Copaxone is a brand-name prescription drug. It’s FDA-approved to treat certain forms of multiple sclerosis (MS) in adults.
With MS, your immune system mistakenly attacks your nerves. The damaged nerves then have trouble communicating with your brain. This condition can cause a wide variety of symptoms, such as muscle weakness and fatigue (lack of energy).
Specifically, Copaxone can be used to treat the following conditions:
- Clinically isolated syndrome (CIS). With CIS, you have an episode of MS-like symptoms that lasts at least 24 hours. CIS may or may not develop into MS.
- Relapsing-remitting MS (RRMS). With RRMS, you have periods when your MS symptoms relapse (flare up) followed by periods when your MS symptoms are in remission (improved or have gone away).
- Active secondary progressive MS (SPMS). With active SPMS, the condition steadily becomes worse, but you still have periods of relapse. During periods of relapse, your symptoms noticeably get worse for a while.
Drug details
Copaxone contains the active drug glatiramer acetate. It’s a disease-modifying therapy for MS. Copaxone helps to stop your immune system from attacking your nerves. The drug can reduce the number of MS relapses you have and also slow worsening of your disease.
Copaxone comes as a solution that’s given by subcutaneous injection (an injection under your skin). Your healthcare provider will show you or your caregiver how to administer the drug.
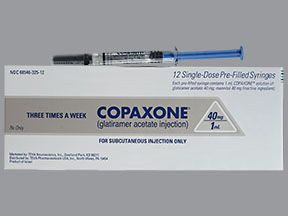
Copaxone comes in single-dose, prefilled syringes. It’s available in two strengths: 20 mg and 40 mg. The 20-mg injection is taken once each day, while the 40-mg injection is taken three times each week at least 48 hours apart.
Effectiveness
For information about the effectiveness of Copaxone, see the section “Copaxone for MS” below.
Copaxone contains the active drug glatiramer acetate. Generic forms of Copaxone are available, including the generic drug called Glatopa.
A generic drug is an exact copy of the active drug in a brand-name medication. The generic is considered to be as safe and effective as the original drug. Generics tend to cost less than brand-name drugs.
Copaxone can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Copaxone. These lists don’t include all possible side effects.
For more information on the possible side effects of Copaxone, talk with your doctor or pharmacist. They can give you tips on how to deal with any side effects that may be bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs it has approved. If you would like to report to the FDA a side effect you’ve had with Copaxone, you can do so through MedWatch.
How long do Copaxone side effects last?
The side effects that you may have from Copaxone, and how long they last, depend on how your body reacts to the drug.
Some side effects may last only a short while. For example, some people have a reaction called postinjection reaction right after receiving a Copaxone injection. This side effect can cause symptoms such as flushing, chest pain, and fast heart rate. If you have a postinjection reaction to Copaxone, your symptoms may last for up to 1 hour after taking your dose.
On the other hand, some side effects may be long-lasting. For example, some people have skin damage where they inject Copaxone into their skin. And in some cases, the skin damage caused by Copaxone injections can be permanent. (To help reduce the risk of skin damage, you should rotate injection sites when taking each of your Copaxone injections.)
To learn more about each of these side effects, see the “Side effect details” section below.
Mild side effects
Mild side effects of Copaxone can include:*
- injection site reaction, which may cause redness, pain, itching, lumps, or swelling in the area of your injection
- flushing
- skin rash
- shortness of breath
- anxiety, depression, or mood changes
- nausea and vomiting
- weakness
- infections, such as the common cold or flu
- pain in your back or other parts of your body
- heart palpitations (feeling like your heart is racing, fluttering, or pounding)
- sweating more than usual
- weight changes, including weight gain or weight loss
Most of these side effects may go away within a few days or a couple of weeks. But if they become more severe or don’t go away, talk with your doctor or pharmacist.
* This is a partial list of mild side effects from Copaxone. To learn about other mild side effects, talk with your doctor or pharmacist, or see the “Patient Information” section in Copaxone’s prescribing information.
Serious side effects
Serious side effects from Copaxone aren’t common, but they can occur. Call your doctor right away if you have serious side effects. But call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects of Copaxone include:
- Liver problems that may be severe, such as liver failure or hepatitis. Symptoms can include:
- pain in the right side of your upper abdomen (belly)
- yellowing of your skin or the whites of your eyes
- fatigue (lack of energy)
- Postinjection reaction (reactions that happen inside your body shortly after receiving a drug injection).*
- Skin damage at the site of your injection.*
- Chest pain.*
- Allergic reaction.*
* This serious side effect is explained further in the “Side effect details” section below.
Side effect details
You may wonder how often certain side effects occur with this drug. Here’s some detail on some of the side effects this drug may cause.
Depression
Some people may have depression while they’re taking Copaxone. In studies, some people taking Copaxone reported having depression. However, it’s not known how often this side effect occurred, or if it was caused by Copaxone.
However, a study found that Copaxone doesn’t increase the risk of depression in people with MS. And another study showed that Copaxone didn’t worsen depression symptoms in people who already had the condition.
It’s important to note that depression is common in people with multiple sclerosis (MS). For example, depression occurs in about 40% to 60% of people with MS at some point during their lifetime.
If you feel depressed while you’re taking Copaxone, talk with your doctor. There are many effective treatment options available that can help you manage the condition. And your doctor can recommend which treatment options are best for you.
Weight gain or weight loss
Some people taking Copaxone have had weight gain. In clinical studies, 3% of people who took the drug gained weight. In comparison, 1% of people who took a placebo (treatment with no active drug) gained weight.
However, weight gain can also be related to multiple sclerosis (MS), which Copaxone is used to treat. For example, two of the most common MS symptoms are fatigue (lack of energy) and trouble walking. And both of these symptoms can make you less active than usual, which may lead to weight gain.
It’s also important to note that corticosteroids, which are used to help treat flare-ups of MS symptoms, can also cause weight gain.
On the other hand, there have also been some reports of weight loss in people using Copaxone. However, these reports were rare. It’s not known how often weight loss occurs in people using Copaxone, or if the side effect is caused by Copaxone.
If you’re concerned about changes to your weight while you’re taking Copaxone, talk with your doctor. They can recommend diet and exercise tips to help you manage a body weight that’s healthy for you.
Injection site reactions, such as lumps or pain
The most common side effects of Copaxone are skin reactions that occur at the injection sites. These reactions may cause bruising, redness, swelling, lumps, pain, or itching.
In clinical studies, the following injection site reactions were reported:
- Redness. This side effect occurred in 22% to 43% of people who took Copaxone. In comparison, 2% to 10% of people who took a placebo (treatment with no active drug) had redness.
- Pain. This side effect occurred in 10% to 40% of people who took Copaxone. In comparison, 2% to 20% of people who took a placebo had pain.
- Itching. This side effect occurred in 6% to 27% of people who took Copaxone. In comparison, 0% to 4% of people who took a placebo had itching.
- Lumps. This side effect occurred in 6% to 26% of people who took Copaxone. In comparison, 0% to 6% of people who took a placebo had lumps.
- Swelling. This side effect occurred in 6% to 19% of people who took Copaxone. In comparison, 0% to 4% of people who took a placebo had swelling.
During studies, injection site reactions were more common in people who took Copaxone 20 mg daily than they were in people who took Copaxone 40 mg three times a week.
If you have an injection site reaction to Copaxone, the reaction should ease within a few days. But if it doesn’t or your symptoms are severe, call your doctor.
Skin damage at the injection site
Rarely, Copaxone injections can cause skin damage at the site of your injections. In some cases, the skin damage caused by Copaxone injections can be permanent.
Examples of skin damage that may occur with Copaxone include:
- Lipoatrophy. With lipoatrophy, the fatty layer under your skin is damaged. This damage can cause permanent pits to form on your skin. In clinical studies, lipoatrophy occurred in 2% of people who took Copaxone 20 mg daily. And it occurred in 0.5% of people who took Copaxone 40 mg three times a week. No one who took a placebo (treatment with no active drug) had lipoatrophy.
- Skin necrosis. With skin necrosis, some of your skin cells die. This condition may cause areas of your skin to look brown or black. This is a rare side effect that’s only been reported since Copaxone was released onto the market. And it’s not known exactly how often the condition happens in people using Copaxone.
You can reduce your risk of both lipoatrophy and skin necrosis by carefully following your healthcare provider’s instructions for Copaxone injections. For example, it’s important that you don’t inject your doses into the same place on your body for each dose. Instead, you should rotate your injection sites each time you take a dose of Copaxone.
If you have concerns about skin damage while you’re using Copaxone, talk with your doctor.
Postinjection reaction
Some people have a reaction from Copaxone right after receiving an injection of the drug. This side effect is called a postinjection reaction. It can cause symptoms including:
- flushing
- chest pain
- fast heart rate
- heart palpitations (feeling like your heart is racing, fluttering, or pounding)
- trouble breathing
- tightness in your throat
- anxiety
- urticaria (itchy hives)
Symptoms of postinjection reaction usually improve within 1 hour after your injection. If your symptoms last longer than this, or they’re severe, call your doctor right away. But if your symptoms feel life threatening, call 911.
Some people only have a postinjection reaction after their first injection of Copaxone. But other people might have a reaction after each injection of the drug. It’s also possible to start having these reactions after you’ve received Copaxone injections in the past with no problems.
If you’re concerned about having a postinjection reaction with Copaxone, talk with your doctor.
How common is postinjection reaction?
In clinical studies, about 16% of people who took Copaxone 20 mg daily had a postinjection reaction. In comparison, 4% of people who took a placebo (treatment with no active drug) had a postinjection reaction.
Post injection reactions were less common in people who took Copaxone 40 mg three times a week. For example, during a clinical study, 2% of these people had a postinjection reaction. In this particular study, no one taking a placebo had a postinjection reaction.
Allergic reaction
As with most drugs, some people can have an allergic reaction after taking Copaxone. But it’s not known how often allergic reactions occur in people using this drug.
Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (warmth and redness in your skin)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
Call your doctor right away if you have a severe allergic reaction to Copaxone. But call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Chest pain
It’s possible to have chest pain as part of a postinjection reaction to Copaxone. With a postinjection reaction, you have certain symptoms, such as chest pain, right after taking a dose of Copaxone. (See the section above for information on postinjection reactions.)
However, some people taking Copaxone have chest pain that doesn’t happen right after receiving an injection of the drug. And chest pain following Copaxone injections doesn’t always occur with other symptoms.
In clinical studies, about 13% of people who took Copaxone 20 mg daily had chest pain. And about 2% of people who took Copaxone 40 mg three times a week had chest pain. In comparison, chest pain was reported in 1% to 6% of people who took a placebo (treatment with no active drug). In the studies, some of this chest pain was related to postinjection reactions. But in many cases, it wasn’t related to postinjection reactions.
If you have chest pain while you’re taking Copaxone, it should go away quickly. However, if you have pain that either lasts longer than a few minutes or is severe, call your doctor right way. And if your pain feels life threatening, call 911.
Hair loss (not a side effect)
Hair loss wasn’t seen in people who took Copaxone during initial clinical studies.
However, hair loss is a common side effect of immunosuppressant drugs,* which are sometimes used to treat multiple sclerosis (MS). These drugs include mitoxantrone and cyclophosphamide. But keep in mind that Copaxone isn’t an immunosuppressant drug.
If you’re concerned about hair loss while you’re taking Copaxone, talk with your doctor. They can help you find ways to manage this side effect.
* Immunosuppressant drugs suppress (weaken) the activity of your immune system.
As with all medications, the cost of Copaxone can vary. The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
Your insurance plan may require you to get prior authorization before approving coverage for Copaxone. This means that your doctor and insurance company will need to communicate about your prescription before the insurance company will cover the drug. The insurance company will review the request and let you and your doctor know if your plan will cover Copaxone.
If you’re not sure if you’ll need to get prior authorization for Copaxone, contact your insurance company.
Financial and insurance assistance
If you need financial support to pay for Copaxone, or if you need help understanding your insurance coverage, help is available.
Teva Neuroscience, Inc., the manufacturer of Copaxone, offers a program called Shared Solutions. This program offers financial assistance, including a copay card that may help lower the cost of Copaxone.
For more information and to find out if you’re eligible for support, call 800-887-8100 or visit the program website.
Generic version
Copaxone is available in a generic form called glatiramer acetate. A generic drug is an exact copy of the active drug in a brand-name medication. The generic is considered to be as safe and effective as the original drug. And generics tend to cost less than brand-name drugs. The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
If your doctor has prescribed Copaxone and you’re interested in using generic glatiramer acetate instead, talk with your doctor. They may have a preference for one version or the other. You’ll also need to check your insurance plan, as it may only cover one or the other.
You should take Copaxone according to your doctor’s or healthcare provider’s instructions.
Copaxone is taken by subcutaneous injection (an injection under your skin). Your healthcare provider will teach you or your caregiver how to administer the drug. And when you’re just starting Copaxone treatment, your doctor or nurse will help give you your first injection.
Copaxone comes as a solution inside single-dose, prefilled syringes that have a needle attached. If you’re not comfortable using these syringes, ask your doctor about a special device, called the autoject 2 for glass syringe.
To use the autoject 2 device, you’ll place a prefilled Copaxone syringe inside the device. The autoject 2 hides the syringe’s needle and allows you to inject the drug by pressing a button, instead of pushing down on the syringe’s plunger.
Instructions for injecting Copaxone doses are provided in the paper leaflet that comes from your pharmacy with Copaxone.
In addition, the drug’s manufacturer also provides an injection guide and a step-by-step instructional video. These resources explain more about how to use Copaxone syringes and the autoject 2 device. And they explain the injection depth settings you should choose when using the autoject 2 device.
Copaxone injection sites
You can inject Copaxone under the skin of the following areas of your body:
- your abdomen (belly), if you avoid injecting into the area that’s within 2 inches of your belly button
- the front of your thighs, if you inject into the area that’s about 2 inches above your knee and 2 inches below your groin
- the back of your hips below your waist
- the back of your upper arms
Talk with your doctor about which of these injection areas is best for you. Keep in mind that each time you inject a dose of Copaxone, you should rotate the injection sites you use. Don’t use the same injection site more than once a week.
It’s helpful to keep a record of the injection sites you use for each dose of Copaxone. In fact, there’s a Copaxone tracker app available on the manufacturer’s website that can help you do this.
Tips for taking Copaxone
When using Copaxone, keep the following tips in mind:
- Take Copaxone out of the refrigerator about 20 minutes before you plan to inject your dose. This gives the drug time to warm up to room temperature, which makes the injection more comfortable for you.
- Copaxone injections should only be given under your skin. Don’t inject this drug into one of your veins or muscles.
- Don’t inject Copaxone into areas of your skin that are red, swollen, lumpy, scarred, or pitted. And avoid giving injections in areas of skin with birthmarks, stretch marks, or tattoos.
- Don’t rub or massage your Copaxone injection site for at least 24 hours after you’ve injected the drug.
When to take
When you’ll take Copaxone depends on which strength of the drug you’re using. Dosage schedules for Copaxone are as follows:
- Copaxone 20 mg. If you’re using this strength, you’ll inject the drug once a day, at the same time each day. It doesn’t matter what time you choose, as long as you’re consistent each day.
- Copaxone 40 mg. If you’re using this strength, you’ll inject the drug three times each week. For example, you could do your injections on Monday, Wednesday, and Friday. Just make sure the injections are taken at least 48 hours apart.
To help make sure that you don’t miss a dose, try setting a reminder on your phone. Reminders can also be set in the Copaxone tracker app.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to fit your needs.
Drug forms and strengths
Copaxone comes as single-dose, prefilled syringes. It’s available in two strengths: 20 mg and 40 mg.
Dosage for MS
Copaxone has the following recommended dosages for multiple sclerosis (MS):
- 20 mg taken once a day
- 40 mg taken three times a week
Your doctor may prescribe either of these dosage schedules, depending on which one is best for your unique situation.
What if I miss a dose?
What to do if you miss a Copaxone dose depends on which dosage of the drug you’re taking. Below, we describe what to do for each recommended dosage.
You can also call your doctor’s office if you miss a dose of Copaxone and you’re not sure what to do. Your doctor or their medical staff can recommend when you should take your next dose of the drug.
And to help make sure that you don’t miss a dose, try setting a reminder on your phone, or use the Copaxone tracker app.
Missed dose of Copaxone 20 mg daily
If you typically take Copaxone 20 mg daily, take the missed dose as soon as you remember. But if it’s closer to your next scheduled dose than it is to the missed dose, skip the missed dose and continue with your usual dosing schedule. Don’t take two doses together to make up for the missed dose.
Missed dose of Copaxone 40 mg three times a week
If you typically take Copaxone 40 mg and you miss a dose, take it the following day at your usual time. Then take your next dose 2 days later at your usual time. Try to go back to your typical schedule the following week. But remember, there should always be at least 48 hours between your doses.
For example, if you usually take Copaxone on Monday, Wednesday, and Friday, but you miss your Monday dose, take your missed dose on Tuesday. Then take the rest of your doses for that week on Thursday and Saturday. The following week, you can go back to your typical schedule.
Will I need to use this drug long term?
Copaxone is meant to be used as a long-term treatment. If you and your doctor determine that Copaxone is safe and effective for you, you’ll likely take it long term.
The Food and Drug Administration (FDA) approves prescription drugs such as Copaxone to treat certain conditions. Copaxone may also be used off-label for other conditions. Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.
Copaxone is FDA-approved to treat relapsing forms of multiple sclerosis (MS) in adults. The drug is also approved to treat clinically isolated syndrome (CIS) in adults. (CIS is a condition that causes MS-like symptoms.)
Specifically, Copaxone can be used to treat the following conditions:
- CIS. With CIS, you have an episode of MS-like symptoms that lasts at least 24 hours. CIS may or may not develop into MS.
- Relapsing-remitting MS (RRMS). With this form of MS, you have periods when your MS symptoms relapse (flare up) followed by periods when your MS symptoms are in remission (improved or have gone away).
- Active secondary progressive MS (SPMS). With this form of MS, your condition steadily becomes worse, but you still have periods of relapse. During periods of relapse, your symptoms noticeably get worse for a while.
With MS, your immune system mistakenly attacks your nerves. The damaged nerves then have trouble communicating with your brain. This condition can cause a wide variety of symptoms, depending on which nerves are damaged.
With relapsing forms of MS, you have episodes of nerve damage that cause new MS symptoms. Or you may have periods when your MS symptoms come back or get worse after they had improved.
Copaxone is a disease-modifying therapy. It works to treat MS and CIS by helping to stop your immune system from attacking your nerves. By doing this, the drug can reduce the number of MS relapses you have and also slow the worsening of your disease.
Effectiveness for MS
In several clinical studies, Copaxone was effective in treating relapsing-remitting forms of MS. Specifically, Copaxone reduced the number of MS relapses people had. And the drug decreased the number of brain lesions (areas of nerve damage) the people had from the disease. Copaxone also slowed MS from worsening in people using the drug.
For example, two studies looked at the effect of using Copaxone 20 mg daily in people with MS. Over 2 years of treatment:
- People who took Copaxone had an average of 0.6 to 1.19 MS relapses. In comparison, people who took a placebo (treatment with no active drug) had an average of 1.68 to 2.4 MS relapses.
- 34% to 56% of people who took Copaxone didn’t have any MS relapses. In comparison, 27% to 28% of people who took a placebo didn’t have any MS relapses.
In addition, one study looked at the effect of using Copaxone 20 mg daily on the development of certain brain lesions. These lesions, which indicated areas of inflammation in the brain, were identified with MRI scans. Over 9 months of treatment:
- half of the people who took Copaxone developed at least 11 new lesions
- half of the people who took a placebo developed at least 17 new lesions
Another study looked at the effect of using Copaxone 40 mg three times a week in people with MS. Over 1 year of treatment, compared with people using a placebo, people using Copaxone had:
- 34% lower risk of MS relapses
- 45% lower risk of brain lesions that showed inflamed areas in their brain
- 35% lower risk of new or growing brain lesions that showed damaged areas in their brain
Effectiveness for CIS
A clinical study looked at Copaxone treatment in people with CIS. In this study, Copaxone reduced the people’s risk of having a second episode of MS-like symptoms.
Over 3 years of treatment, people who took Copaxone 20 mg daily were 45% less likely to have a second episode of MS-like symptoms than were people who took a placebo.
Copaxone and children
Copaxone isn’t approved for use in children ages 17 years or younger. However, the drug is sometimes used off-label to treat MS in children. (With off-label use, a drug that’s approved for certain conditions is used for other conditions.)
Some research has shown that glatiramer (the active drug in Copaxone) can reduce the number of MS relapses in children. The research also showed that the drug slowed worsening of disability caused by MS. In addition, the International Pediatric Multiple Sclerosis Study Group recommends using Copaxone as one of the first treatment options in children with MS.
If you have questions about using Copaxone to treat MS in a child, talk with your doctor.
Other drugs are available that can treat multiple sclerosis (MS), as well as clinically isolated syndrome (CIS). (CIS is a condition that causes MS-like symptoms.)
Some alternative drugs may be a better fit for you than others. If you’re interested in finding an alternative to Copaxone, talk with your doctor. They can tell you about other medications that may work well for you.
Examples of other drugs that may be used to treat either MS or CIS include:
- corticosteroids, which are used to treat MS symptom flare-ups or CIS episodes, such as:
- methylprednisolone (Medrol)
- prednisone (Rayos)
- disease-modifying therapies that are taken by mouth, such as:
- dimethyl fumarate (Tecfidera)
- diroximel fumarate (Vumerity)
- fingolimod (Gilenya)
- siponimod (Mayzent)
- teriflunomide (Aubagio)
- disease-modifying therapies that are taken by self-injection, such as:
- glatiramer acetate (Glatopa)
- interferon beta-1b (Betaseron, Extavia)
- pegylated interferon beta-1a (Plegridy)
- disease-modifying therapies that are given intravenously (injected into your vein), such as:
- alemtuzumab (Lemtrada)
- natalizumab (Tysabri)
- ocrelizumab (Ocrevus)
You may wonder how Copaxone compares with other medications that are prescribed for similar uses. Here we look at how Copaxone and Glatopa are alike and different.
Ingredients
Copaxone and Glatopa both contain the same active drug: glatiramer acetate.
However, while Copaxone is a brand-name medication, Glatopa is a generic form of Copaxone. A generic drug is an exact copy of the active drug in a brand-name medication.
Uses
Copaxone and Glatopa are both approved to treat certain forms of multiple sclerosis (MS) in adults.
Specifically, Copaxone and Glatopa can be used to treat the following conditions:
- clinically isolated syndrome (CIS)
- relapsing-remitting MS (RRMS)
- active secondary progressive MS (SPMS)
Copaxone and Glatopa are both called disease-modifying drugs. They work by helping to stop your immune system from attacking your nerves. These drugs can reduce the number of MS relapses you have and also slow your disease from worsening.
Drug strengths and forms
Both Copaxone and Glatopa come as solutions inside single-dose, prefilled syringes. They’re each given by subcutaneous injection (an injection under your skin). Depending on the strength of the drug your doctor prescribes for you, you’ll take each medication either once each day or three times each week.
Your healthcare provider will teach you or your caregiver how to inject either drug.
Effectiveness and safety
The Food and Drug Administration (FDA) considers generics to be just as safe and effective as the original drug. This means that Glatopa is considered just as effective in treating MS and CIS as Copaxone is. It also means that Copaxone and Glatopa can both cause the same side effects.
To learn about the mild and serious side effects of Copaxone, see the section “Copaxone side effects” above.
Costs
Copaxone is a brand-name drug, while Glatopa is a generic version of Copaxone. Brand-name medications usually cost more than generics do.
Glatopa costs significantly less than Copaxone costs. But the actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
You may wonder how Copaxone compares with other medications that are prescribed for similar uses. Here we look at how Copaxone and Tecfidera are alike and different.
Ingredients
Copaxone contains glatiramer acetate, while Tecfidera contains dimethyl fumarate.
Uses
Copaxone and Tecfidera are both approved to treat certain forms of multiple sclerosis (MS) in adults.
Specifically, Copaxone and Tecfidera can be used to treat the following conditions:
- clinically isolated syndrome (CIS)
- relapsing-remitting MS (RRMS)
- active secondary progressive MS (SPMS)
Copaxone and Tecfidera are both called disease-modifying drugs. They work by helping to stop your immune system from attacking your nerves. These drugs can reduce the number of MS relapses you have and also slow your disease from worsening.
Drug forms and administration
Copaxone comes as a solution inside single-dose, prefilled syringes. It’s taken by subcutaneous injection (an injection under your skin). Depending on the strength of the drug your doctor prescribes, it can be taken either once each day or three times each week. Your healthcare provider will teach you or your caregiver how to administer the drug.
Tecfidera, on the other hand, comes as capsules that are taken by mouth. It’s taken twice each day.
Side effects and risks
Copaxone and Tecfidera both contain a disease-modifying drug. However, these drugs work in different ways in your body. Copaxone and Tecfidera can cause some similar and some different side effects. Below are examples of these side effects.
Mild side effects
These lists contain up to 10 of the most common mild side effects that can occur with Copaxone, with Tecfidera, or with both Copaxone and Tecfidera (when taken individually).
- Can occur with Copaxone:
- injection site reactions, which may cause redness, pain, itching, lumps, or swelling in the area of your injection
- anxiety
- weakness
- infections, such as the common cold and flu
- pain in your back or other parts of your body
- heart palpitations (feeling like your heart is racing, fluttering, or pounding)
- sweating more than usual
- weight changes, including weight gain or weight loss
- Can occur with Tecfidera:
- abdominal (belly) pain
- diarrhea
- indigestion
- Can occur with both Copaxone and Tecfidera:
- flushing
- nausea and vomiting
- skin rash
Serious side effects
These lists contain examples of serious side effects that can occur with Copaxone, with Tecfidera, or with both drugs (when taken individually).
- Can occur with Copaxone:
- postinjection reaction (reactions that happen inside your body shortly after receiving a drug injection)
- skin damage at the site of your injections
- Can occur with Tecfidera:
- lymphopenia (decreased level of white blood cells called lymphocytes)
- progressive multifocal leukoencephalopathy (PML), which is a life threatening infection in your brain
- other serious infections, such as shingles (an infection that’s caused by the herpes zoster virus)
- Can occur with both Copaxone and Tecfidera:
- liver problems that may be severe, such as liver failure or hepatitis
- severe allergic reaction
Effectiveness
Copaxone and Tecfidera are both approved to treat certain forms of MS as well as CIS. These drugs haven’t been directly compared in clinical studies. But separate studies have found both Copaxone and Tecfidera to be effective in treating these conditions.
One review of studies found that Tecfidera was more effective than Copaxone in reducing the number of MS relapses and slowing the worsening of disability caused by MS.
In addition, some research has found Tecfidera more effective than Copaxone in reducing the number of MS relapses. However, this research found the drugs were similarly effective in slowing the worsening of disability caused by MS.
If you’re interested in taking one of these drugs for MS, talk with your doctor. They can recommend which medication would be best for you.
Costs
Copaxone and Tecfidera are both brand-name drugs. Copaxone is also available in generic form. There are currently no generic forms of Tecfidera available. Brand-name medications usually cost more than generics.
The actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
Here are answers to some frequently asked questions about Copaxone.
Is Copaxone an immunosuppressant?
No, it isn’t. Immunosuppressant drugs suppress (weaken) the activity of your immune system. Instead, Copaxone is called an immunomodulator. It works by changing the activity of certain cells in your immune system to reduce the symptoms of multiple sclerosis (MS). This can slow the worsening of your condition and increased disability. For information on how Copaxone works to treat MS, see the “How Copaxone works” section below.
Certain other drugs used to treat MS are immunosuppressant drugs. These drugs include mitoxantrone and cyclophosphamide. But Copaxone isn’t an immunosuppressant.
Will I have withdrawal symptoms or side effects after stopping Copaxone?
No, that’s unlikely. Withdrawal symptoms are side effects that can happen when you stop taking a drug that your body has become dependent on. (With dependence, your body needs the drug in order to feel normal.)
Stopping Copaxone isn’t known to cause any withdrawal symptoms. Because of this, you don’t need to stop taking the drug gradually, as you do with certain drugs that can cause withdrawal symptoms.
However, keep in mind that stopping Copaxone could cause your multiple sclerosis (MS) to relapse or become worse.
If you have questions about stopping Copaxone, talk with your doctor. They can discuss with you the risks and benefits of stopping this drug.
Does using Copaxone increase my risk of cancer?
No. It’s currently thought that there’s no increased risk of cancer with Copaxone use. While there were some reports of cancer in people taking the drug after it was released onto the market, these reports were rare. And increased risk of cancer hasn’t been directly linked to Copaxone use.
However, certain other drugs used to treat multiple sclerosis (MS), such as those that cause immunosuppression, may increase the risk of cancer. Examples of these other drugs include alemtuzumab (Lemtrada) and mitoxantrone.
Normally, your immune system kills germs, as well as cells in your body that are abnormal or not working right. This action helps to protect you from developing cancers and infections. But with immunosuppression, your immune system is suppressed (weakened) and doesn’t work as well as it should. If your immune system is suppressed, you have a higher risk of developing certain cancers and infections.
Copaxone does make some parts of your immune system less active than usual. However, Copaxone is called an immunomodulator, rather than an immunosuppressant. That’s because Copaxone changes the way your immune system works, rather than suppresses your immune system.
If you have questions about the risks of Copaxone treatment, talk with your doctor.
Is Copaxone a biologic?
No, Copaxone isn’t a biologic. Biologics are drugs that are made from living cells. Copaxone is made from chemicals.
Some of the disease-modifying therapies used to treat multiple sclerosis (MS) are biologics, but Copaxone isn’t one of them. Examples of biologics used to treat MS include alemtuzumab (Lemtrada), natalizumab (Tysabri), and ocrelizumab (Ocrevus).
For information on how Copaxone works to treat MS, see the “How Copaxone works” section below.
How long can you take Copaxone?
Copaxone is meant to be used as a long-term treatment. In general, you can keep taking it for as long as it continues to be safe and effective for you.
But if you develop bothersome or severe side effects, or the drug doesn’t control your condition well enough, you might need to switch to a different treatment. In that case, your doctor will recommend an alternative treatment for you.
If you have questions about how long you should take Copaxone, talk with your doctor.
Can I donate blood if I’m taking Copaxone?
Yes. According to the American Red Cross, taking Copaxone shouldn’t prevent you from giving blood. And it’s also fine to give blood if you have multiple sclerosis (MS), as long as your condition is well managed and you’re currently in good health.
If you have questions about whether it’s safe for you to donate blood, talk with your doctor. Or you can contact the American Red Cross by visiting their website.
When you get Copaxone from your pharmacy, your pharmacist will add an expiration date to the box of syringes and on the syringes themselves. This date is typically 1 year from the date they dispensed the medication. The expiration date helps guarantee that the medication is effective to use during a certain period of time.
The
Storage
How long a medication remains good can depend on many factors, including how and where you store the medication.
Copaxone prefilled syringes should be stored in a refrigerator at a temperature of 36°F to 46°F (2°C to 8°C). Don’t freeze Copaxone syringes. If a syringe does become frozen, don’t use it. Instead, dispose of the syringe in a sharps container.
If you’re unable to refrigerate Copaxone, such as when you’re travelling, you can store the drug at room temperature (59°F to 86°F/15°C to 30°C). However, you can only store Copaxone at room temperature for up to 1 month. And while the drug is being stored outside of the refrigerator, make sure the temperature doesn’t rise above 86°F (30°C).
Whether you’re storing Copaxone in a refrigerator or at room temperature, you should keep the syringes in their individual blister packs, inside their original carton. Doing this will protect the drug from light.
Disposal
Right after you’ve used a syringe, needle, or autoinjector, dispose of it in an
This article provides several useful tips on medication disposal. You can also ask your pharmacist for information on how to dispose of your medication.
Copaxone hasn’t been studied in pregnant women. So it’s not known for sure if the drug is safe to take during pregnancy.
Some women have taken Copaxone during pregnancy. But there’s not enough information available to say whether the drug increases the risks of birth defects or miscarriage.
Animal studies have been done in pregnant females who were given Copaxone. And these studies didn’t show any harm to fetuses when the drug was used. But keep in mind that studies done in animals don’t always predict what will happen in humans.
If you’re pregnant or may become pregnant, talk with your doctor about whether Copaxone is right for you. And if you’re already taking Copaxone and you become pregnant, be sure to call your doctor right away.
It’s not known if Copaxone is safe to take during pregnancy. If you’re sexually active and you or your partner can become pregnant, talk with your doctor about your birth control needs while you’re using Copaxone.
It’s not known whether Copaxone passes into breast milk or if it can affect a child who’s breastfed.
If you’re breastfeeding or planning to breastfeed, talk with your doctor about whether Copaxone is right for you.
Alcohol isn’t known to interact with Copaxone. However, if you have certain side effects from Copaxone, such as flushing or nausea, drinking alcohol could worsen your side effects.
After Copaxone was released onto the market, there were some reports of people using the drug having intolerance to alcohol. (With alcohol intolerance, you may have certain reactions right after consuming alcohol. These reactions could include flushing in your face or having a stuffy nose.)
However, these reports were rare. And having intolerance to alcohol hasn’t been directly linked to Copaxone use.
The risks of alcohol use in people with multiple sclerosis (MS) aren’t known for sure. If you drink alcohol, talk with your doctor about how much is safe for you to consume.
There aren’t any known interactions between Copaxone and any other medications, herbs, supplements, or foods.
However, before taking Copaxone, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Copaxone is approved to treat relapsing forms of multiple sclerosis (MS) and clinically isolated syndrome (CIS). (CIS is a condition that causes MS-like symptoms.)
What happens in MS?
MS is a long-term condition that gets worse over time. It affects your central nervous system (CNS), which is made up of your brain and spinal cord. Your CNS is also made up of nerves that send messages between your brain and the rest of your body.
Each of these nerve fibers is surrounded by a protective layer of tissue called a myelin sheath. The myelin sheath is like the plastic coating that surrounds wires inside an electrical cable. If the sheath is damaged, your nerves can’t conduct messages as well.
With MS, your immune system starts mistakenly attacking myelin sheaths surrounding your nerves. This causes inflammation that damages the myelin sheaths. The damage makes it harder for your nerves to send and receive messages. Depending on which nerves are damaged, your symptoms of MS can vary quite a bit.
After your immune system attacks your myelin sheath, scar tissue can develop around the damaged areas. The scar tissue also makes it difficult for your nerves to send and receive messages. The areas of damage and scarring on your nerves are called lesions. These areas can be seen on MRI scans, which are imaging tests used to monitor MS.
What is relapsing MS?
With relapsing forms of MS, you’ll have periods of time when your symptoms get better or even go away completely. (These periods are called remission.) But you’ll also have periods of new MS symptoms, or periods when your MS symptoms come back or get worse after they improved. (These periods are called relapses.)
Remission happens when your nerve cells repair themselves from the damage that’s caused by MS. Remission can also happen when your body makes new nerve pathways that bypass nerves that have been damaged by MS. Periods of remission can last from a few months up to a few years.
Each episode of nerve damage and its resulting symptoms can last for a few days or a few months. This is called an MS attack or MS relapse. Over time, the relapse symptoms may worsen or become more frequent. This worsening leads to difficulty in everyday tasks such as walking or speaking.
What is CIS?
With CIS, you have a single episode of MS-like symptoms that lasts for at least 24 hours. CIS may or may not progress to MS, but it can be a sign of possible MS. Because of this, it’s usually grouped with other conditions, such as relapsing forms of MS.
What does Copaxone do?
Copaxone is a disease-modifying therapy for relapsing forms of MS, as well as CIS. It slows down nerve damage that’s caused by MS and also slows worsening of the disease.
Copaxone contains the active drug glatiramer acetate. It’s a protein that’s made in a lab. However, it’s very similar to one of the proteins that’s naturally found in your body’s myelin tissue.
Copaxone is called an immunomodulator. It works by changing the activity of certain cells in your immune system. Although it’s not fully understood how the drug works, it’s thought that it activates certain white blood cells, called suppressor T cells. These cells work in several ways to stop your immune system from attacking your myelin sheath tissue.
With fewer attacks to your myelin sheath, you should have fewer MS relapses. This can slow the worsening of your condition and increased disability.
How long does it take to work?
Copaxone will start to work soon after your first injection, but you’re unlikely to notice that it’s working. This is because the drug helps to prevent your condition from getting worse, rather than treating your current symptoms.
But during treatment, your doctor may check to see if Copaxone is working for you. To do this, they may order certain imaging tests, such as an MRI scan.
Before taking Copaxone, talk with your doctor about your health history. Copaxone may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Allergy to Copaxone. Do not take Copaxone if you’ve ever had an allergic reaction to Copaxone, glatiramer acetate (the active drug in Copaxone), or mannitol (an inactive ingredient in Copaxone). If you’re unsure about your medication allergies, talk with your doctor.
- Pregnancy. It’s not known if Copaxone is safe to use during pregnancy. For more information, please see the “Copaxone and pregnancy” section above.
- Breastfeeding. It’s not known if Copaxone passes into breast milk. For more information, please see the “Copaxone and breastfeeding” section above.
Note: For more information about the potential negative effects of Copaxone, see the “Copaxone side effects” section above.
Do not use more Copaxone than your doctor recommends. For some drugs, doing so may lead to unwanted side effects or overdose.
What to do in case you’ve taken too much Copaxone
If you think you’ve taken too much of this drug, call your doctor. You can also call the American Association of Poison Control Centers at 800-222-1222 or use their online tool. But if your symptoms are severe, call 911 or go to the nearest emergency room right away.
The following information is provided for clinicians and other healthcare professionals.
Indications
Copaxone is approved to treat the following conditions in adults:
- clinically isolated syndrome (CIS)
- relapsing-remitting MS (RRMS)
- active secondary progressive MS (SPMS)
Mechanism of action
Copaxone is a disease-modifying therapy that contains the active drug glatiramer acetate. It is an immunomodulating drug, although its mechanism of action is not fully understood.
Glatiramer acetate is a synthetic protein molecule that is similar to one of the natural proteins found in myelin. It appears to activate T suppressor cells that suppress the immune response to myelin.
Glatiramer thereby reduces the immune attack on myelin, resulting in both fewer MS relapses and slowed progression of the disease.
Pharmacokinetics and metabolism
A significant amount of Copaxone is hydrolyzed in the subcutaneous tissue after administration. Both intact and hydrolyzed Copaxone enter the lymphatic and systemic circulation. The half-life of Copaxone is not known.
Contraindications
Copaxone must not be used in people with a known allergy to either glatiramer acetate or mannitol.
Storage
Store Copaxone in the refrigerator at a temperature of 36°F to 46°F (2°C to 8°C). Keep the medication in the original packaging. Do not freeze. If a Copaxone syringe has become frozen, do not use it.
If needed, Copaxone can be kept at room temperature (59°F to 86°F/15°C to 30°C) for up to 1 month.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.