Suboxone (buprenorphine and naloxone) is a brand-name prescription medication. The Food and Drug Administration (FDA) has approved it to treat dependence on opioid drugs. This includes treating opioid use disorder (formerly called opioid addiction). The medication can help reduce withdrawal symptoms when you stop using an opioid and for a long time after.
Suboxone comes as a film that dissolves in your mouth, either under your tongue or inside your cheek.
Suboxone contains the active ingredients buprenorphine and naloxone. Buprenorphine belongs to a class of drugs called partial opioid agonists. Naloxone belongs to a class of drugs called opioid antagonists.
Suboxone is also available as the generic drug buprenorphine and naloxone. This generic form comes as an oral tablet.
For information about the dosage of Suboxone, including its strengths and how to take it, keep reading. For a comprehensive look at Suboxone, see this article.
This article describes typical dosages for Suboxone provided by the drug’s manufacturer. When taking Suboxone, always follow the dosage prescribed by your doctor.
Typical Suboxone dosages are described below. These are dosages recommended and approved by the manufacturer and the Food and Drug Administration (FDA). However, your doctor will prescribe the Suboxone dosage that’s right for you.
Suboxone form
Suboxone comes as a film that dissolves in your mouth, either under your tongue or inside your cheek.
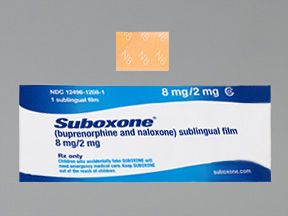
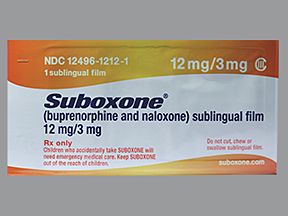
Suboxone strengths
Suboxone comes in four strengths:
- 2 milligrams (mg) buprenorphine/0.5 mg naloxone
- 4 mg buprenorphine/1 mg naloxone
- 8 mg buprenorphine/2 mg naloxone
- 12 mg buprenorphine/3 mg naloxone
Typical dosages
Typically, your doctor will start your treatment with a low dosage. Then, they’ll adjust it over time to reach the amount that’s right for you. Your doctor will ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to fit your needs.
Treating opioid use disorder with Suboxone consists of two stages: induction and maintenance. Below are more details on induction and maintenance and possible Suboxone dosages during each stage.
Induction dosage
The induction phase refers to when you first stop taking opioids or your opioid use decreases. Doctors prescribe Suboxone during induction to help reduce withdrawal symptoms. Withdrawal symptoms are side effects that occur after you stop taking a drug your body has become dependent on.
Suboxone is only prescribed for induction if you are dependent on a short-acting opioid. Short-acting opioids include morphine, heroin, and oxycodone. Your doctor will wait to prescribe your first Suboxone dose for induction until it’s been at least 6 hours since your last opioid dose.
During induction treatment, you’ll receive Suboxone doses at your doctor’s office or clinic. For induction therapy, it’s recommended that you place Suboxone film under your tongue and not on your cheeks.
The table below describes recommended Suboxone induction dosages:
| Suboxone treatment day | Suboxone dose* and notes |
| Day 1 | A starting dose ranging from 2 mg/0.5 mg up to 8 mg/2 mg. • Your doctor will give this dose in their office or clinic. • Your doctor may give your starting dose as one or multiple doses, depending on your withdrawal symptoms in the office or clinic. |
| Day 2 | A single dose of up to 16 mg/4 mg. • Your doctor will determine your dose based on your withdrawal symptoms. This may be the same dose as Day 1, or they may adjust the dose based on your symptoms. • Your doctor will give your dose in their office or clinic and evaluate your withdrawal symptoms. |
| Day 3 and beyond, as needed | Your doctor will continue to give Suboxone doses in their office or clinic. They’ll evaluate you and continue the induction stage until your withdrawal symptoms are managed for at least 2 hours. Your dose on Day 3 and beyond will be based on the doses that best managed your symptoms on Days 1 and 2. Once your Suboxone dose and withdrawal symptoms are managed, you’ll start maintenance treatment. See below for more information on maintenance treatment. |
* Each dose contains two numbers because Suboxone contains two drugs: buprenorphine and naloxone. The first number represents the buprenorphine dose per film. The second number is the dose of naloxone in each film.
Maintenance dosage
Once you and your doctor find a Suboxone dosage that manages your symptoms, your treatment will continue into the maintenance phase. For the maintenance phase of treatment, Suboxone film may be placed under your tongue or inside your cheeks to dissolve.
The typical maintenance dosage of Suboxone ranges from 4 mg buprenorphine/1 mg naloxone up to 24 mg buprenorphine/6 mg naloxone, which is also the maximum dose.
During the maintenance phase, you’ll likely have weekly or monthly appointments with your doctor. How long your maintenance treatment lasts depends on your treatment needs and goals. This stage may last a few weeks or months, or it could last for years. During this time, you may continue going to your doctor’s office or clinic to receive Suboxone doses. You may also be able to give yourself doses at home. This will depend on your specific situation and the treatment plan you and your doctor agreed on.
Long-term treatment
Suboxone may be a short- or long-term treatment. If you and your doctor determine that Suboxone is safe and effective for you, you’ll take it for as long as you benefit from treatment.
You and your doctor will periodically reevaluate your need for Suboxone throughout your treatment. Your doctor can answer any questions you may have about how long you’ll take Suboxone.
Below are some answers to frequently asked questions about Suboxone dosages.
What are the signs my Suboxone dosage is too high or too low?
Signs that your Suboxone dosage is too low can include cravings for opioids. It can also include symptoms of opioid withdrawal. These symptoms can include dilated pupils, diarrhea, and excessive sweating.
On the other hand, your Suboxone dose may be too high if you experience side effects from the medication. Examples of side effects Suboxone may cause include headache, fatigue, and difficulty sleeping. (Symptoms of an overdose can also be a sign your Suboxone dose is too high. These symptoms are detailed in the “Suboxone and overdose” section below.)
Check out this article to learn more about Suboxone, including possible side effects the drug can cause. Contact your doctor if you’re having side effects from Suboxone. This may mean your dosage is too high.
Your doctor will instruct you on what to watch for during your Suboxone treatment. If you have questions about how to know whether your dose is too low or too high, talk with your doctor.
Is there a recommended dosage chart for Suboxone?
No, there’s no official dosage chart for Suboxone.
Doctors and other healthcare professionals sometimes use a dosage guide or chart for certain drugs. These charts or guides can help healthcare professionals quickly calculate a dose when needed.
Your Suboxone dosage will be based on several factors, including the stage and severity of your opioid dependence. Your doctor can provide more details on how they’ll determine your Suboxone dosage.
Can Suboxone be used for pain? If so, what is the drug’s dose for pain?
No, Suboxone is not approved as a treatment for pain. Using the drug for this purpose is an example of off-label use. With off-label use, a drug is prescribed for a purpose other than what it’s approved for.
Talk with your doctor if you’re interested in learning more about off-label uses for Suboxone.
What is the recommended maximum daily dose of Suboxone?
The highest recommended dose of Suboxone in one day is 24 milligrams (mg) buprenorphine/6 mg naloxone.
For more information on Suboxone doses, refer to the “Dosages of Suboxone” section above. This includes information about recommended dosages, including the lowest dose and highest dose typically prescribed. You can also talk with your doctor or pharmacist. Or, you can view the drug’s full prescribing information.
The Suboxone dosage your doctor prescribes will depend on several factors. These include:
- the severity of your opioid dependence
- the stage of treatment you’re in for opioid dependence
Other medical conditions you have can also affect your Suboxone dosage.
Suboxone comes as a film that dissolves in your mouth, either under your tongue or inside your cheeks. Remember to always take Suboxone according to your doctor’s instructions.
When you first begin treatment with Suboxone, you’ll receive your doses in your doctor’s office or clinic. As your treatment progresses, you may be able to take your doses at home.
Use the entire Suboxone film for each dose. Do not cut, tear, chew, or swallow Suboxone films.
You should not eat or drink while the Suboxone film is in your mouth. However, you may take a dose on an empty or full stomach, as Suboxone films are absorbed in your mouth and not your stomach. Once the Suboxone film fully dissolves, rinse your mouth with water and swallow it. You should wait at least 1 hour after the film dissolves before brushing your teeth.
To view step-by-step instructions for using Suboxone, refer to the drug’s medication guide. You can also talk with your doctor or pharmacist for help.
ACCESSIBLE DRUG LABELS AND CONTAINERSIf you’re having trouble reading your prescription label, talk with your doctor or pharmacist. Some pharmacies offer labels with large print, braille, or a code you scan with a smartphone to convert text to speech. If your local pharmacy doesn’t have these options, your doctor or pharmacist might be able to recommend a pharmacy that does.
If you’re having trouble opening medication bottles, ask your pharmacist about putting Suboxone in an easy-open container. They also may recommend tools that can make it easier to open bottles.
If you miss a Suboxone dose, try to take it as soon as you remember.
However, you should skip the missed dose if it’s nearly time for your next dose. In this case, take the next dose as scheduled. Do not use more than one dose of Suboxone at once, unless specifically instructed to do so by your doctor.
To help make sure you don’t miss a dose, try using a medication reminder. This can include setting an alarm or using a timer. You could also download a reminder app on your phone.
If you miss a dose of Suboxone and aren’t sure what to do, call your doctor. They can instruct you on the best course of action to take.
If you take more Suboxone than your doctor prescribes, you may develop serious side effects.
It’s important that you do not take more Suboxone than your doctor advises.
Symptoms of an overdose
Overdose symptoms of Suboxone can include:
- pinpoint pupils
- low blood pressure
- slowed or difficult breathing
- extreme sleepiness
- loss of consciousness
- death, in extreme cases
If you take more than the recommended amount of Suboxone
Call your doctor right away if you believe you’ve taken too much Suboxone. Another option is to call America’s Poison Centers at 800-222-1222 or use its online tool. If you have severe symptoms, immediately call 911 or your local emergency number, or go to the nearest emergency room.
Treatment with Suboxone can cause dependence. With dependence, your body becomes used to a drug and needs it in your system in order to function as usual. This means you may have withdrawal symptoms if you suddenly stop taking Suboxone after taking it regularly for some time. (Withdrawal symptoms are side effects that happen after you stop taking a drug your body has become dependent on.)
Dependence happens with Suboxone because it contains the opioid drug buprenorphine. This drug is weaker than many other opioid drugs. So, dependence and withdrawal symptoms with Suboxone are often milder compared with symptoms caused by other opioids. This also means that withdrawal symptoms with Suboxone may not appear right away.
Symptoms of withdrawal after abruptly stopping Suboxone include:
- feeling anxious or agitated
- sleep problems
- muscle aches
- nausea, vomiting, and diarrhea
- excessive sweating
These symptoms can be very uncomfortable. However, they’re usually not life threatening.
You and your doctor will periodically reevaluate your need for Suboxone throughout your treatment. If a decision is made to stop your Suboxone treatment, your doctor will slowly lower your dose over time. This is known as a dose taper. A dose taper helps reduce your risk of withdrawal symptoms when you stop treatment with Suboxone.
Tapering your Suboxone dose could last several weeks or even months. The exact time needed to taper your dose depends on your Suboxone dose and how long you’ve taken it.
Do not stop taking Suboxone unless your doctor specifically tells you to do so. If you have questions about your treatment, talk with your doctor.
The dosages in this article are typical dosages provided by the drug’s manufacturer. If your doctor recommends Suboxone for you, they will prescribe the dosage that’s right for you. Always follow the dosage that your doctor prescribes.
As with any drug, never change your dosage of Suboxone without your doctor’s recommendation. If you have questions about the dosage of Suboxone that’s best for you, talk with your doctor.
Besides learning about dosage, you may want other information about Suboxone. These additional articles might be helpful:
- More about Suboxone. For information about other aspects of Suboxone, refer to this article.
- Drug comparison. To find out how Suboxone compares with Sublocade, read this article.
- Interactions. For details about what Suboxone interacts with, see this article.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.