Mylotarg is a brand-name prescription medication that’s used to treat certain types of acute myeloid leukemia (AML). AML is a cancer that affects myeloid cells, which are cells in your bone marrow. These cells normally develop into red blood cells, white blood cells, and platelets.
Specifically, Mylotarg is used to treat AML that’s CD33-positive. This means the cancer cells have high levels of a protein called CD33 on their surface. Most cases of AML are CD33-positive.
Mylotarg is used to treat CD33-positive AML that’s:
- Newly diagnosed. For this purpose, Mylotarg is used in adults and in children ages 1 month and older.
- Relapsed* or refractory.* For this purpose, Mylotarg is used in adults and in children ages 2 years and older.
* Relapsed cancer has returned after remission, which is a decrease in cancer symptoms. Refractory cancer hasn’t responded to previous cancer treatments.
Drug details
Mylotarg is a targeted therapy for AML. Targeted therapies are treatments that act very precisely on cancer cells.
Mylotarg contains a monoclonal antibody attached to a chemotherapy drug. Monoclonal antibodies are drugs made from immune system cells. These drugs attach to specific proteins on cells. Mylotarg attaches to the CD33 protein on the cancerous myeloid cells. It delivers the chemotherapy directly into these cells.
Mylotarg is given by intravenous (IV) infusion. An IV infusion is an injection into a vein that’s given over a period of time. Mylotarg infusions typically last about 2 hours.
You’ll receive these infusions at your doctor’s office, a hospital, or an infusion center. Mylotarg can be used on its own or with other chemotherapy drugs.
Effectiveness
For information about the effectiveness of Mylotarg, see the “Mylotarg for AML” section below.
Mylotarg is a biologic drug that’s available only as a brand-name medication. It’s not currently available in a biosimilar form.
A biologic drug is made from living cells, while other drugs are made from chemicals. Drugs made from chemicals can have generics, which are exact copies of the active drug in the brand-name medication. Biologics, on the other hand, can’t be copied exactly. Therefore, instead of a generic, biologics have biosimilars. Biosimilars are “similar” to the parent drug, and they’re considered to be just as effective and safe.
Like generics, biosimilars usually cost less than brand-name drugs.
The Food and Drug Administration (FDA) approves prescription drugs such as Mylotarg to treat certain conditions. Mylotarg may also be used off-label for other conditions. Off-label drug use means using a drug for a purpose other than what it’s been approved for by the FDA.
Mylotarg is FDA-approved to treat a certain type of acute myeloid leukemia (AML), which is cancer that affects myeloid cells. (See “About AML” below to learn more.)
Specifically, Mylotarg treats AML that’s CD33-positive. This means the cancer cells have high levels of a protein called CD33 on their surface. Most cases of AML are CD33-positive.
Mylotarg is used to treat CD33-positive AML that’s:
- Newly diagnosed. For this purpose, Mylotarg is used in adults and in children ages 1 month and older.
- Relapsed* or refractory.* For this purpose, Mylotarg is used in adults and in children ages 2 years and older.
* Relapsed cancer has returned after remission, which is a decrease in cancer symptoms. Refractory cancer hasn’t responded to previous cancer treatments.
About AML
AML is a type of cancer that affects myeloid cells, which are cells in your bone marrow. (Bone marrow is the spongy material inside your bones, where your blood cells are made.)
Myeloid cells normally develop into red blood cells, white blood cells, and platelets. These move from your bone marrow into your bloodstream when needed. But with AML, the myeloid cells develop an abnormality that stops them from growing into normal, mature blood cells.
Instead, they develop into immature cells called blasts. The blasts don’t function as normal blood cells. And they take up lots of space in your bone marrow, leaving less space for healthy blood cells to develop.
AML leads to low levels of white blood cells, red blood cells, and platelets in your blood.
- White blood cells usually fight infection, so with AML you may experience frequent infections and fever.
- Red blood cells usually carry oxygen throughout your body, so with AML you may have fatigue (lack of energy) and shortness of breath. You may also have paleness of your skin, gums, or nail beds.
- Platelets help your blood to clot, so with AML you may bruise or bleed more easily than usual.
Mylotarg is used to treat a specific type of AML called CD33-positive AML. With this kind of AML, the cancer cells have high levels of a particular protein called CD33 on their surface. Most cases of AML are CD33-positive.
Mylotarg is used to treat CD33-positive AML that’s:
- Newly diagnosed. For this purpose, Mylotarg is used in adults and in children ages 1 month and older.
- Relapsed* or refractory.* For this purpose, Mylotarg is used in adults and in children ages 2 years and older.
* Relapsed cancer has returned after remission, which is a decrease in cancer symptoms. Refractory cancer hasn’t responded to previous cancer treatments.
Effectiveness for AML
Mylotarg has been found to be effective for treating AML. It’s included as a treatment option for this type of cancer in guidelines from the National Comprehensive Cancer Network. For information on how the drug performed in clinical studies, see the prescribing information for Mylotarg.
Mylotarg and children
Mylotarg is FDA-approved to treat CD33-positive AML in children. It’s approved for use in children ages 1 month and older with newly diagnosed AML. It’s also approved for children ages 2 years and older with relapsed or refractory AML.
Mylotarg may be used alone or with other drugs.
- For acute myeloid leukemia (AML) that’s newly diagnosed, Mylotarg can be used with chemotherapy drugs:
- In adults, daunorubicin and cytarabine are the chemotherapy drugs used with Mylotarg. Adults who can’t use chemotherapy, or choose not to, may use Mylotarg on its own.
- In children, daunorubicin and cytarabine or other chemotherapy drugs may be used with Mylotarg.
- For AML that’s relapsed* or refractory,* Mylotarg is used alone.
Before you receive each Mylotarg infusion, you’ll be given certain drugs (called premedications) to help lower your risk for an infusion reaction.
Infusion reactions are side effects that occur during or shortly after you receive a drug by intravenous (IV) infusion. With an IV infusion, the drug is slowly injected into a vein over a period of time. To learn more about infusion reactions, see the “Mylotarg side effects” section below. Your Mylotarg premedications will likely include:
- acetaminophen (Tylenol) taken by mouth about 1 hour before your Mylotarg infusion
- diphenhydramine (an antihistamine) taken by mouth or injection about 1 hour before the infusion
- a corticosteroid such as methylprednisolone taken by mouth or injection about 30 minutes before the infusion
You may also receive other drugs to help reduce your risk of certain side effects with Mylotarg. For example, you may be given medication to help prevent nausea.
If you have questions about other drugs you may be given with Mylotarg, talk with your doctor.
* Relapsed cancer has returned after remission, which is a decrease in cancer symptoms. Refractory cancer hasn’t responded to previous cancer treatments.
Mylotarg can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Mylotarg. These lists do not include all possible side effects.
For more information about the possible side effects of Mylotarg, talk with your doctor or pharmacist. They can give you tips on how to deal with any side effects that may be concerning or bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs it has approved. If you would like to notify the FDA about a side effect you’ve had with Mylotarg, you can do so through MedWatch.
Mild side effects
Mild side effects* of Mylotarg can include:
- nausea and vomiting
- constipation
- headache
- rash
- decreased appetite
- mucositis (inflammation and soreness in your mouth and digestive tract)
- fever
- increased liver enzymes
Most of these side effects may go away within a few days or a couple of weeks. But if they become more severe or don’t go away, talk with your doctor or pharmacist.
* This is a partial list of mild side effects from Mylotarg. To learn about other mild side effects, talk with your doctor or pharmacist, or view Mylotarg’s prescribing information.
Serious side effects
Serious side effects from Mylotarg aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 or your local emergency number if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include:
- Febrile neutropenia (fever with a low white blood cell count). Symptoms can include:
- single temperature reading of 101°F (38.3°C) or higher
- temperature of 100.4°F (38°C) or higher that lasts for more than 1 hour
- Infection. Symptoms can include:
- fever
- shivering
- cough
- sore throat
- diarrhea
- urinating more often than usual
- Prolonged QT interval (an abnormal heart rhythm). Symptoms can include:
- fluttering feeling in your chest
- dizziness
- fainting
- Bleeding.*
- Infusion reactions.*
- Allergic reaction.*
- Liver problems, including a condition called veno-occlusive liver disease (VOD).*†
* For more information about this side effect, see “Side effect details” below.
† Mylotarg has a
Side effect details
Here’s some detail on certain side effects this drug may cause.
Liver problems
Mylotarg has a
Serious liver problems Mylotarg can cause include a condition called veno-occlusive liver disease (VOD). This condition is also known as sinusoidal obstruction syndrome.
VOD occurs when small blood vessels in your liver become blocked. This condition can be severe and even fatal. It has been reported when Mylotarg is used alone or when it’s used with other chemotherapy.
VOD was a common side effect in clinical studies of Mylotarg. To find out how often this side effect occurred in clinical studies, see the drug’s prescribing information.
People with certain health factors may have a higher risk for VOD. See the “Mylotarg precautions” section to learn more.
VOD symptoms
During your Mylotarg treatment, your doctor will monitor you closely for symptoms of VOD. These may include:
- swelling of your liver
- ascites (swelling of your belly due to fluid buildup)
- pain in the upper-right side of your belly
- rapid weight gain
- increased levels of bilirubin or liver enzymes in certain blood tests
Tell your doctor right away if you have any of these symptoms. If you have liver problems during your Mylotarg treatment, your doctor may need to delay your next dose until your liver recovers. In some cases, you may need to stop using Mylotarg permanently.
If you have concerns about liver problems with Mylotarg, talk with your doctor or pharmacist.
Bleeding
Acute myeloid leukemia (the condition Mylotarg is used to treat) often causes thrombocytopenia (low platelet count). Mylotarg can also cause low platelet counts.
Platelets are blood cells that help your blood to clot. If you have a low platelet count, you may bruise or bleed more easily than usual. Some people using Mylotarg have had severe or even life-threatening bleeding, such as bleeding in the brain.
Bleeding is one of the most common side effects reported with Mylotarg. To find out how often this side effect occurred in clinical studies, see the drug’s prescribing information.
Chemotherapy can also cause low platelet counts. You may have a higher risk for bleeding if you use Mylotarg with other chemotherapy. (Mylotarg is a type of chemotherapy, too.)
During treatment with Mylotarg, tell your doctor right away if you have symptoms of bleeding. These may include:
- bruising for no obvious reason
- bleeding, such as nosebleeds or bleeding gums, for no obvious reason
- bleeding that takes a long time to stop, such as if you injure yourself
- coughing up blood
- blood in your urine, which may be pink or red
- blood in your stool, which may be red, black, or tarry
If you have severe bleeding with Mylotarg, your doctor may delay your next dose until your platelet levels recover. In some cases, you may have to stop your Mylotarg treatment permanently.
If you have concerns about bleeding with Mylotarg, talk with your doctor or pharmacist.
Infusion reactions
Some people may have infusion reactions with Mylotarg. Infusion reactions occur during or shortly after you receive a drug by intravenous (IV) infusion. (With an IV infusion, the drug is slowly injected into a vein over a period of time.)
Infusion reactions may occur during a Mylotarg infusion or within 24 hours after the infusion. They may cause symptoms such as:
- shivering
- fever
- shortness of breath
- dizziness
- feeling lightheaded
- hypotension (low blood pressure)
- fast heartbeat
It’s not known how often infusion reactions may have occurred in clinical studies of Mylotarg.
To help prevent infusion reactions, you’ll be given certain drugs (called premedications) before each Mylotarg infusion. You’ll likely be given acetaminophen (Tylenol), a corticosteroid, and an antihistamine.
Your doctor will monitor your heart rate, blood pressure, and breathing during the Mylotarg infusion. You’ll also be monitored for at least 1 hour after the infusion has finished. If you notice any symptoms of an infusion reaction, tell your doctor right away. If you have a reaction during the infusion, the infusion will be stopped until your symptoms improve. If you have a serious reaction, the treatment may need to be stopped permanently.
For more information about infusion reactions that can occur with Mylotarg, talk with your doctor or pharmacist.
Allergic reactionAs with most drugs, some people can have an allergic reaction after taking Mylotarg. Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (warmth or redness/deepening of skin color for a brief time)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
Call your doctor right away if you have an allergic reaction to Mylotarg, as the reaction could become severe. Call 911 or your local emergency number if your symptoms feel life threatening or if you think you’re having a medical emergency.
Here are answers to some frequently asked questions about Mylotarg.
What’s the success rate of treating AML with Mylotarg?
Mylotarg has been shown to be an effective treatment for acute myeloid leukemia (AML). However, exact success rates with the drug depend on the form of AML being treated and if it’s used alone or with chemotherapy. For information on success rates with Mylotarg in clinical studies, see the prescribing information for Mylotarg.
How effective Mylotarg is for you may depend on various factors. These include:
- the type of AML you have and how advanced it is
- your age
- other treatments you may be using
- how your body responds to the drug
To find out what you can expect with Mylotarg treatment, talk with your doctor.
Is Mylotarg a chemotherapy drug?
Yes, Mylotarg is a type of chemotherapy. But unlike traditional chemotherapy, Mylotarg is a targeted form of chemotherapy.
Traditional chemotherapy kills all cells that are rapidly growing and multiplying in your body. It often kills healthy cells as well as cancer cells. Mylotarg, on the other hand, targets and kills cancer cells only.
Mylotarg contains a chemotherapy drug that’s attached to a monoclonal antibody. Monoclonal antibodies are drugs made from immune system cells. These drugs attach to specific proteins on cells. The monoclonal antibody in Mylotarg attaches to a specific protein that’s found on cancerous cells. It delivers the chemotherapy directly into these cells.
Although it’s more targeted than traditional chemotherapy, Mylotarg can still cause side effects. To learn more, see the “Mylotarg side effects” section above.
Why was Mylotarg withdrawn from the market and then later reapproved?
Mylotarg was first approved by the Food and Drug Administration (FDA) in 2000. It received
Accelerated approval is granted to certain drugs used for conditions without many successful treatment options. The approval is based on information from early clinical studies of the drug. Depending on the results of further clinical studies, the drug may then be fully approved by the FDA, or the approval may be revoked.
With Mylotarg, further clinical studies found the drug didn’t improve survival rates in people ages 60 years and older with relapsed AML when the higher original dosage was used. The studies also found that this group of people had an increased risk of serious side effects from Mylotarg use. As a result, the manufacturer withdrew Mylotarg from the market in 2010.
However, Mylotarg was then studied in different groups of people with AML. This time it was also used in younger people with AML that was newly diagnosed, relapsed, or refractory.† It was used at a lower dose and with a different dosing schedule. The new studies found that when Mylotarg was used in these ways, its benefits outweighed its risks.
As a result of these studies, Mylotarg was reapproved by the FDA in 2017. This time it was granted full approval to treat relapsed or refractory AML in adults and children ages 2 years and older. It also received full approval to treat newly diagnosed AML in adults. In 2020, the FDA approved Mylotarg for newly diagnosed AML in children ages 1 month and older.
* Relapsed cancer has returned after remission, which is a decrease in cancer symptoms.
† Refractory cancer hasn’t responded to previous cancer treatments.
As with all medications, the cost of Mylotarg can vary.
The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
Before approving coverage for Mylotarg, your insurance company may require you to get prior authorization. This means that your doctor and insurance company will need to communicate about your prescription before the insurance company will cover the drug. The insurance company will review the prior authorization request and decide if the drug will be covered.
If you’re not sure if you’ll need to get prior authorization for Mylotarg, contact your insurance company.
Financial and insurance assistance
If you need financial support to pay for Mylotarg, or if you need help understanding your insurance coverage, help may be available.
Pfizer Inc., the manufacturer of Mylotarg, offers a program called Pfizer Oncology together. For more information and to find out if you’re eligible for support, call 877-744-5675 or visit the program website.
Generic or biosimilar version
Mylotarg is a biologic drug that’s available only as a brand-name medication. It’s not currently available in a biosimilar form.
A biologic drug is made from living cells, while other drugs are made from chemicals. Drugs made from chemicals can have generics, which are exact copies of the active drug in the brand-name medication. Biologics, on the other hand, can’t be copied exactly. Therefore, instead of a generic, biologics have biosimilars. Biosimilars are “similar” to the parent drug, and they’re considered to be just as effective and safe.
Like generics, biosimilars usually cost less than brand-name drugs.
The Mylotarg dosage your doctor prescribes will depend on several factors. These include:
- the form of AML you’re using Mylotarg to treat
- your age
- your body surface area, measured in square meters (m2)
- other treatments you may use with Mylotarg
- if you have certain side effects
The following information describes dosages that are commonly used or recommended. However, your doctor will determine the best dosage to fit your needs.
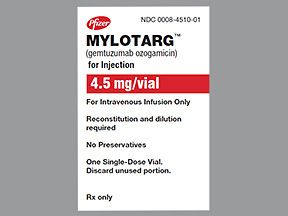
Drug forms and strengths
Mylotarg is given by intravenous (IV) infusion. An IV infusion is an injection into a vein that’s given over a period of time. You’ll receive Mylotarg infusions at your doctor’s office, a hospital, or an infusion center.
Mylotarg comes as a powder in a single-dose vial. Each vial contains 4.5 milligrams (mg) of Mylotarg. Your doctor will mix the powder with sterile water to make a liquid solution.
Dosage for AML
The recommended dosage of Mylotarg for acute myeloid leukemia (AML) in adults depends on the form of AML it’s being used to treat. It also depends on whether you use Mylotarg alone or with chemotherapy. Typical dosages are described below.
- For newly diagnosed AML in adults, when used with chemotherapy: The recommended dose of Mylotarg is 3 mg per m2 of body surface area, up to a maximum of 4.5 mg per dose. This is typically given on days 1, 4, and 7 of your first week of treatment. You’ll also likely have chemotherapy every day this week. This first week of treatment is called the induction cycle. After this, you may have two more rounds of treatment. These are called consolidation cycles. For each consolidation cycle, you’ll likely receive Mylotarg infusions on day 1 and chemotherapy on days 1 to 4.
- For newly diagnosed AML in adults, when used alone: The recommended dose of Mylotarg is 6 mg per m2 of body surface area on day 1 of treatment. This is followed by 3 mg per m2 of body surface area on day 8 of treatment. The first round of treatment is called the induction cycle. After this, you may have up to eight more rounds of treatment. These are called continuation cycles. The recommended dose for each continuation cycle is 2 mg per m2 of body surface area, and these doses are usually given once every 4 weeks.
- For AML that’s relapsed* or refractory* in adults: For this purpose, Mylotarg is used alone. The recommended dose is 3 mg per m2 of body surface area, up to a maximum of 4.5 mg per dose. This is typically given as one round of treatment on days 1, 4, and 7.
* Relapsed cancer has returned after remission, which is a decrease in cancer symptoms. Refractory cancer hasn’t responded to previous cancer treatments.
Children’s dosage
Mylotarg is used for newly diagnosed AML in children ages 1 month and older. It’s also used for relapsed* or refractory* AML in children ages 2 years and older. The typical recommended dosages are described below.
- For newly diagnosed AML in children: For this purpose, Mylotarg is used with chemotherapy. The child will likely have five rounds of chemotherapy. Mylotarg is typically given on day 6 of the first round and on day 7 of the fourth round. For children with a body surface area of at least 0.6 m2, the recommended Mylotarg dose is 3 mg per m2 of body surface area. For children with a body surface area less than 0.6 m2, the recommended Mylotarg dose is 0.1 mg per kilogram of body weight.
- For relapsed or refractory AML in children: Mylotarg is used on its own for this purpose. The recommended dose is 3 mg per m2 of body surface area, up to a maximum of 4.5 mg per dose. This dose is typically given as one round of treatment on days 1, 4, and 7.
* Relapsed cancer has returned after remission, which is a decrease in cancer symptoms. Refractory cancer hasn’t responded to previous cancer treatments.
What if I miss a dose?
It’s important to keep your appointments for your Mylotarg infusions. If you miss an appointment, call your doctor’s office right away to reschedule.
To help make sure you don’t miss an appointment, try setting a reminder on your phone.
Will I need to use this drug long term?
No. Mylotarg is a short-term treatment for AML. The number of doses you’ll receive depends on the treatment plan your doctor has prescribed for you. Factors that can affect your treatment length include the type of AML you have, how it responds to treatment, and if you experience certain side effects.
If you have questions about how long you’ll use Mylotarg, talk with your doctor.
Mylotarg is used to treat acute myeloid leukemia (AML) that’s CD33-positive. To learn more about its specific uses, see the “Mylotarg for AML” section above.
What happens with AML?
AML is a type of cancer that affects myeloid cells, which are cells in your bone marrow. (Bone marrow is the spongy material inside your bones, where your blood cells are made.)
Myeloid cells normally develop into red blood cells, white blood cells, and platelets. These move from your bone marrow into your bloodstream when needed. But with AML, the myeloid cells develop an abnormality that stops them from growing into normal, mature blood cells.
Instead, they develop into immature cells called blasts. The blasts don’t function as normal blood cells. And they take up lots of space in your bone marrow, leaving less space for healthy blood cells to develop. This leads to low levels of white blood cells, red blood cells, and platelets.
Mylotarg is used to treat a specific type of AML called CD33-positive AML. With this kind of AML, the cancer cells have high levels of a particular protein called CD33 on their surface. Most cases of AML are CD33-positive.
What Mylotarg does
Mylotarg is a targeted therapy for CD33-positive AML. Targeted therapies are treatments with a mechanism of action that allows them to act very precisely on cancer cells. (Mechanism of action is the way a drug works.)
Mylotarg contains a monoclonal antibody attached to a chemotherapy drug. Monoclonal antibodies are drugs made from immune system cells. These drugs attach to specific proteins on cells. The monoclonal antibody in Mylotarg attaches to the CD33 protein on the cancerous myeloid and blast cells.
After the monoclonal antibody attaches to the CD33 protein, Mylotarg gets absorbed into the cancer cells. It then releases the chemotherapy drug, which kills the cancer cells. Healthy, mature blood cells don’t have the CD33 protein on their surface, so they’re not affected by Mylotarg.
Mylotarg helps lower the number of cancerous myeloid cells and blast cells in your bone marrow. This allows space for healthy myeloid cells to develop into healthy, mature blood cells. This helps your blood counts return to normal.
How long does it take to work?
Mylotarg typically starts to work soon after you receive your first dose. However, because of how the drug works, you likely won’t notice its affects. Instead, you’ll have various tests done during your treatment to check whether Mylotarg is working for you.
Mylotarg isn’t known to interact with alcohol. However, if you have certain side effects with Mylotarg, such as nausea, headache, or diarrhea, drinking alcohol could make these worse. (See the “Mylotarg side effects” section above.)
In addition, Mylotarg can sometimes cause serious liver problems, including a condition called veno-occlusive liver disease (VOD)*. Drinking alcohol may make these liver problems worse.
If you drink alcohol, talk with your doctor about how much may be safe for you to drink during your Mylotarg treatment.
* Mylotarg has a
Mylotarg may interact with several other medications.
Different interactions can cause different effects. For instance, some interactions can interfere with how well a drug works. Other interactions can increase side effects or make them more severe.
Mylotarg and other medications
Below is a list of medications that can interact with Mylotarg. This list does not contain all drugs that may interact with Mylotarg.
Before taking Mylotarg, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
Types of drugs that may interact with Mylotarg include:
- Drugs that can cause prolonged QT interval (a type of abnormal heart rhythm). Mylotarg can also cause prolonged QT interval. Therefore, using it with other drugs that could cause this side effect may raise your risk even more. Examples of these drugs include:
- certain drugs for irregular heartbeat, such as amiodarone (Pacerone)
- certain antidepressants, such as citalopram (Celexa)
- certain antipsychotics, such as pimozide (Orap)
- certain antimicrobials, such as clarithromycin
- Drugs that can change the levels of electrolytes (such as potassium or magnesium) in your blood. Using Mylotarg with these drugs may also raise your risk for prolonged QT interval. Examples of these drugs include:
- diuretics, such as furosemide (Lasix)
If you have questions about potential interactions with Mylotarg, talk with your doctor or pharmacist.
Mylotarg and herbs and supplements
There aren’t any herbs or supplements that have been specifically reported to interact with Mylotarg. However, you should still check with your doctor or pharmacist before using any of these products while taking Mylotarg.
Mylotarg and foods
There aren’t any foods that have been specifically reported to interact with Mylotarg. If you have any questions about eating certain foods with Mylotarg, talk with your doctor.
Mylotarg is given by intravenous (IV) infusion. An IV infusion is an injection into a vein that’s given over a period of time. Mylotarg infusions typically last about 2 hours.
You’ll receive Mylotarg infusions at your doctor’s office, a hospital, or an infusion center.
When it’s given
The treatment schedule for Mylotarg depends on the form of AML it’s being used to treat. It also depends if you use Mylotarg alone or with other chemotherapy.
- For newly diagnosed AML in adults, when used with chemotherapy: You’ll likely receive Mylotarg infusions on days 1, 4, and 7 of your first week of treatment. You’ll also likely have chemotherapy every day this week. This first week of treatment is called the induction cycle. After this, you may have two more rounds of treatment, which are called consolidation cycles. For each consolidation cycle, you’ll likely receive Mylotarg infusions on day 1 and chemotherapy on days 1 to 4.
- For newly diagnosed AML in adults, when used alone: Mylotarg is typically given on day 1 and day 8 of treatment. This first round of treatment is called the induction cycle. After this, you may have up to eight more rounds of treatment. These are called continuation cycles, and these doses are usually given once every 4 weeks.
- For newly diagnosed AML in children: For this purpose, Mylotarg is used with chemotherapy. The child will likely have five rounds of chemotherapy. Mylotarg is typically given on day 6 of the first round and on day 7 of the fourth round.
- For AML that’s relapsed* or refractory* in adults and children: Mylotarg is used on its own for this purpose. It’s typically given as one round of treatment on days 1, 4, and 7.
To help make sure you don’t miss an appointment for your Mylotarg infusions, try setting a reminder on your phone.
* Relapsed cancer has returned after remission, which is a decrease in cancer symptoms. Refractory cancer hasn’t responded to previous cancer treatments.
Mylotarg isn’t safe to take during pregnancy. No human studies have looked at Mylotarg use during pregnancy. However, the drug is expected to cause harm to a fetus if used during pregnancy. This is based on the way Mylotarg works, along with effects seen in animal studies. Mylotarg was found to cause birth defects when given to pregnant females in animal studies.
If you could become pregnant, you’ll need to have a pregnancy test before using Mylotarg to make sure you’re not pregnant. You should use birth control to prevent pregnancy during your Mylotarg treatment and for 6 months after your last dose. For more details, see the “Mylotarg and birth control” section below.
If you’re pregnant or planning to become pregnant, talk with your doctor. They’ll likely recommend a treatment other than Mylotarg.
Mylotarg and fertility
Mylotarg may affect your fertility (the ability to conceive a child). In animal studies, Mylotarg was found to reduce fertility in both males and females.
If you’re concerned about Mylotarg affecting your fertility, talk with your doctor before starting treatment.
Even though Mylotarg may reduce fertility, you should still use birth control to prevent pregnancy during treatment and for a few months after. To learn more, see the “Mylotarg and birth control” section below.
Mylotarg isn’t safe to use during pregnancy. If you’re sexually active and you or your partner can become pregnant, talk with your doctor about your birth control needs while you’re using Mylotarg.
For more information about Mylotarg use during pregnancy, see the “Mylotarg and pregnancy” section above.
For females* using Mylotarg
If you’re able to become pregnant, you should use birth control during your Mylotarg treatment and for 6 months after your last dose.
For males* using Mylotarg
If your partner could become pregnant, you should use birth control (such as condoms) during your Mylotarg treatment and for 3 months after your last dose.
* In this article, we use the terms “male” and “female” to refer to someone’s sex assigned at birth. For information about the difference between sex and gender, see this article.
You shouldn’t breastfeed during your Mylotarg treatment and for at least 1 month after your last dose. It’s not known if Mylotarg passes into breast milk or if it can affect breast milk production. However, if used during breastfeeding, Mylotarg could have serious side effects in a breastfed child.
If you’re currently breastfeeding or planning to breastfeed, talk with your doctor about your options.
This drug comes with several precautions.
FDA warning: Liver problems
This drug has a
Mylotarg can sometimes cause serious liver problems, including a condition called veno-occlusive liver disease (VOD).
VOD has been reported in people using Mylotarg when the drug is used alone or when it’s used with chemotherapy. To learn more, see “Liver problems” under the “Mylotarg side effects” section above.
Other precautions
Before taking Mylotarg, talk with your doctor about your health history. Mylotarg may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Stem cell transplant. Mylotarg can sometimes cause a serious liver problem called veno-occlusive liver disease (VOD). See the FDA warning above to learn more. If you have a hematopoietic stem cell transplant before or after your Mylotarg treatment, you may have a higher risk for VOD. If you’ve had a stem cell transplant or plan to have one, talk with your doctor about whether Mylotarg is right for you.
- Low blood cell counts. Acute myeloid leukemia (the condition Mylotarg is used to treat) can cause low levels of white blood cells, red blood cells, and platelets. Mylotarg can also cause low blood cell counts, so it can make these problems worse. Your blood cell counts will be checked before and after each dose of Mylotarg. If your blood counts are too low after receiving Mylotarg, your doctor may delay your next infusion or stop your treatment permanently.
- Prolonged QT interval. Mylotarg can sometimes cause an abnormal heart rhythm called a prolonged QT interval. If you have a personal or family history of prolonged QT interval (sometimes called long QT syndrome), you may have a higher risk for this side effect. You’ll likely have an electrocardiogram (ECG) before starting Mylotarg to make sure the treatment is safe for you. Having abnormal levels of electrolytes (such as potassium or magnesium) in your blood also raises your risk for a prolonged QT interval with Mylotarg. Your doctor will order frequent blood tests during your treatment to check your electrolytes.
- Allergic reaction. If you’ve had an allergic reaction to Mylotarg or any of its ingredients, you shouldn’t take Mylotarg. Ask your doctor what other medications are better options for you.
- Pregnancy. Mylotarg isn’t safe to take during pregnancy. For more information, see the “Mylotarg and pregnancy” section above.
- Breastfeeding. You shouldn’t breastfeed while taking Mylotarg. For more information, see the “Mylotarg and breastfeeding” section above.
Note: For more information about the potential negative effects of Mylotarg, see the “Mylotarg side effects” section above.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.