reported in some children breastfed by people taking mesalamine.
If you’re currently breastfeeding or planning to do so, talk with your doctor before taking this medication.
Lialda can interact with several other medications, and alcohol.
Medication interactions
Medications that can interact with Lialda include:
- nonsteroidal anti-inflammatory drugs (NSAIDs), such as:
- ibuprofen (Motrin, Advil)
- diclofenac (Zipsor)
- celecoxib (Celebrex)
- azathioprine (Imuran, Azasan)
- mercaptopurine (Purinethol)
Before taking Lialda, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
Alcohol interaction
Alcohol is not known to interact with Lialda. It’s likely safe to consume alcohol while taking Lialda.
However, if you get headaches or feel nauseated while taking Lialda, drinking alcohol could worsen this.
Some people also find that drinking alcohol can cause a flare-up of ulcerative colitis. In some people, alcohol may also trigger symptoms such as diarrhea, cramping, or bloating.
If you have questions about how much alcohol is safe to drink while taking Lialda, talk with your doctor or pharmacist.
Before taking Lialda, talk with your doctor about your health history. Lialda may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- being 65 years of age or older
- history of allergic reaction to salicylate medications, such as aspirin, mesalamine, sulfasalazine (Azulfidine), olsalazine (Dipentum), or balsalazide (Colazal)
- kidney problems
- liver problems
- heart problems
- narrowing or blockage in your stomach or upper intestine
- skin conditions such as eczema or dermatitis
- pregnancy
- breastfeeding
Note: For more information about the potential negative effects of Lialda, see the “Lialda side effects” section above.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.