Admelog is a brand-name prescription drug that’s used to improve blood sugar levels in:
- adults and children (ages 3 years and older) with type 1 diabetes
- adults with type 2 diabetes
Admelog should be used at mealtimes to help manage your blood sugar level after you’ve eaten. It comes as a liquid solution that’s given by subcutaneous injection (an injection under the skin). You’ll inject Admelog using either a syringe; a prefilled disposable pen; or an insulin pump. This drug can also be given by healthcare providers as an intravenous (IV) injection (an injection into your vein).
Admelog comes in one strength: 100 units/mL. It contains the drug insulin lispro, which is a rapid-acting form of insulin. This drug is made in a lab, but it’s similar to your body’s natural insulin.
Admelog is a follow-on biologic drug of Humalog. (Humalog is considered the parent drug of Admelog.) This means Admelog is very similar to Humalog, which is also a biologic (a drug made from living cells). Follow-on drugs are often used to treat the same or very similar conditions as their parent drug treats. And they’re considered just as safe and effective as their parent drug.
FDA approval
Admelog was approved by the Food and Drug Administration (FDA) in December 2017. It’s the first follow-on, rapid-acting insulin drug that’s been approved by the FDA.
Effectiveness
Clinical studies have shown that Admelog is very similar to Humalog, which also contains insulin lispro. In fact, Admelog is considered a bioequivalent to Humalog. This means that the two drugs work the same way inside your body.
The FDA approved the use of Admelog in part based on how similar its effectiveness was to that of Humalog. Clinical studies have shown that Humalog is safe and effective in managing blood sugar levels in people with either type 1 or type 2 diabetes.
For information on the results of these studies, see the section “Admelog uses” below.
Admelog is only available as a brand-name medication.
Admelog contains the active drug insulin lispro. It’s considered a follow-on biologic of the brand-name drug Humalog.
Follow-on biologic drugs are a very similar copy of another biologic drug (a drug made from living cells). Follow-on drugs are often used to treat the same or very similar conditions as their parent drug treats. And they’re considered just as safe and effective as their parent drug.
There is a generic form of Humalog (insulin lispro) available. A generic drug is an exact copy of a brand-name medication. Generics tend to cost less than brand-name drugs.
You may wonder how Admelog compares to other medications that are prescribed for similar uses. Here we look at how Admelog and Humalog are alike and different.
Ingredients
Admelog contains the drug insulin lispro. It’s considered a follow-on biologic drug of Humalog, which also contains insulin lispro.
Follow-on biologic drugs are a very similar copy of another biologic drug (a drug made from living cells). Follow-on drugs are often used to treat the same or very similar conditions as their parent drug treats. And they’re considered just as safe and effective as their parent drug.
Both Admelog and Humalog are rapid-acting forms of insulin. This means they begin to work within 5 to 15 minutes after you’ve taken them.
Uses
Both Admelog and Humalog are approved to treat:
- type 1 diabetes in adults and children ages 3 years and older
- type 2 diabetes in adults
Drug forms and administration
Admelog comes as a liquid solution that’s given by subcutaneous injection (an injection under the skin). You’ll inject it using either a syringe; a prefilled, disposable pen; or an insulin pump. This drug can also be given by healthcare providers as an intravenous (IV) injection (an injection into your vein).
Humalog also comes as a liquid solution inside vials, injectable pens, or cartridges (which are used inside certain pens).
Humalog is also available in combination with a type of insulin called insulin lispro protamine. Insulin lispro protamine is intermediate-acting form of insulin. This means it works in your body for a longer time than does insulin lispro, which is a rapid-acting insulin. This combination product is available in two strengths:
- Humalog 75/25 (contains 75% insulin lispro protamine and 25% insulin lispro)
- Humalog 50/50 (contains 50% insulin lispro protamine and 50% insulin lispro)
Side effects and risks
Admelog and Humalog both contain insulin lispro. Because Admelog is a follow-on biologic drug of Humalog, these drugs share the same side effects. Below are lists of these side effects.
More common side effects
This list contains examples of more common side effects that can occur with both Admelog and Humalog (when they’re taken individually). More common side effects can include:
- hypoglycemia (low blood sugar level)
- injection site reaction (redness, pain, or swelling at your injection site)
- lipodystrophy (changes in the thickness of your skin near your injection sites)
- itchy skin
- skin rash
- weight gain
- swelling of your hands and feet
- respiratory infections, such as the common cold or flu
Serious side effects
This list contains examples of serious side effects that can occur with both Admelog and Humalog (when they’re taken individually). Serious side effects can include:
- severe hypoglycemia (dangerously low blood sugar level)
- severe allergic reaction
- low potassium level
Effectiveness
Admelog and Humalog both contain insulin lispro. And they’re both used to treat type 1 and type 2 diabetes. The effectiveness of Admelog to treat diabetes has been directly compared to the effectiveness of Humalog.
Studies often look at a blood test called hemoglobin A1c (HbA1c) as way to measure how well diabetes in a person is being treated. A lower HbA1c shows better control of blood sugar levels. The American Diabetes Association recommends a HbA1c goal of less than 7% for most people.
Effectiveness in treating type 1 diabetes
A 26-week clinical study compared blood sugar control in adults with type 1 diabetes. Some people were given Admelog and insulin glargine, while other people were given Humalog and insulin glargine.
In the study, Admelog and Humalog had similar effectiveness in treating type 1 diabetes. For people taking Admelog and insulin glargine, HbA1c was reduced by 0.4%. For people taking Humalog with insulin glargine, HbA1c was reduced by 0.46%.
Effectiveness in treating type 2 diabetes
Another 26-week clinical study looked at blood sugar control in adults with type 2 diabetes. Some people were given Admelog and insulin glargine, while other people were given Humalog and insulin glargine.
In this study, Admelog and Humalog had similar effectiveness in treating type 2 diabetes. For people using Admelog plus insulin glargine, HbA1c was reduced by 0.86%. For people using Humalog plus insulin glargine, HbA1c was reduced by 0.8%.
Costs
Admelog and Humalog are both brand-name drugs. There’s not a generic form of Admelog available, but there is a generic form of Humalog available. Generic medications usually cost less than brand-name drugs.
Admelog generally costs less than Humalog. The actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
You may wonder how Admelog compares to other medications that are prescribed for similar uses. Here we look at how Admelog and Novolog are alike and different.
Ingredients
Admelog contains the drug insulin lispro, while Novolog contains the drug insulin aspart. Both of these drugs are rapid-acting forms of insulin. This means they begin to work within 5 to 15 minutes after you’ve taken them.
Uses
Admelog and Novolog are both approved to treat diabetes, but they’ve been studied and approved for use in different age groups.
- Admelog can be used to treat:
- type 1 diabetes in adults and children ages 3 years and older
- type 2 diabetes in adults
- Novolog can be used to treat:
- type 1 diabetes in adults and children ages 2 years and older
- type 2 diabetes in adults
Drug forms and administration
Admelog comes as a liquid solution that’s given by subcutaneous injection (an injection under the skin). You’ll inject it using either a syringe; a prefilled, disposable pen; or an insulin pump. This drug can also be given by healthcare providers as an intravenous (IV) injection (an injection into your vein).
Novolog is a liquid solution that comes in vials, injectable pens, or cartridges (which are used inside certain pens).
Side effects and risks
Both Admelog and Novolog are rapid-acting insulins. Because both drugs work the same way in your body, they share the same side effects. Below are lists of these side effects.
More common side effects
This list contains examples of more common side effects that can occur with both Admelog and Novolog (when they’re taken individually). More common side effects can include:
- hypoglycemia (low blood sugar level)
- injection site reaction (redness, pain, or swelling at your injection site)
- · lipodystrophy (changes in the thickness of your skin near your injection sites)
- itchy skin
- skin rash
- weight gain
- swelling in your hands and feet
Serious side effects
This list contains examples of serious side effects that can occur with both Admelog and Novolog (when taken individually). Serious side effects can include:
- severe hypoglycemia (dangerously low blood sugar level)
- severe allergic reaction
- low potassium level
Effectiveness
Admelog and Novolog are both used to treat type 1 and type 2 diabetes. And the effectiveness of Admelog has been directly compared to the effectiveness of Novolog.
Studies often look at a blood test called hemoglobin A1c (HbA1c) as way to measure how well diabetes in a person is being treated. A lower HbA1c shows better control of blood sugar levels. The American Diabetes Association recommends a HbA1c goal of less than 7% for most people.
In a large study of people with either type 1 or type 2 diabetes, insulin lispro (the active drug in Admelog) was compared to insulin aspart (the active drug in Novolog). HbA1c was reduced by about 0.1% in people taking insulin lispro. In comparison, people taking insulin aspart had their HbA1c decreased by about 0.2%.
This study showed that both drugs had similar effectiveness and were each safe to use.
Costs
Admelog and Novolog are both brand-name drugs. There are currently no generic forms of either drug. Brand-name medications usually cost more than generics.
Admelog costs significantly less than Novolog. The actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
Other rapid-acting insulins are available as alternatives to Admelog. Other forms of insulin can also be used to treat diabetes. Some insulins may be better suited for you than others.
If you’re interested in finding an alternative to Admelog, talk with your doctor. They can tell you about other medications that may work well for you.
Examples of other rapid-acting insulins that may be used to treat type 1 or type 2 diabetes include:
- insulin lispro (Humalog); this drug is discussed in detail in the “Admelog vs. Humalog” section above
- insulin aspart (Fiasp, Novolog); this drug is discussed in detail in the “Admelog vs. Novolog” section above
- insulin glulisine (Apidra)
As with all medications, the cost of Admelog can vary.
The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
Your insurance plan may require you to get prior authorization before approving coverage for Admelog. This means that your doctor and insurance company will need to communicate about your prescription before the insurance company will cover the drug. The insurance company will review the request and let you and your doctor know if your plan will cover Admelog.
If you’re not sure if you’ll need to get prior authorization for Admelog, contact your insurance company.
Financial assistance
If you need financial support to pay for Admelog, help is available. Sanofi-Aventis U.S. LLC, the manufacturer of Admelog, offers the Admelog Savings Card. For more information and to find out if you’re eligible for support, call 833-813-0190 or visit the program website.
Admelog can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Admelog. These lists don’t include all possible side effects.
For more information on the possible side effects of Admelog, talk with your doctor or pharmacist. They can give you tips on how to deal with any side effects that may be bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs they have approved. If you would like to report to the FDA a side effect you’ve had with Admelog, you can do so through MedWatch.
Mild side effects
Mild side effects of Admelog that are more common include:
- respiratory infections, such as the common cold or flu
- hypoglycemia (low blood sugar level)
Mild side effects of Admelog that are less common include:
- lipodystrophy (changes in the thickness of your skin near your injection sites)
- weight gain
- swelling in your feet or ankles
- injection site reaction (redness, pain, or swelling at your injection site)
- itchy skin
- skin rash
Most of these side effects may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk with your doctor or pharmacist.
Serious side effects
Serious side effects from Admelog aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects, which are discussed below in “Side effect details,” can include the following:
- severe allergic reaction
- severe hypoglycemia (dangerously low blood sugar level)
- low potassium level
Side effect details
You may wonder how often certain side effects occur with this drug. Here’s some detail on a few of the side effects this drug may cause.
Allergic reaction
As with most drugs, some people can have an allergic reaction after taking Admelog. But it’s not known for sure how many people have had allergic reactions to Admelog.
Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (warmth and redness in your skin)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
Call your doctor right away if you have a severe allergic reaction to Admelog. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Hypoglycemia
It’s possible to have hypoglycemia (low blood sugar level) when you’re using an insulin drug, such as Admelog. Insulin is used to help manage and lower your blood sugar level. But sometimes, your blood sugar level can become too low when you take insulin.
Symptoms of hypoglycemia can include:
- shaking
- dizziness
- sweating
- tiredness
- confusion
In clinical studies, 2.4% of people using Admelog had severe hypoglycemia over 26 weeks of treatment. This number increased to 13.5% in people using Admelog for 1 year.
Hypoglycemia is a common side effect of all insulin drugs. Sometimes it’s mild and is easily treated by eating or drinking something to increase your blood sugar level. But other times, it can be more serious. Severe hypoglycemia may lead to life-threatening side effects, including seizures or death.
If your blood sugar level gets too low, your symptoms can become a medical emergency. Symptoms of severe hypoglycemia (very low blood sugar) can include sweating, confusion, anxiety, seizure, and even coma. If you or someone you know has these symptoms, call 911 right away.
Talk with your doctor about how often you should check your blood sugar level to monitor for hypoglycemia while you’re taking Admelog. Your doctor can also suggest ways to help prevent hypoglycemia while you’re using Admelog.
Low potassium level
Low potassium level (hypokalemia) is a possible side effect of Admelog. But it wasn’t reported how often this occurred in people using Admelog during clinical studies.
Symptoms of low potassium can include:
- feeling weak
- fatigue (lack of energy)
- constipation
- muscle cramps
- heart palpitations (when your heart flutters or pounds)
Serious cases of hypokalemia can lead to life-threatening side effects, including trouble breathing, heart rhythm problems, or even death.
If you have symptoms of hypokalemia, call your doctor right away. But If you have symptoms that feel life threatening, call 911.
Be sure to talk with your doctor about how often they’ll check your potassium level while you’re using Admelog. Your doctor may also suggest ways to help prevent hypokalemia while you’re using the drug. This could include recommending that you eat foods that are high in potassium.
Admelog can be used alone or in combination with other drugs to help manage blood sugar levels. These levels change throughout the day depending on what foods you eat, if you exercise, and your overall health.
It’s common for people to use more than one drug to treat their diabetes. Examples of drugs that are used to control blood sugar levels are listed below.
Examples of other insulins that may be used with Admelog in people with type 1 or type 2 diabetes include:
- intermediate-interacting insulin, such as:
- regular human insulin (Humulin N, Novolin N)
- long-acting insulin, such as:
Examples of other medications that may be used with Admelog in people with type 2 diabetes include:
- glucagon-like peptide-1 (GLP-1) receptor agonists, such as:
- dipeptidyl peptidase-4 (DPP-4) inhibitors, such as:
- alogliptin (Nesina)
- linagliptin (Tradjenta)
- saxagliptin (Onglyza)
- sitagliptin (Januvia)
- meglitinides, such as:
- repaglinide
- nateglinide
- metformin (Glumetza, Riomet)
- sodium-glucose cotransporter 2 (SGLT2) inhibitors, such as:
- sulfonylureas, such as:
- glimepiride (Amaryl)
- glipizide (Glucotrol)
- glyburide (DiaBeta, Glynase)
- thiazolidinediones (TZDs), such as:
- pioglitazone (Actos)
- rosiglitazone (Avandia)
Admelog with other drugs to treat type 1 diabetes
If you have type 1 diabetes, you may need to use a combination of insulins during the day to keep your blood sugar level stable. This might include taking a long-acting insulin (such as insulin glargine) with a rapid-acting insulin (such as Admelog).
Longer-acting insulins are typically given once or twice each day. They work in your body over several hours to maintain control of your blood sugar level. Shorter-acting insulins are used around mealtimes. They help control blood sugar spikes, which are commonly seen after eating.
Admelog with other drugs to treat type 2 diabetes
If you have type 2 diabetes, you may also need to use a combination of medications to keep your blood sugar level stable. This could include using a combination of insulins or using other injectable or oral drugs to help control your blood sugar level.
The Admelog dosage your doctor prescribes will depend on several factors. These include:
- the type and severity of the condition you’re using Admelog to treat
- your age
- your diet and exercise habits
- other diabetes medications you’re taking
- your blood sugar level goals
- whether you’re taking Admelog using prefilled pens, an insulin pump, or syringes
- other medical conditions you may have
Typically, your doctor will start you on a low dosage. Then they’ll adjust it over time to reach the amount that’s right for you. Your doctor will ultimately prescribe the smallest dosage that provides the desired effect.
Be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to suit your needs.
Your doctor may adjust your dosage depending on other factors, including other drugs you are taking or if you’re switching insulins. If you have questions about the dosage that’s right for you, talk with your doctor.
Drug forms and strengths
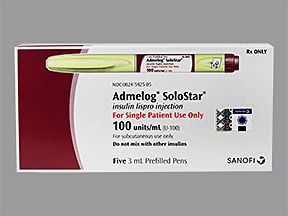
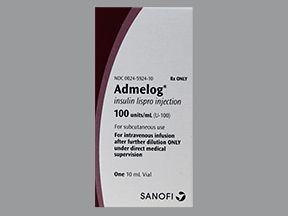
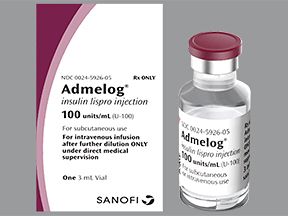
Admelog is a liquid solution that comes in either a vial or an injectable pen. It’s available in these sizes:
- 10-mL vials (each containing 1,000 units of insulin lispro)
- 3-mL vials (each containing 300 units of insulin lispro)
- 3-mL SoloStar pens (prefilled, disposable pens that each contain 300 units of insulin lispro)
Dosage for type 1 diabetes
If you have type 1 diabetes, your total daily insulin dosage is based on your body weight. Daily dosages can range from 0.4 units to 1.0 unit of insulin per kilogram (about 2.2 pounds) of body weight. This amount of insulin is divided up between your long-acting and short-acting insulins. (Admelog is a short-acting insulin.)
Admelog is typically taken with each of your meals. It should be used 15 minutes before your meal or right after you’ve eaten. When it’s self-injected, this drug is given as a subcutaneous (under your skin) injection. It can be injected under the skin of your upper arms, belly, thighs, or buttocks.
If you’re taking Admelog through an insulin pump, your doctor will explain how and when to take the medication. If you’re receiving Admelog through an intravenous (IV) injection (an injection into your vein), your doctor will determine the appropriate dosage for you.
Your doctor will adjust your dosage of Admelog to help you reach your blood sugar level goals. They may adjust your dosage every few days to weeks until your blood sugar levels are well controlled. You’ll likely use Admelog with a long-acting insulin, which is taken once or twice each day.
Dosage for type 2 diabetes
If you have type 2 diabetes, your starting dosage of Admelog is usually about 4 units each day. Typically, it’s taken with your largest meal of the day. It should be used 15 minutes before you eat or right after you’ve had a meal.
When it’s self-injected, Admelog is given as a subcutaneous (under your skin) injection. It can be injected under the skin of your upper arms, belly, thighs, or buttocks.
If you’re taking Admelog through an insulin pump, your doctor will explain how and when to take the medication. If you’re receiving Admelog through an intravenous (IV) injection (an injection into your vein), your doctor will determine the appropriate dosage for you.
Admelog is typically used with other medications to maintain blood sugar control in people with type 2 diabetes. Your doctor will adjust your dosage of Admelog to help you reach your blood sugar level goals. They may adjust your dosage every few days to weeks until your blood sugar levels are well controlled.
Pediatric dosage
For children with type 1 diabetes, total daily insulin dosage is calculated by using their body weight. Children should start at a daily dosage between 0.4 units and 1.0 unit of insulin per kilogram (about 2.2 pounds) of their body weight. This amount of insulin is then divided up between long-acting and short-acting insulins. (Admelog is a short-acting insulin.)
If Admelog is self-injected or you’re giving it to your child, this drug is given as a subcutaneous injection (an injection under the skin).
If your child is taking Admelog through an insulin pump, your doctor will explain how and when to take the medication. If your child is receiving Admelog through an intravenous (IV) injection (an injection into your vein), your doctor will determine the appropriate dosage for your child.
The child’s doctor will adjust their dosage of Admelog to help them reach their blood sugar level goals. The doctor may adjust the child’s dosage every few days to weeks until their blood sugars are well controlled. Admelog will likely be used in combination with a long-acting insulin, which is taken once or twice each day.
Admelog hasn’t been studied in children with type 2 diabetes, and it’s not approved for this use.
What if I miss a dose?
Admelog is typically taken at mealtimes to manage your blood sugar level after you’ve eaten. If it’s been less than two hours since you last ate, you can take the missed dose. However, if more than a couple of hours have passed since you last ate, just skip the missed dose. Taking insulin too long after you’ve eaten will increase your risk of low blood sugar (hypoglycemia).
Will I need to use this drug long term?
You might. Diabetes is a chronic (long-term) condition. And Admelog is meant to be used as a long-term treatment for diabetes. If you and your doctor determine that Admelog is safe and effective for you, you’ll likely take it long term.
The Food and Drug Administration (FDA) approves prescription drugs such as Admelog to treat certain conditions.
Admelog for type 1 diabetes
Admelog is approved to help improve blood sugar levels in adults and children ages 3 years and older with type 1 diabetes.
Type 1 diabetes is a chronic (long-term) disease that’s caused by a shortage of insulin in your body. Insulin is a hormone that helps sugar move from your bloodstream into your body’s cells. Once inside your cells, the sugar is processed. This is how your cells get energy to keep you alive and help your body function well.
Normally, your pancreas makes insulin. However, for people with type 1 diabetes, the pancreas doesn’t make insulin.
Without insulin, sugar isn’t able to move into cells and be processed. Since sugar can’t move into cells, it stays in your bloodstream. This raises your blood sugar level, causing symptoms and complications of diabetes.
Effectiveness in treating type 1 diabetes
Clinical studies have shown that Admelog is very similar to the drug Humalog, which also contains insulin lispro. In fact, Admelog is considered a bioequivalent of Humalog. This means that the two drugs work the same way inside your body. Studies looking at treatment with both Admelog and Humalog are described below.
In these studies, people’s hemoglobin A1c (HbA1c) was measured as a way to follow their response to treatment. A lower HbA1c shows better control of blood sugar levels. The American Diabetes Association recommends a HbA1c goal of less than 7% for most people.
Effectiveness shown in Admelog studies
One clinical study looked at blood sugar control in two groups of adults with type 1 diabetes. Some people were given Admelog and insulin glargine, while other people were given Humalog and insulin glargine.
After 26 weeks of treatment, people taking Admelog and insulin glargine had their HbA1c levels lowered by 0.4%. People taking Humalog with insulin glargine had their HbA1c levels lowered by 0.46%. These close results showed that Admelog and Humalog were similar in their effectiveness to lower people’s blood sugar levels.
Effectiveness shown in Humalog studies
The effectiveness of Admelog for adults was also determined in part by using studies that looked at the effectiveness of Humalog. This was done because Admelog and Humalog are very similar to each other, and they both contain insulin lispro. Because Admelog is so similar to Humalog, it’s expected to improve people’s blood sugar levels just like Humalog does.
Studies of Humalog were also used to determine the effectiveness of Admelog in children.
One study compared Humalog to regular human insulin. This study looked at adults and children ages 12 years and older. Over 12 months of treatment, Humalog and regular human insulin had similar effectiveness in lowering people’s blood sugar levels. People taking Humalog and people taking regular human insulin had very close HbA1c results that only differed by 0.4%.
Another clinical study was done in people ages 9 to 19 years. This study compared treatment using Humalog and NPH human insulin isophane to treatment with regular human insulin and NPH human insulin isophane. Over 8 months of treatment, no difference was seen in HbA1c levels between the two treatment groups. Both groups actually had their HbA1c increased by 0.1%.
Insulin lispro (the active drug in Admelog) has also been studied in people ages 15 years and older who use insulin pumps. (Pumps continuously deliver insulin to your body.) In two studies, some people were given Humalog, while other people were given regular human insulin.
Each of these medications was given through an insulin pump. Over 12 weeks, HbA1c was lowered 0.3% more in people taking Humalog than in people using regular human insulin.
Admelog for type 2 diabetes
Admelog is approved to help improve blood sugar levels in adults with type 2 diabetes.
Type 2 diabetes is a chronic (long-term) disease. It’s caused when your body doesn’t respond the right way to insulin. Insulin is a hormone that helps sugar move from your bloodstream into your body’s cells. Once inside your cells, the sugar is processed. This is how your cells get energy to keep you alive and help your body function well.
With type 2 diabetes, your body becomes resistant to insulin. This means that even though your body is making insulin, it doesn’t use the hormone the right way.
Because your cells don’t respond to insulin, sugar isn’t able to move into your cells and be processed. Instead, the sugar stays in your bloodstream, leading to high blood sugar levels. This results in symptoms and complications of diabetes.
Effectiveness in treating type 2 diabetes
Clinical studies have shown that Admelog is very similar to the drug Humalog, which also contains insulin lispro. In fact, Admelog is considered a bioequivalent of Humalog. This means that the two drugs work the same way inside your body. Studies looking at treatment with both Admelog and Humalog are described below.
In these studies, people’s hemoglobin A1c (HbA1c) was measured as a way to follow their response to treatment. A lower HbA1c shows better control of blood sugar levels. The American Diabetes Association recommends a HbA1c goal of less than 7% for most people.
Effectiveness shown in Admelog studies
A 26-week clinical study compared blood sugar control in two groups of people with type 2 diabetes. Some people were given Admelog and insulin glargine, while other people were given Humalog and insulin glargine.
In this study, HbA1c was reduced by 0.86% in people using Admelog plus insulin glargine. In comparison, HbA1c was reduced by 0.8% in people using Humalog plus insulin glargine. These close results showed that Admelog and Humalog were similar in their effectiveness to treat type 2 diabetes.
Effectiveness shown in Humalog studies
A separate study compared treatment with Humalog to treatment with regular human insulin in adults. Both groups also took a long-acting form of insulin. Over 3 months of treatment, HbA1c was reduced by the same amount (about 0.7%) in people taking each of the drugs.
Admelog and children
Admelog is approved for use in children 3 years or older with type 1 diabetes. It hasn’t been studied in children with type 2 diabetes, and it’s not approved for this use. For more information about how Admelog works to treat type 1 diabetes, see the section “Admelog for type 1 diabetes” above.
Effectiveness in children
The effectiveness of Admelog for children was determined by looking at studies that showed the effectiveness of Humalog. This is because Admelog and Humalog are very similar to each other, and they both contain insulin lispro. Because Admelog is so similar to Humalog, it’s expected to improve people’s blood sugar levels just like Humalog does.
In one study, children’s hemoglobin A1c (HbA1c) was measured as a way to follow their response to treatment. A lower HbA1c shows better control of blood sugar levels.
The study compared treatment with Humalog to treatment with insulin aspart in children ages 4 to 18 years. Children in this study received either drug through an insulin pump. Over 16 weeks of treatment, HbA1c was lowered 0.1% more in children taking Humalog than in children taking insulin aspart.
Alcohol may affect how well Admelog works to control your blood sugar level. Both alcohol and Admelog lower your blood sugar level. Taking them together can increase your risk of hypoglycemia (low blood sugar), which can sometimes be dangerous.
Talk with your doctor about how whether it’s safe for you to drink alcohol while you’re using Admelog.
Admelog can interact with several other medications. It can also interact with certain supplements as well as certain foods.
Different interactions can cause different effects. For instance, some interactions can interfere with how well a drug works. Other interactions can increase side effects or make them more severe.
Admelog and other medications
Below are lists of medications that can interact with Admelog. These lists do not contain all the drugs that may interact with Admelog.
Before taking Admelog, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Admelog and other diabetes medications
Taking Admelog with other diabetes medications can increase your risk of hypoglycemia (low blood sugar). If you’re taking these medications together, your doctor may need to adjust your dosages. You may also need to check your blood sugar level more often to make sure that it’s not too low.
Examples of diabetes medications that may increase your risk of hypoglycemia include:
- other insulins, such as:
- glucagon-like peptide-1 (GLP-1) receptor agonists, such as:
- dipeptidyl peptidase-4 (DPP-4) inhibitors, such as:
- linagliptin (Tradjenta)
- sitagliptin (Januvia)
- meglitinides, such as:
- metformin (Glumetza, Riomet)
- sodium-glucose cotransporter 2 (SGLT2) inhibitors, such as:
- sulfonylureas, such as:
- glimepiride (Amaryl)
- glipizide (Glucotrol)
- glyburide (DiaBeta, Glynase)
Admelog and thiazolidinediones
Using Admelog with medications from a class of diabetes drugs called thiazolidinediones (TZDs) can cause your body to retain fluid. Examples of TZDs include:
- pioglitazone (Actos)
- rosiglitazone (Avandia)
This build-up of fluid can also increase your risk of heart failure. It’s not known for sure how often fluid retention or heart failure occurs in people using Admelog. Symptoms of heart failure can include chest pain, trouble breathing, swelling in your ankles or feet, and sudden weight gain.
Call your doctor right away if you have signs of heart failure. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency. This condition can sometimes be dangerous if not treated as soon as possible.
Also, let your doctor know if you have a history of heart problems before starting Admelog. If you already have heart failure, using Admelog with a TZD may worsen your symptoms of heart failure. Your doctor will probably recommend that you don’t take a TZD drug if you have heart failure. But you’ll likely be able to use Admelog if needed for diabetes treatment.
Talk with your doctor about all the medications you’re taking before starting Admelog. If you’re taking TZDs, Admelog may not be a good treatment option for you. Your doctor will help you decide which medications will help you meet your blood sugar goals.
Drugs that decrease the effectiveness of Admelog
Taking certain drugs with Admelog can make Admelog less effective in your body. This increases your chances of having high blood sugar levels (hyperglycemia).
Examples of drugs that decrease the effectiveness of Admelog include:
- corticosteroids, such as:
- prednisone (Rayos)
- hydrocortisone (Cortef)
- isoniazid (Laniazid)
- niacin (Niacor, Niaspan)
- oral contraceptives (birth control pills)
- certain antivirals, such as
- atazanavir (Reyataz)
- ritonavir (Norvir)
- saquinavir (Invirase)
- antipsychotics, such as:
- aripiprazole (Abilify, Aristada)
- quetiapine (Seroquel)
- risperidone (Risperdal)
If you’re taking any of the medications listed above, talk with your doctor about your risk of drug interactions with Admelog.
Admelog and certain blood pressure medications
Taking certain blood pressure medications with Admelog can increase your risk of having low blood sugar (hypoglycemia).
Examples of blood pressure medications that can increase your risk of hypoglycemia include:
- lisinopril (Prinivil, Zestril)
- enalapril (Vasotec)
- losartan (Cozaar)
- valsartan (Diovan)
Other blood pressure medications can mask your symptoms of low blood sugar. This means you might not notice if your blood sugar becomes low. This can increase your risk of having very low blood sugar while you’re using Admelog, because you may not realize that you’ve taken too much Admelog.
Examples of blood pressure medications that can mask the symptoms of hypoglycemia include:
- beta-blockers, such as metoprolol (Lopressor, Toprol XL), atenolol (Tenormin), and propranolol (Inderal, Innopran XL)
- clonidine (Catapres, Kapvay)
- guanethidine
- reserpine
If you’re using Admelog with any of the blood pressure drugs listed above, your doctor may need to adjust your dosage of either medication. They may even recommend that you take a blood pressure medication that doesn’t interact with Admelog.
If you’re taking Admelog with one of these blood pressure drugs, you may also need to monitor your blood sugar level more often than usual. This will help you to make sure your blood sugar level is within a safe range.
You should take Admelog according to your doctor’s or healthcare provider’s instructions.
Admelog should be injected under the skin of your upper arms, belly, thighs, or buttocks. It can be taken by using an injectable pen or a needle, syringe, and vial.
It’s important not to share used needles with anyone else. You should also avoid sharing your Admelog pen, even if you’ve changed the needle. Not sharing needles and pens can help protect you from getting or spreading infections.
For step-by-step instructions on how to inject Admelog by using a pen or a needle and syringe, visit the manufacturer’s website.
Admelog can also be taken through an insulin pump. If you’re going to use an insulin pump to take Admelog, your doctor will explain how to take the drug.
Your doctor may also give you Admelog through an intravenous (IV) injection (an injection into your vein). You might receive the drug this way if you’re taking it in a clinic or hospital.
When to take
Admelog is usually taken with meals to help manage your blood sugar level after you’ve eaten. This drug should be taken 15 minutes before your meal or right after you’ve eaten. Your doctor will prescribe a dosage schedule that best fits your condition and blood sugar goals.
Taking Admelog with food
Be sure to eat right before or right after you’ve taken Admelog. This drug is meant to be used around the time of your meals to manage any spikes in your blood sugar level. Taking Admelog without food increases your risk of having low blood sugar (hypoglycemia).
Admelog is a rapid-acting form of insulin. It’s used to improve blood sugar levels in people with type 1 or type 2 diabetes.
What happens in diabetes?
Normally, your pancreas makes a hormone called insulin. This hormone helps sugar move into your body’s cells and be processed. This gives your cells energy to keep you alive and keep your body functioning properly.
People with type 1 diabetes have a shortage of insulin, because their body doesn’t make insulin. People with type 2 diabetes make their own insulin, but their body doesn’t respond to it very well. In both types of diabetes, sugar doesn’t have the help of insulin to leave your bloodstream and enter your cells to be processed. This leads to high levels of sugar in your bloodstream.
What does Admelog do?
Admelog is an insulin analog. This means it’s a form of insulin that’s made in a lab. But it works very much like the natural insulin that’s made inside your body.
Admelog works to lower blood sugar levels by helping sugar move from your bloodstream into your cells. Once inside your cells, the sugar can be processed and used for energy. Or the sugar can be stored and used later. Admelog also helps stop your liver from putting more sugar into your bloodstream.
How long does it take to work?
Admelog is a rapid-acting insulin. It starts to lower your blood sugar levels within 5 to 15 minutes after you’ve taken it. Admelog’s effect on lowering your blood sugar level can last for about 4 to 6 hours.
Not much is known about the safety of using Admelog during pregnancy. Other medications that contain insulin lispro (the active drug in Admelog) have been studied in pregnant women. These drugs didn’t cause any harm to developing fetuses when they were used during pregnancy.
Pregnant women are sometimes affected by diabetes. They might develop it during their pregnancy (called gestational diabetes), or they may have the condition before they become pregnant (called pregestational diabetes).
Diabetes during pregnancy is often treated with certain forms of insulin to help keep blood sugar levels normal. Blood sugar levels that aren’t well managed can lead to serious problems for the pregnant mother and her baby.
Talk with your doctor if you’re pregnant or planning to become pregnant. If you have diabetes, they can discuss what your treatment might look like during pregnancy. If you don’t have diabetes, your doctor can discuss ways to help prevent gestational diabetes from developing during your pregnancy.
If you need treatment for diabetes during pregnancy, your doctor will determine whether insulin therapy is right for you. They’ll recommend an option that they feel is safe for you and your baby.
If you’re sexually active and you or your partner can become pregnant, talk with your doctor about your birth control needs while you’re using Admelog.
There aren’t any studies to know whether Admelog is safe for use in women who are breastfeeding.
If you’re breastfeeding or planning to breastfeed while using Admelog, talk with your doctor. They can discuss the risks and benefits of using Admelog, and help you decide if this drug is the right choice for you.
Here are answers to some frequently asked questions about Admelog.
If I’m taking Humalog, can I switch to Admelog?
Yes, it’s possible to switch your treatment from Humalog to Admelog if your doctor recommends it. These medications are very similar to each other.
In fact, Admelog is called a follow-on biologic of Humalog. This means it’s very similar to Humalog. The Food and Drug Administration (FDA) consider the two drugs to have nearly the same effectiveness and safety.
Be sure to talk with your doctor before making any changes in your diabetes treatment. Switching or starting new medications may lead to serious side effects or drug interactions. Your doctor will recommend a treatment plan that’s safe and effective for you.
Is Admelog a fast-acting form of insulin?
Yes, Admelog is considered a rapid-acting insulin. This means it begins to work very quickly after you’ve taken it.
Admelog starts to work about 5 to 15 minutes after it’s taken. Rapid-acting insulins (including Admelog) are typically taken at mealtime to prevent spikes in your blood sugar level after you’ve eaten.
Can I use Admelog in my insulin pump?
Yes, Admelog can be used with an insulin pump. But be sure to follow your pump’s instructions for use. Also, you’ll want to replace the Admelog that’s in your pump at least every 7 days. This helps to make sure the drug is still safe and effective for you.
Why do I need Admelog if I’m already taking long-acting insulin?
Long-acting insulin is used to control blood sugar over the course of an entire day. It lasts several hours in your body. However, eating food increases your blood sugar level, which can sometimes cause large spikes in your blood sugar.
Admelog and other rapid-acting insulins are used right before or right after meals. These forms of insulin help to prevent large spikes in your blood sugar level and help manage your blood sugar level.
How soon after taking Admelog do I need to eat?
You should try to eat within about 15 minutes after taking Admelog. This drug begins working to lower your blood sugar about 5 to 15 minutes after you’ve taken your dose. If you take Admelog without eating any food, you have an increased risk of hypoglycemia (low blood sugar). Sometimes, low blood sugar can be dangerous if your blood sugar level drops too low.
Before taking Admelog, talk with your doctor about your health history. Admelog may not be right for you if you have certain medical conditions. These include:
- Current hypoglycemia. You should never use Admelog while you have hypoglycemia (low blood sugar). Taking this drug may lead to severe hypoglycemia and cause serious and life-threatening side effects.
- Low potassium levels. Admelog can cause you to have a low potassium level, which may lead to serious heart problems. If you have certain health conditions or use medications that lower your potassium level, Admelog can further lower the level. Your doctor will likely monitor your potassium level more closely during Admelog treatment if you’re at risk of having a low potassium level.
- Allergic reaction. If you’ve had an allergic reaction to insulin lispro or any other ingredients in Admelog, you shouldn’t take the medication. If you’ve had allergies to any form of insulin in the past, talk with your doctor before starting Admelog.
- Pregnancy and breastfeeding. Not much is known about the safety of using Admelog while you’re pregnant or breastfeeding. For more information, see the “Admelog and pregnancy” and “Admelog and breastfeeding” sections above.
Note: For more information about the potential negative effects of Admelog, see the “Admelog side effects” section above.
It’s possible to overdose on Admelog if you take too much of the drug. Always follow the dosage schedule your doctor gives you to help prevent overdose.
Overdose symptoms
Overdosing on Admelog can cause serious problems, such as:
- Severe hypoglycemia (dangerously low blood sugar level). Symptoms can include:
- shaking
- dizziness
- sweating
- seizures
- in rare cases, death
- Low potassium level. Symptoms can include:
- weakness
- fatigue (lack of energy)
- constipation
- muscle cramps
- heart palpitations (when your heart flutters or pounds)
What to do in case of overdose
If you think you’ve taken too much of this drug, call your doctor. You can also call the American Association of Poison Control Centers at 800-222-1222 or use their online tool. But if your symptoms are severe, call 911 or go to the nearest emergency room right away.
When you get Admelog from the pharmacy, the pharmacist will add an expiration date to the label on the medication. This date is typically 1 year from the date they dispensed the drug to you.
The expiration date helps guarantee the effectiveness of the medication during this time. The
Storage
How long a medication remains good can depend on many factors, including how and where you store the medication.
Unopened Admelog vials and SoloStar pens can be stored at room temperature (but kept below 86°F/30°C) for up to 28 days. However, they can be kept until their expiration date if they’re stored in the refrigerator at a temperature between 36°F and 46°F (2°C to 8°C).
Admelog vials and SoloStar pens shouldn’t be frozen. If the drug freezes, throw it away — don’t use it.
Once opened, Admelog vials can be stored for up to 28 days either at room temperature or in the refrigerator. However, opened Admelog pens should be stored at room temperature. They can also be kept for up to 28 days.
Be sure to store this medication away from light and heat. And throw away any vials and pens that have been opened for more than 28 days.
Disposal
Needles and pens that have been used should be discarded right away into a sharps container. You may be able to get a sharps container from your doctor, a local pharmacy, or an online store. If you can’t find a container that’s approved for sharps by the Food and Drug Administration (FDA), you can use a heavy-duty plastic container (such as a food storage container) instead.
If you no longer need to take Admelog and have leftover medication, it’s important to dispose of it safely. This helps prevent others, including children and pets, from taking the drug by accident. It also helps keep the drug from harming the environment.
The
The following information is provided for clinicians and other healthcare professionals.
Indications
Admelog is approved to improve glycemic control in:
- adults and children 3 years and older with type 1 diabetes
- adults with type 2 diabetes
Mechanism of action
Admelog contains the insulin analog called insulin lispro. Diabetes occurs due to inadequate glycemic control caused by either lack of insulin production or insulin resistance. Insulin and insulin analogs improve glycemic control by regulating cellular glucose uptake and decreasing hepatic glucose production. This lowers serum glucose levels within the body.
Pharmacokinetics and metabolism
Median time to maximum plasma concentration is 0.83 hours after administration of 0.3 unit/kg of Admelog. Insulin lispro with a strength of 100 units/mL has a bioavailability between 55% and 77% based on doses of 0.1 unit/kg and 0.2 unit/kg given by subcutaneous injection.
The average half-life of insulin lispro 100 units/mL is 0.85 hours for a 0.1-unit/kg dose and 0.92 hours with a 0.2-unit/kg dose.
Contraindications
Admelog is contraindicated:
- during episodes of hypoglycemia
- in people with hypersensitivity to insulin lispro or any other ingredients contained in the drug
Storage
Unopened Admelog vials and SoloStar pens can be stored at room temperature (but kept below 86°F/30°C) for up to 28 days. However, they can be kept until their expiration date if stored in the refrigerator at a temperature between 36°F and 46°F (2°C to 8°C).
Do not freeze Admelog. If Admelog is frozen, discard the medication. Admelog should be protected from light and heat.
Opened Admelog vials can be stored either in a refrigerator or at room temperature for up to 28 days. Opened Admelog pens should be stored at room temperature for up to 28 days.
Discard any unused or leftover medication 28 days after opening.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up-to-date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.