Tysabri (natalizumab) is a brand-name drug prescribed for multiple sclerosis (MS), clinically isolated syndrome (CIS), and Crohn’s disease in adults. Tysabri comes as an intravenous (IV) infusion given by a healthcare professional, typically every 4 weeks.
Tysabri is a biologic and belongs to a drug class called integrin receptor antagonists. Tysabri is not available in a
Keep reading for specific information about the dosage of Tysabri, including its strength and how it’s given. For a comprehensive look at Tysabri, see this article.
Note: This article describes the Tysabri dosage for MS, CIS, and Crohn’s disease provided by the drug’s manufacturer. However, your doctor will prescribe the dosage that’s right for you.
Here’s some information on the dosage and administration of Tysabri for multiple sclerosis (MS), clinically isolated syndrome (CIS), and Crohn’s disease.
Tysabri form
Tysabri comes as a solution that’s given as an intravenous (IV) infusion by a healthcare professional.
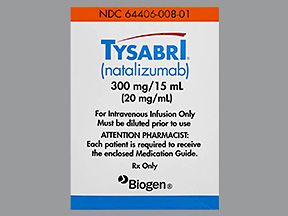
Tysabri strength
Tysabri comes in one strength: 300 milligrams (mg) per 15 milliliters (mL) of solution.
Tysabri dosage for all uses
The following information describes the infusion dosage that’s commonly prescribed or recommended. However, your doctor will determine the best dosage to fit your needs.
For MS, CIS, and Crohn’s disease, the typical Tysabri dosing frequency is 300 mg once every 4 weeks. The usual dosage of Tysabri is the same for all conditions it’s prescribed to treat.
Long-term treatment
Tysabri is meant to be a long-term treatment. If you and your doctor determine that Tysabri is safe and effective for you, you’ll likely receive it long term.
If you’re receiving Tysabri for Crohn’s disease, your doctor will likely have you stop Tysabri treatment if the drug hasn’t been effective after 12 weeks.
Note that long-term treatment raises your risk of a serious side effect called progressive multifocal leukoencephalopathy (PML). Tysabri has a
Extended dosing
In some cases, your doctor might recommend extended dosing of Tysabri. This means receiving the drug once every 6–8 weeks (instead of every 4 weeks). This is considered off-label dosing. This means it’s not FDA-approved, but doctors can choose to prescribe the drug in this way.
Extended dosing may help lower your risk of PML. But more studies are needed to confirm whether extended dosing could lower the risk of PML and still be effective.
It’s important to discuss the possible risks of extended dosing with your doctor. They can help you decide whether receiving Tysabri long term is right for you.
Tysabri is given as an intravenous (IV) infusion by a healthcare professional. (An IV infusion is an injection given into a vein over time.) You’ll likely receive Tysabri infusions at your doctor’s office, a clinic, a hospital, or an infusion center once every 4 weeks.
Tysabri infusions typically last about 1 hour. Then a healthcare professional will also monitor you for at least 1 hour after your infusion has finished. This is to make sure you don’t have an allergic reaction to Tysabri.
Note: Due to the risk of a serious brain infection called progressive multifocal leukoencephalopathy (PML),* Tysabri is only available through a drug safety program called the TOUCH Prescribing Program. You can only receive Tysabri from doctors and infusion centers that are enrolled in the program. If you have questions about this program, you can contact your doctor.
If you’d like to know more about infusions with Tysabri, talk with your doctor.
* Tysabri has a boxed warning about the risk of PML. For details, see the “Boxed warning” section at the top of this article.
If you miss an appointment to have your Tysabri infusion, call your doctor’s office right away to reschedule.
To help make sure that you don’t miss an appointment, put your dosing schedule on a calendar or try using a medication reminder. This can include setting an alarm or downloading a reminder app on your phone.
The dosages in this article are typical dosages provided by the drug’s manufacturer. If your doctor recommends Tysabri for you, they will prescribe the dosage that’s right for you. If you have questions about the dosage of Tysabri that’s right for you, talk with your doctor.
Besides learning about dosage, you may want other information about Tysabri. These additional articles might be helpful to you:
- More about Tysabri. For information about other aspects of Tysabri, refer to this article.
- Side effects. To learn about side effects of Tysabri, see this article. You can also look at the Tysabri prescribing information.
- Drug comparison. Find out how Tysabri compares with Ocrevus and Humira.
- Details about your condition. For details about how Tysabri is used for multiple sclerosis (MS), you can read this article. You can also refer to our MS hub for more information about this condition. To learn more about Crohn’s disease, see our inflammatory bowel disease hub and list of related articles.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.