Neulasta is a brand-name prescription medication. It’s FDA-approved for the following:
- Reducing the risk of infection due to a condition called febrile neutropenia in people with non-myeloid cancers. To use Neulasta, you must be taking an anticancer drug that could cause febrile neutropenia (low level of white blood cells called neutrophils).
- Treating radiation sickness. The type of radiation sickness that Neulasta is used for is called hematopoietic subsyndrome.
For detailed information on these conditions, see the “Neulasta uses” section below.
Neulasta drug class and forms
Neulasta contains one active drug ingredient: pegfilgrastim. Neulasta belongs to a drug class called leukocyte growth factors. A drug class is a group of medications that work in a similar way.
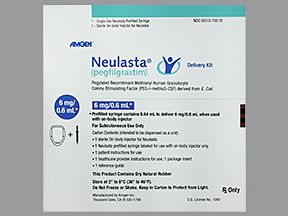
Neulasta comes in two forms. One is a single-dose prefilled syringe. This form is given as a subcutaneous injection (an injection directly under your skin).
A healthcare professional will give you the Neulasta injection, or you may be able to give yourself the injection at home after being trained. The syringe is available in one strength: 6 mg/0.6 mL.
The second form is called Neulasta Onpro, which is an on-body injector (OBI). A healthcare professional will apply it to your stomach or the back of your arm the same day you receive chemotherapy.
Neulasta Onpro delivers a dose of the drug about a day after the OBI is applied. This means you don’t have to return to your doctor’s office for an injection. Neulasta Onpro is available in one strength: 6 mg/0.6 mL.
Note: While the Neulasta syringe can be used to treat both conditions listed above, Neulasta Onpro isn’t used to treat radiation sickness.
Effectiveness
For information on the effectiveness of Neulasta, see the “Neulasta uses” section below.
Neulasta can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Neulasta. These lists don’t include all possible side effects.
For more information on the possible side effects of Neulasta, talk with your doctor or pharmacist. They can give you tips on how to deal with any side effects that may be bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs they have approved. If you would like to report to the FDA a side effect you’ve had with Neulasta, you can do so through MedWatch.
Mild side effects
The mild side effects of Neulasta can include:
- bone pain (more information in “Side effect details” below)
- pain in your arms or legs
Most of these side effects may go away within a few days or a couple of weeks. But if they become more severe or don’t go away, talk with your doctor or pharmacist.
Serious side effects
Serious side effects from Neulasta aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include:
- Aortitis (inflammation of the aorta, the main artery of the heart). Symptoms can include:
- malaise (feelings of discomfort or uneasiness)
- abdominal pain
- Thrombocytopenia (low platelet level). Symptoms can include:
- bruising
- bleeding, such as nosebleeds
- Myelodysplastic syndrome (MDS), a blood and bone marrow cancer, in people with breast or lung cancer. Symptoms can include:
- fatigue
- frequent infections
- easy bleeding or bruising
- Acute myeloid leukemia (AML), a blood cancer, in people with breast or lung cancer. Symptoms can include:
- fatigue
- swollen lymph nodes
- sweating or fever
- shortness of breath
Other serious side effects, explained in more detail below in “Side effect details,” include:
- allergic reaction
- acute respiratory distress syndrome (a type of lung condition)
- capillary leak syndrome (a condition in which tiny blood vessels leak)
- glomerulonephritis (a group of kidney conditions)
- leukocytosis (increased level of white blood cells called leukocytes)
- ruptured spleen (the opening of an organ called the spleen)
Side effect details
You may wonder how often certain side effects occur with this drug. Here’s some detail on some of the side effects that may occur with either the Neulasta shot or patch.
Allergic reaction
As with most drugs, some people can have an allergic reaction after taking Neulasta. It’s not known how many people had an allergic reaction to Neulasta in clinical trials. However, most reactions occurred in people who received a dose of Neulasta for the first time.
And in some people, the reaction occurred again days later, after the treatment for the allergic reaction was stopped. An acrylic adhesive is used with the Neulasta on-body injector (OBI) and can cause an allergic reaction if someone has an allergy to adhesives.
Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
Call your doctor right away if you have a severe allergic reaction to Neulasta. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Bone pain
Bone pain is a common side effect of Neulasta. In clinical studies, 31% of people who took Neulasta reported bone pain compared with 26% of people who took a placebo (treatment with no active drug).
It’s not known exactly why Neulasta causes bone pain in some people. One theory involves histamine, a protein that your immune system makes to help fight infections.
Neulasta stimulates your immune system into producing more white blood cells, which also leads to more histamine being created. And the release of histamine has been linked to bone marrow swelling and pain. More research is needed before it’s known for sure why Neulasta causes bone pain.
If you have bone pain while using Neulasta, tell your doctor. They may prescribe a medication for the pain, such as ibuprofen or naproxen. Or they may switch you to a medication other than Neulasta.
Acute respiratory distress syndrome (ARDS)
Acute respiratory distress syndrome (ARDS) is a possible side effect of Neulasta, but it rarely occurs. ARDS wasn’t reported during clinical trials of the drug, but the condition has been reported in a few people taking Neulasta since it came on the market.
With ARDS, your lungs become filled with fluid and can’t deliver enough oxygen to the rest of your body. This could lead to other lung problems such as pneumonia or infections.
Symptoms of ARDS can include:
- confusion
- dry, hacking cough
- feeling weak
- fever
- low blood pressure
ARDS is a potentially life threatening condition that requires prompt medical care. If you’re taking Neulasta and you have trouble breathing, a fast rate of breathing, or shortness of breath, call 911 or go to the emergency room.
Capillary leak syndrome
Capillary leak syndrome is a rare but serious potential side effect of Neulasta. It’s not known for sure how often it occurred in clinical studies.
Capillaries are tiny blood vessels. Capillary leak syndrome occurs when fluids and proteins manage to leak out of capillaries and into surrounding body tissue. This can cause low blood pressure and hypoalbuminemia (low levels of an important protein called albumin).
Symptoms of capillary leak syndrome can include:
- edema (bloating and fluid retention)
- diarrhea
- fatigue (lack of energy)
- feeling extremely thirsty
- nausea
- abdominal pain
As mentioned above, capillary leak syndrome is rare, but it can be fatal. So if you think you have symptoms of capillary leak syndrome while taking Neulasta, call 911 or go to the emergency room.
Glomerulonephritis
Although glomerulonephritis wasn’t reported in clinical studies of Neulasta, it’s been reported in people who took the drug since it came on the market.
Glomerulonephritis refers to inflammation (swelling) of the glomeruli, which are clusters of blood vessels in your kidneys. Glomeruli help filter waste products from your blood and pass them into urine.
Symptoms of glomerulonephritis can include:
- bloating and swelling due to fluid retention, especially in the face, feet, hands, or stomach
- high blood pressure
- urine that’s pink or dark brown in color
- urine that looks foamy
If you think you have glomerulonephritis while taking Neulasta, tell your doctor. They may reduce your dose, which usually clears up glomerulonephritis. If that doesn’t work, your doctor will likely have you stop taking Neulasta. They may have you try a different medication instead.
Leukocytosis
Leukocytosis is a rare but potentially serious side effect of Neulasta.
In clinical studies, leukocytosis occurred in less than 1% of people who took the drug. Neulasta was compared with a placebo, but it’s not known whether or how often leukocytosis occurred in people who took a placebo. No complications related to leukocytosis were reported in these studies.
Leukocytosis is a condition in which the level of white blood cells called leukocytes is higher than normal. This is usually a sign that your body is trying to fight an infection. However, leukocytosis can also be a sign of leukemia (a cancer that affects the bone marrow or blood).
Symptoms of leukocytosis can include:
- bleeding or bruising
- breathing problems such as wheezing
- fever
Because you’re at an increased risk for infection while taking Neulasta, tell your doctor right away if you develop a fever or other symptoms of leukocytosis. They’ll help determine the cause and what treatment is right for you.
Ruptured spleen
An enlarged spleen and a ruptured spleen weren’t reported in clinical trials of Neulasta. However, these conditions have been reported in people who took Neulasta since the drug came on the market.
The spleen is an organ that’s in the upper left of your abdomen, under your ribs. It works to filter blood and fight infection.
Symptoms of a ruptured spleen can include:
- confusion
- feeling anxious or restless
- lightheadedness
- nausea
- pain in the upper left area of the abdomen
- pale skin
- shoulder pain
A ruptured spleen is a life threatening condition requiring prompt medical care. If you’re taking Neulasta and have pain in your left shoulder or upper left abdomen area, tell your doctor right away.
Fever (not a side effect)
Fever isn’t an expected side effect of taking Neulasta.
Keep in mind, Neulasta is used to help lower the risk of infection due to a condition called febrile neutropenia. This condition causes a fever along with a low level of white blood cells called neutrophils. Neulasta is also used to treat radiation sickness, which can cause fever. So, you may have a fever while taking this drug. But the fever could be due to the conditions being treated. Your fever may not be caused by Neulasta itself.
Developing a fever during your Neulasta treatment may also mean you have an infection. Fever can also be a symptom of rare but serious side effects of Neulasta, such as acute respiratory distress syndrome (ARDS), aortitis, or leukocytosis. (For more about ARDS and leukocytosis, see those sections below.)
If you develop a fever while taking Neulasta, tell your doctor right away. They can help determine what’s causing your fever and the best way to treat it.
The Food and Drug Administration (FDA) approves prescription drugs such as Neulasta to treat certain conditions. Neulasta may also be used off-label for other conditions. Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.
Neulasta for preventing infections during chemotherapy
Chemotherapy is a type of cancer treatment that uses medications to kill dividing cancer cells. This helps prevent cancer from growing and spreading.
However, chemotherapy isn’t specific for cancer cells. Chemotherapy also destroys other dividing cells in the body, including helpful cells such as white blood cells.
Neutropenia is a blood condition in which neutrophil levels become low. Neutrophils are a type of white blood cell that protect your body from infection. If your neutrophil levels are low, your body won’t be able to properly fight off bacteria. So having neutropenia increases your risk for infection.
Febrile neutropenia occurs when you have neutropenia and develop a fever, which can be a sign of an infection. And having neutropenia means that you can’t fight infections as well as usual. So febrile neutropenia is a serious condition that a doctor should check out right away.
What Neulasta does
Neulasta is used to help prevent infection in people with certain cancers who are receiving chemotherapy. The cancers are called non-myeloid cancers, which don’t involve bone marrow (the tissue inside bones that makes blood cells). An example of a non-myeloid cancer is breast cancer.
Neulasta aids you in creating more neutrophils and other white blood cells. This helps your body be more prepared to fight infections, help prevent febrile neutropenia, and shorten how long you have neutropenia.
Effectiveness
In clinical studies, Neulasta has been shown to decrease both the risk of febrile neutropenia and how long the condition lasts in people who develop it.
One study compared Neulasta with filgrastim (Neupogen), which is another drug proven to help prevent and treat febrile neutropenia. Researchers wanted to see if Neulasta was as effective as filgrastim at shortening how long febrile neutropenia lasts.
In this study, people received a chemotherapy regimen (treatment plan) consisting of doxorubicin and docetaxel every 21 days. Similar regimens have been linked to severe neutropenia that occurred in all cases.
The condition lasted around 5 to 7 days on average, and about 30% to 40% of people developed febrile neutropenia.
The people were randomly assigned to receive either Neulasta or filgrastim. The researchers found that Neulasta was similarly effective as filgrastim.
People who received Neulasta and developed severe neutropenia had the condition for an average of 1.8 days. People who received filgrastim and developed severe neutropenia had the condition for an average of 1.6 days.
A second study with an identical setup also found similar results. People who received Neulasta and developed severe neutropenia had the condition for an average of 1.7 days. This was compared with an average of 1.6 days in people who received filgrastim.
Neulasta for radiation sickness
Neulasta is also approved by the FDA to treat radiation sickness. The condition may also be referred to as acute radiation syndrome or radiation toxicity.
The type of radiation sickness that Neulasta is used for is called hematopoietic subsyndrome. The amounts of radiation exposure that cause this syndrome are described as myelosuppressive, meaning they lead your bone marrow to make fewer blood cells.
Radiation sickness occurs when a person is exposed to high doses of radiation over a very short period of time (typically only a few minutes). High doses of radiation can kill the cells in your body. Radiation sickness can be fatal if the radiation exposure is severe enough.
For ethical reasons, researchers weren’t able to test Neulasta’s ability to treat radiation sickness in people. Instead, the drug was approved to treat radiation sickness based on animal studies, in addition to the data mentioned in the “Neulasta for preventing infections during chemotherapy” section above.
Note: Neulasta Onpro (the Neulasta on-body injector) should not be used to treat radiation sickness.
Off-label uses for Neulasta
In addition to the uses listed above, Neulasta may be used off-label in certain cases. Off-label drug use is when a drug that’s approved for one use is used for a different one that’s not approved.
Post-hematopoietic cell transplants
Neulasta isn’t FDA-approved for use post-hematopoietic cell transplant (HCT). However, the drug may be used off-label for this purpose.
An HCT is a procedure that’s performed after you’ve had chemotherapy. Once chemotherapy is used to kill cancer cells, stem cells are transplanted to you during an HCT. This is done because chemotherapy doesn’t just attack cancer cells. It can also kill stem cells made by your bone marrow.
Stem cells normally become platelets (blood cells that help your blood clot), red blood cells, and white blood cells, which are all vital in keeping you alive.
When an HCT is given to people with blood cancers, an infection can occur. This is because the new cells aren’t fully effective right after the transplant.
Using Neulasta after an HCT helps your body make new white blood cells, including neutrophils. A healthy level of neutrophils helps your body fight off infection better.
Effectiveness
Although Neulasta isn’t FDA-approved for use after an HCT, clinical studies have shown the drug is effective for this use.
One study compared Neulasta with a similar drug, filgrastim (Neupogen), which is FDA-approved to be used after an HCT. Neulasta is given as just a single injection, while filgrastim is given as multiple injections on several days.
In the study, 14 people with non-Hodgkin lymphoma, multiple myeloma, or amyloidosis received Neulasta after having an HCT.
The researchers compared the results of these people with the results of people who received filgrastim in the past. This means that there wasn’t a placebo group (treatment with no active drug).
The researchers found that it took an average of about 11 days for neutrophils to return to safe levels in people who received Neulasta. In comparison, it took an average of 14 days for people who took filgrastim in the past.
If you have questions about taking Neulasta after an HCT, talk with your doctor.
Neulasta and children
Neulasta is approved to help prevent infections in children receiving chemotherapy. The drug is also approved for use in children with radiation sickness. There are no age-based restrictions for using Neulasta.
Neulasta is available as a brand-name medication. Neulasta has four biosimilar versions: Fulphila, Nyvepria, Udenyca, and Ziextenzo.
A biosimilar is a drug that’s similar to a brand-name medication. A generic drug, on the other hand, is an exact copy of the active ingredient in a brand-name medication.
Biosimilars are based on biologic drugs, which are created from parts of living organisms. Generics are based on regular medications made from chemicals. Biosimilars and generics also tend to cost less than brand-name drugs.
Neulasta contains one active drug ingredient: pegfilgrastim. This means pegfilgrastim is the ingredient that makes Neulasta work.
The Neulasta dosage your doctor prescribes will depend on several factors. These include:
- the type and severity of the condition you’re using Neulasta to treat
- your age
- the form of Neulasta you take
- other medical conditions you may have
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to fit your needs.
Drug forms and strengths
Neulasta comes in two forms. One is a single-dose prefilled syringe. This form is given as a subcutaneous injection (an injection directly under your skin).
A healthcare professional will give you the Neulasta injection, or you may be able to give yourself the injection at home after being trained. The syringe is available in one strength: 6 mg/0.6 mL.
The second form is called Neulasta Onpro, which is an on-body injector (OBI). A healthcare professional will apply it to your stomach or the back of your arm the same day you receive chemotherapy.
Neulasta Onpro delivers a dose of the drug about a day after the OBI is applied. This means you don’t have to return to your doctor’s office for an injection. Neulasta Onpro is available in one strength: 6 mg/0.6 mL.
It’s important to note that Neulasta Onpro is not used to treat radiation sickness.
Dosage for preventing infections during chemotherapy
For preventing infection during chemotherapy, Neulasta is given as a single dose once each chemotherapy cycle. A single dose is either one injection with the syringe or the use of one Neulasta Onpro.
You should not use Neulasta either 14 days before or 24 hours after having chemotherapy.
Dosage for radiation sickness
For treating hematopoietic subsyndrome of acute radiation syndrome (radiation sickness), Neulasta is given as two doses. You’ll have them 1 week apart. A single dose is one injection with the syringe.
Pediatric dosage
Neulasta is approved to help prevent infections in children receiving chemotherapy. The drug is also approved for use in children with radiation sickness. There are no age-based restrictions for using Neulasta.
For Neulasta dosages in children who weigh more than 99 pounds (lb), about 45 kilograms (kg), see the dosage sections above.
Dosages for children who weigh less than 99 lb (45 kg) are based on weight. Your child’s doctor will determine what Neulasta dosage is right for your child.
What if I miss a dose?
If you miss giving yourself an injection of Neulasta with a syringe, call your doctor as soon as you realize this. They can advise you on when you take your dose.
If you miss an appointment for a Neulasta injection, call your doctor’s office. The staff can reschedule you and adjust the timing of future visits, if necessary.
It’s also possible to miss a dose while using Neulasta Onpro. This is because the on-body injector can sometimes fail to work or leak. If this happens, call your doctor’s office right away. The staff will schedule a time for you to come in for a Neulasta injection so that you receive your full dose.
To help make sure that you don’t miss a dose, try setting a reminder on your phone. You can also write your treatment schedule in a calendar.
Will I need to use this drug long term?
Whether you’ll use Neulasta as a long-term treatment depends on the reason you’re taking the drug.
For preventing infections during chemotherapy, Neulasta is meant to be used as a long-term treatment. If you’re receiving chemotherapy, and your doctor determines that Neulasta is safe and effective for you, you’ll likely take it long term.
For radiation sickness, you’ll only take two doses of the drug. Neulasta isn’t typically used as a long-term treatment for this purpose.
Here are answers to some frequently asked questions about Neulasta.
Can Claritin help me manage side effects of Neulasta?
Possibly. Neulasta works by triggering your immune system to make more white blood cells.
Certain proteins called histamines are also released by this process. It’s not exactly known why the release of histamines leads to side effects such as bone pain. But research has shown that histamine is involved in inflammation, which can cause pain.
Claritin is an antihistamine medication. It works by blocking the action of histamine. By doing so, Claritin may help reduce bone pain in people taking Neulasta, but more research is needed.
If you’re taking Neulasta and having bone pain, talk with your doctor. They can review available treatments and help determine which one is best for you.
How long do side effects of the Neulasta shot last?
It’s not known because there isn’t enough data on how long side effects of the Neulasta shot last.
In clinical studies, some people reported bone pain or pain in their arms or legs after receiving Neulasta. But the researchers didn’t record how long the side effects lasted.
For more details on potential side effects of Neulasta, please refer to the “Neulasta side effects” section above. You can also reach out to your doctor.
How long does Neulasta stay in your system?
The timing can vary. Clinical studies showed that clearing Neulasta from the body is affected by your body weight and the number of neutrophils (a type of white blood cell) present in your blood.
In general, after one injection, Neulasta is completely eliminated from your system within 14 days.
When I fly, do I need to tell airport security that I have Neulasta Onpro?
Yes. The manufacturer of Neulasta has a Transportation Security Administration (TSA) notification card that you can print and present to security personnel at the airport. Click here to access the card.
However, it’s recommended that you avoid traveling (including driving) during the 26- to 29-hour window after you receive Neulasta Onpro. The device is dispensing the drug into your body during this time. And traveling may increase the risk of Neulasta Onpro getting knocked off your body.
If you have questions about your Neulasta treatment while traveling, talk with your doctor.
Why do I have to keep Neulasta Onpro away from cell phones and other electrical devices?
The signals from these electrical devices may interfere with Neulasta Onpro and keep it from providing your dose.
It’s recommended that you keep Neulasta Onpro at least 4 inches away from electrical devices, including cell phones and microwaves.
If you have questions about using Neulasta Onpro, ask your doctor.
How should I dispose of Neulasta Onpro?
After you’ve received your full dose of Neulasta by using Neulasta Onpro, you should dispose of the device by putting it in a Sharps container.
The manufacturer of Neulasta has a Sharps Disposal Container Program to help you safely dispose of Neulasta Onpro. This is offered at no additional cost to you. To sign up for the program, you can click here (see the “Injector Disposal Program” section) or call 844-696-3852.
Neulasta is typically used with other drugs. This is because Neulasta is only one part of a cancer treatment regimen (plan).
Neulasta is commonly used with chemotherapy because Neulasta helps prevent or treat side effects of chemotherapy.
Commonly used chemotherapy drugs include:
- bleomycin
- carboplatin
- cyclophosphamide
- docetaxel (Taxotere)
- doxorubicin (Doxil)
- gemcitabine (Infugem)
- paclitaxel (Abraxane)
Keep in mind that this is not a full list of chemotherapy medications. Talk with your doctor if you have questions about any chemotherapy drugs and whether Neulasta might benefit you.
Other drugs are available that can treat your condition. Some may be a better fit for you than others. If you’re interested in finding an alternative to Neulasta, talk with your doctor. They can tell you about other medications that may work well for you.
Note: Some of the drugs listed below are used off-label to treat these specific conditions. Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.
Alternatives for preventing infections during chemotherapy
Examples of other drugs that may be used to help prevent infections during chemotherapy include:
- tbo-filgrastim (Granix)
- pegfilgrastim-jmdb (Fulphila)
- sargramostim (Leukine)
- filgrastim (Neupogen)
- filgrastim-aafi (Nivestym)
- pegfilgrastim-cbqv (Udenyca)
- filgrastim-sndz (Zarxio)
- pegfilgrastim-bmez (Ziextenzo)
- pegfilgrastim-apgf (Nyvepria)
Alternatives for radiation sickness
Examples of other drugs that may be used to treat radiation sickness include:
- potassium iodide
- Prussian blue
- filgrastim (Neupogen)
- filgrastim-aafi (Nivestym)
- filgrastim-sndz (Zarxio)
- romiplostim (Nplate)
- sargramostim (Leukine)
Neulasta is a biologic medication, which means it’s created from parts of living organisms. It has four biosimilar versions, including Udenyca.
A biosimilar version is a drug that’s similar to a brand-name biologic drug. To learn more, see the “Neulasta generic or biosimilar” section above.
Uses
Both Neulasta and Udenyca are approved by the Food and Drug Administration (FDA) to reduce the risk of infection due to a condition called febrile neutropenia in people with non-myeloid cancers.* To use these medications, you must be taking an anticancer drug that could cause febrile neutropenia.
Neulasta is also FDA-approved to treat radiation sickness.* The type of radiation sickness that Neulasta is used for is called hematopoietic subsyndrome.
* For detailed information on these conditions, see the “Neulasta uses” section.
Drug forms and administration
Neulasta comes in two forms. One is a single-dose prefilled syringe. This form is given as a subcutaneous injection (an injection directly under your skin).
A healthcare professional will give you the Neulasta injection, or you may be able to give yourself the injection at home after being trained.
The second form is called Neulasta Onpro, which is an on-body injector (OBI). A healthcare professional will apply it to your stomach or the back of your arm the same day you receive chemotherapy.
Neulasta Onpro delivers a dose of the drug about a day after the OBI is applied. This means you don’t have to return to your doctor’s office for an injection.
Udenyca comes in a single-dose prefilled syringe and is also given by subcutaneous injection. Healthcare professionals may administer the drug, or they may show you how to inject the drug at home.
Note: Neulasta Onpro is not used to treat radiation sickness.
Side effects and other information
Neulasta and Udenyca share several mild and serious side effects. To view lists of Neulasta’s side effects, see the “Neulasta side effects” section above. To read about Udenyca’s side effects, view the drug’s prescribing information.
Because Udenyca is a biosimilar of Neulasta, these drugs are expected to have the same effectiveness and safety.
To learn more about how Neulasta compares with Udenyca, talk with your doctor. They can discuss which drug is best for your condition.
You may wonder how Neulasta compares with other medications that are prescribed for similar uses. Here we look at how Neulasta and Granix are alike and different.
Ingredients
Neulasta contains the active drug pegfilgrastim. Granix contains the active drug tbo-filgrastim.
Both pegfilgrastim and tbo-filgrastim belong to a class of medications known as granulocyte-colony stimulating factors (G-CSFs). A medication class is a group of drugs that work in a similar way.
A G-CSF is a medication that causes neutrophils (a type of white blood cell) to grow in your bone marrow. Bone marrow is the tissue inside bones that makes blood cells. G-CSFs are man-made copies of the G-CSF hormone your body makes naturally.
Uses
Both Neulasta and Granix are approved by the Food and Drug Administration (FDA) to reduce the risk of infection due to a condition called febrile neutropenia in people with non-myeloid cancers.* To use these medications, you must be taking an anticancer drug that could cause febrile neutropenia.
Neulasta is also FDA-approved to treat radiation sickness.* The type of radiation sickness that Neulasta is used for is called hematopoietic subsyndrome.
* For detailed information on these conditions, see the “Neulasta uses” section.
Drug forms and administration
Here’s some information about the forms of Neulasta and Granix and how they’re given.
Neulasta forms
Neulasta comes in two forms. One is a single-dose prefilled syringe. This form is given as a subcutaneous injection (an injection directly under your skin).
A healthcare professional will give you the Neulasta injection, or you may be able to give yourself the injection at home after being trained.
The second form is called Neulasta Onpro, which is an on-body injector (OBI). A healthcare professional will apply it to your stomach or the back of your arm the same day you receive chemotherapy.
Neulasta Onpro delivers a dose of the drug about a day after the OBI is applied. This means you don’t have to return to your doctor’s office for an injection.
Note: Neulasta Onpro isn’t used to treat radiation sickness.
Granix forms
Granix also comes in two forms: a single-dose prefilled syringe and a single-dose vial of liquid solution. Both forms can be given by a healthcare professional as an injection subcutaneously, directly under your skin. But with some training, you may be able to give yourself injections at home.
Dosage frequency
One important difference between Neulasta and Granix is how often the drugs are given to reduce the risk of infection during chemotherapy.
Neulasta is given only once during each chemotherapy cycle. Granix, on the other hand, is given every day until the levels of neutrophils in your blood return to normal.
Side effects and risks
Neulasta and Granix are both used to help prevent infections during chemotherapy. Therefore, these medications can cause some similar side effects, but some different ones as well. Below are examples of these side effects.
Mild side effects
These lists contain examples of mild side effects that can occur with Neulasta, with Granix, or with both drugs (when taken individually).
- Can occur with Neulasta:
- few unique side effects
- Can occur with Granix:
- headache
- muscle aches
- vomiting
- Can occur with both Neulasta and Granix:
- bone pain
- pain in your arms or legs
Serious side effects
These lists contain examples of serious side effects that can occur with Neulasta, with Granix, or with both drugs (when taken individually).
- Can occur with Neulasta:
- myelodysplastic syndrome, in certain people
- acute myeloid leukemia, in certain people
- Can occur with Granix:
- cutaneous vasculitis (inflammation of the skin’s blood vessels)
- sickle cell disorders (a group of disorders affecting red blood cells, specifically hemoglobin)
- Can occur with both Neulasta and Granix:
- leukocytosis (increased level of white blood cells)
- ruptured spleen (the opening of an organ called the spleen)
- acute respiratory distress syndrome (a type of lung condition)
- glomerulonephritis (a group of kidney conditions)
- capillary leak syndrome (a condition in which tiny blood vessels leak)
- aortitis (inflammation of the aorta, the main artery of the heart)
- thrombocytopenia (low platelet level)
Effectiveness
The only use both Neulasta and Granix are approved for is reducing the risk of infection due to a condition called febrile neutropenia in people with non-myeloid cancers.
Separate studies of the two drugs were compared in a larger review of studies called a systemic review. Researchers looked at data from 18 studies.
People had received pegfilgrastim (the active drug in Neulasta), filgrastim, or a similar drug, including Granix. The pegfilgrastim group was less likely to develop febrile neutropenia and less likely to require a hospital stay as a result of febrile neutropenia. This was compared with the other drug groups.
Costs
Neulasta and Granix are both brand-name drugs.
Neulasta has four biosimilar versions: Fulphila, Nyvepria, Udenyca, and Ziextenzo.
Granix isn’t technically considered to be a biosimilar, according to the FDA.
A biosimilar is a drug that’s similar to a brand-name medication. A generic drug, on the other hand, is an exact copy of the active ingredient in a brand-name medication.
Biosimilars are based on biologic drugs, which are created from parts of living organisms. Generics are based on regular medications made from chemicals. Biosimilars and generics also tend to cost less than brand-name drugs.
The actual price you’ll pay for either drug will depend on your insurance plan, your location, and the pharmacy you use.
Like Granix (discussed above), the drug Fulphila has uses similar to those of Neulasta. Here’s a comparison of how Neulasta and Fulphila are alike and different.
Ingredients
Neulasta and Fulphila contain the same active drug, pegfilgrastim.
Technically, Fulphila contains the active ingredient pegfilgrastim-jmdb. This is because Fulphila is a type of drug known as a biosimilar. A biosimilar is a drug that’s similar to a brand-name medication. Biosimilars are based on biologic drugs, which are created from parts of living organisms.
In this case, Neulasta is the biologic drug, and Fulphila is the biosimilar of it. Pegfilgrastim and pegfilgrastim-jmdb both work in the same way.
Pegfilgrastim belongs to a class of medications known as granulocyte-colony stimulating factors (G-CSFs). A class of medications is a group of drugs that work in a similar way.
A G-CSF is a medication that causes neutrophils (a type of white blood cell) to grow in your bone marrow. Bone marrow is the tissue inside bones that makes blood cells. And G-CSFs are man-made copies of the G-CSF hormone your body makes naturally.
Uses
Both Neulasta and Fulphila are approved by the Food and Drug Administration (FDA) to reduce the risk of infection due to a condition called febrile neutropenia in people with non-myeloid cancers.* To use these medications, you must be taking an anticancer drug that could cause febrile neutropenia.
Neulasta is also FDA-approved to treat radiation sickness.* The type of radiation sickness that Neulasta is used for is called hematopoietic subsyndrome.
Fulphila isn’t approved to help move blood cells from bone marrow into the blood for a hematopoietic cell transplant (HCT).
* For detailed information on these conditions, see the “Neulasta uses” section.
Drug forms and administration
Both Neulasta and Fulphila come as a single-dose prefilled syringe. This form is given as a subcutaneous injection (an injection directly under your skin).
A healthcare professional will give you the Neulasta or Fulphila injection, or you may be able to give yourself the injection at home after being trained.
Neulasta also comes in another form called Neulasta Onpro, which is an on-body injector (OBI). A healthcare professional will apply it to your stomach or the back of your arm the same day you receive chemotherapy.
Neulasta Onpro delivers a dose of the drug about a day after the OBI is applied. This means you don’t have to return to your doctor’s office for an injection.
Note: Neulasta Onpro isn’t used to treat radiation sickness.
Side effects and risks
Neulasta and Fulphila both contain pegfilgrastim. Therefore, these medications can cause very similar side effects. Below are examples of these side effects.
Mild side effects
This list contains examples of mild side effects that can occur with Neulasta and Fulphila (when taken individually):
- bone pain
- pain in your arms or legs
Serious side effects
This list contains examples of serious side effects that can occur with Neulasta and Fulphila (when taken individually):
- allergic reaction
- acute respiratory distress syndrome (a type of lung condition)
- aortitis (inflammation of the aorta, the main artery of the heart)
- capillary leak syndrome (a condition in which tiny blood vessels leak)
- glomerulonephritis (a group of kidney conditions)
- leukocytosis (increased level of white blood cells)
- ruptured spleen (the opening of an organ called the spleen)
- thrombocytopenia (low platelet level)
- myelodysplastic syndrome, in certain people
- acute myeloid leukemia, in certain people
Effectiveness
The only use both Neulasta and Fulphila are approved for is reducing the risk of infection due to a condition called febrile neutropenia in people with non-myeloid cancers.
These drugs haven’t been directly compared in clinical studies, but studies have found both Neulasta and Fulphila to be effective for reducing the risk of infection due to a condition called febrile neutropenia in people with non-myeloid cancers.
Costs
The actual price you’ll pay for either drug will depend on your insurance plan, your location, and the pharmacy you use.
Generics or biosimilars
Many typical drugs that are made from chemicals have generic versions. A generic drug is an exact copy of the active ingredient in a brand-name medication. It often costs less than the brand-name version.
However, Neulasta and Fulphila are both brand-name biologic drugs, which are created from parts of living organisms. Instead of generics, biologic drugs have biosimilars. A biosimilar is a drug that’s similar to a biologic drug.
Like generics, biosimilars often cost less than the brand-name biologic they’re based on.
Neulasta has four biosimilar versions: Fulphila, Nyvepria, Udenyca, and Ziextenzo. So Fulphila is a biosimilar of Neulasta. If you’d like to learn more about biosimilar versions of Neulasta, including Fulphila, talk with your doctor or pharmacist.
Here’s some information about what Neulasta treats and how the drug works.
Febrile neutropenia
Neulasta helps reduce the risk of infection due to a condition called febrile neutropenia in people with non-myeloid cancers.
Neutropenia is a blood condition in which neutrophil levels become low. Neutrophils are a type of white blood cell that protect your body from infection. If your neutrophil levels are low, your body won’t be able to properly fight off bacteria. So having neutropenia increases your risk for infection.
Febrile neutropenia occurs when you have neutropenia and develop a fever, which can be a sign of an infection. And having neutropenia means that you can’t fight infections as well as usual. So febrile neutropenia is a serious condition that a doctor should check out right away.
Non-myeloid cancers are cancers that don’t involve bone marrow, which is the tissue inside bones that makes blood cells. An example of a non-myeloid cancer is breast cancer.
Radiation sickness
Neulasta is also used to treat radiation sickness, a condition that occurs when you’re exposed to high levels of radiation. It may also be referred to as acute radiation syndrome.
The type of radiation sickness that Neulasta is used for is called hematopoietic subsyndrome. The amounts of radiation exposure that cause this syndrome are described as myelosuppressive, meaning they lead your bone marrow to make fewer blood cells.
How Neulasta works
Granulocyte-colony stimulating factor (G-CSF) is a hormone that causes neutrophils to grow in your bone marrow.
The active drug in Neulasta, pegfilgrastim, is a man-made copy of the G-CSF hormone your body makes naturally. Pegfilgrastim works in the same exact way that natural G-CSF does.
Neulasta aids you in creating more neutrophils and other white blood cells. This helps your body be more prepared to fight infections, prevent febrile neutropenia, and shorten how long you have neutropenia.
For hematopoietic subsyndrome due to radiation sickness, Neulasta helps your body replace white blood cells that were destroyed in the bone marrow by radiation exposure.
How long does it take to work?
Neulasta begins to work shortly after it’s injected into your body.
However,
When used for radiation sickness, it may take several days for Neulasta to help your body replace white blood cells that were destroyed.
Currently, there are no known interactions between Neulasta and alcohol.
However, alcohol may interfere with some chemotherapy drugs or make their side effects worse.
If you drink alcohol, talk with your doctor about whether it is safe for you to drink during your chemotherapy treatment. (Neulasta is given after a dose of chemotherapy.)
There aren’t any known interactions between Neulasta and other medications, herbs and supplements, and foods.
Neulasta and other medications
It isn’t known whether there are any drug interactions between Neulasta and other medications. This is because no formal studies have been done to detect drug interactions. Based on how the drug works, interactions with other medications are unlikely.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Neulasta and herbs and supplements
There aren’t any herbs or supplements that have been specifically reported to interact with Neulasta. However, you should still check with your doctor or pharmacist before using any of these products while taking Neulasta.
Neulasta and foods
There aren’t any foods that have been specifically reported to interact with Neulasta. If you have any questions about eating certain foods while taking Neulasta, talk with your doctor.
As with all medications, the cost of Neulasta can vary. The actual price you’ll pay will depend on your insurance plan, your location, and the pharmacy you use.
It’s important to note that you’ll have to get Neulasta at a specialty pharmacy. This type of pharmacy is authorized to carry specialty medications. These are drugs that may be expensive or may require help from healthcare professionals to be used safely and effectively.
Your insurance plan may require you to get prior authorization before they approve coverage for Neulasta. This means that your doctor and insurance company will need to communicate about your prescription before the insurance company will cover the drug. The insurance company will review the request and let you and your doctor know if your plan will cover Neulasta.
If you’re not sure if you’ll need to get prior authorization for Neulasta, contact your insurance plan.
Financial and insurance assistance
If you need financial support to pay for Neulasta, or if you need help understanding your insurance coverage, help is available.
Amgen Inc., the manufacturer of Neulasta, offers programs called Amgen FIRST STEP and Amgen Assist 360. For more information and to find out if you’re eligible for support, call 888-657-8371 or visit the manufacturer’s website.
Generic version
Neulasta is available in four biosimilar versions: Fulphila, Nyvepria, Udenyca, and Ziextenzo.
A biosimilar is a drug that’s similar to a brand-name medication. A generic drug, on the other hand, is an exact copy of the active ingredient in a brand-name medication.
Biosimilars are based on biologic drugs, which are created from parts of living organisms. Generics are based on regular medications that are made from chemicals. Biosimilars and generics also tend to cost less than brand-name drugs.
The actual price you’ll pay will depend on your insurance plan, your location, and the pharmacy you use.
If your doctor has prescribed Neulasta and you’re interested in using Fulphila, Udenyca, and Ziextenzo instead, talk with your doctor. They may have a preference for one version or the other. You’ll also need to check your insurance plan, as it may only cover one or the other.
You should take Neulasta according to your doctor or healthcare professional’s instructions.
When to take
Neulasta comes in two forms. One is a single-dose prefilled syringe. This form is given as a subcutaneous injection (an injection directly under your skin). A healthcare professional will give you the Neulasta injection, or you may be able to give yourself the injection at home after being trained.
The second form is called Neulasta Onpro. It’s an on-body injector (OBI) that a healthcare professional will apply to your stomach or the back of your arm. They’ll do this on the same day you receive chemotherapy.
Then the OBI will automatically deliver your Neulasta dose about 27 hours after being attached. This means you don’t need to return to your doctor’s office for an injection.
It’s important to note that Neulasta Onpro isn’t used to treat radiation sickness.
It isn’t known if Neulasta is safe to take during pregnancy.
Studies have been done in pregnant animals that were given filgrastim (a drug similar to Neulasta). Researchers found no increased risk of:
- congenital anomalies (also called birth defects)
- pregnancy loss
- health problems for the pregnant animal or fetus
However, animal studies don’t always reflect what happens in humans. More research on Neulasta and pregnancy is needed.
If you’re pregnant or planning to become pregnant, talk with your doctor before using Neulasta. They can explain the risks and benefits of the drug as well as other treatment options.
It’s not known if Neulasta is safe to take during pregnancy. (See the “Neulasta and pregnancy” section above to learn more.)
If you’re sexually active and you or your partner can become pregnant, talk with your doctor about your birth control needs while you’re using Neulasta.
It isn’t known whether it’s safe to take Neulasta while breastfeeding.
It also isn’t known whether the active drug in Neulasta, pegfilgrastim, is present in human breast milk.
If you’re taking Neulasta and considering breastfeeding, talk with your doctor.
This drug comes with several precautions. Before taking Neulasta, talk with your doctor about your health history. Neulasta may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Certain blood cancers. If you have a myeloid cancer (a cancer that involves bone marrow), you shouldn’t use Neulasta. The drug may cause tumor growth in people with certain blood cancers, specifically myeloid cancers. Tumors are masses of cancerous tissue. Ask your doctor what other treatments might be better choices for you.
- Sickle cell disorders. Taking Neulasta when you have a sickle cell disorder may cause a sickle cell crisis, which can be fatal. (This disorder affects hemoglobin, which is found in red blood cells.) If you have a sickle cell disorder, talk with your doctor before using Neulasta. They can recommend the best treatment options for you.
- Breast cancer or lung cancer. If you have breast or lung cancer, you have an increased risk of myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML) with Neulasta. MDS is a blood and bone marrow cancer. And AML is a blood cancer. Your doctor will monitor you for these conditions during Neulasta treatment.
- Allergy to acrylics. If you’re allergic to acrylic adhesives, you shouldn’t use Neulasta Onpro, the Neulasta on-body injector. The device uses an acrylic adhesive. Ask your doctor if the Neulasta prefilled syringe is a good choice for you.
- Allergy to latex. If you have a latex allergy, you shouldn’t use Neulasta prefilled syringes. The needle cap on the syringes contains a natural rubber derived from latex. Ask your doctor if the Neulasta Onpro on-body injector is a good choice for you.
- Allergy to Neulasta. If you’re allergic to Neulasta or any of its ingredients, you shouldn’t use the drug. Ask your doctor about other treatment options.
- Pregnancy. It isn’t known whether Neulasta is safe to use during pregnancy. For more information, please see the “Neulasta and pregnancy” section above.
- Breastfeeding. It isn’t known whether it’s safe to take Neulasta while breastfeeding. For more information, please see the “Neulasta and breastfeeding” section above.
Note: For more information about the potential negative effects of Neulasta, see the “Neulasta side effects” section above.
Using more than the recommended dosage of Neulasta can lead to serious side effects.
Overdose symptoms
Symptoms of an overdose can include:
- bloating and fluid retention
- bone pain
- shortness of breath
- pleural effusion (water buildup around the lungs)
What to do in case of overdose
If you think you’ve taken too much of this drug, call your doctor. You can also call the American Association of Poison Control Centers at 800-222-1222 or use their online tool. But if your symptoms are severe, call 911 or go to the nearest emergency room right away.
When you get Neulasta from the pharmacy, the pharmacist will add an expiration date to the label on the box or carton. This date is typically 1 year from the date they dispensed the medication.
The expiration date helps guarantee that the medication is effective during this time. The
If you have unused medication that has gone past the expiration date, talk with your pharmacist about whether you might still be able to use it.
Storage
How long a medication remains good can depend on many factors, including how and where you store the medication.
You should store Neulasta prefilled syringes in a refrigerator (36°F to 46°F / 2°C to 8°C). Don’t freeze them. But if they do become frozen, let the syringes defrost in the refrigerator before you use them. If a syringe is frozen more than one time, dispose of it.
You should also dispose of any syringes that you’ve kept at room temperature for longer than 48 hours. Finally, never shake Neulasta syringes.
Disposal
Here’s some information on how to safely dispose of Neulasta prefilled syringes and Neulasta Onpro.
Neulasta prefilled syringes
Right after you’ve used a Neulasta prefilled syringe, dispose of it in an
You can buy a sharps container online, or ask your doctor, pharmacist, or health insurance company where to get one.
This article provides several useful tips on medication disposal. You can also ask your pharmacist for information on how to dispose of your syringes.
Neulasta Onpro
If you use Neulasta Onpro, there are special disposal instructions. After you receive your full dose, you should put Neulasta Onpro in a sharps container.
The manufacturer of Neulasta Onpro has a Sharps Disposal Container Program to help you safely dispose of Neulasta Onpro. This is offered at no additional cost to you. You can click here to sign up for the program, or call 844-696-3852.
The following information is provided for clinicians and other healthcare professionals.
Indications
Neulasta is indicated for reducing infection risk in patients with non-myeloid malignancies being treated with myelosuppressive anticancer treatment that causes febrile neutropenia.
Neulasta is also approved for increasing survival in people with hematopoietic subsyndrome of acute radiation syndrome (radiation sickness).
Mechanism of action
The active ingredient in Neulasta, pegfilgrastim, is a synthetic colony-stimulating factor. It binds to receptors on the cell surface of hematopoietic cells, triggering their proliferation, differentiation, and activation. This results in an increase in absolute neutrophil count (ANC).
Pharmacokinetics and metabolism
The serum half-life of Neulasta after subcutaneous administration ranges from 15 to 80 hours.
Patients with a higher body weight experienced higher systemic exposure to Neulasta in clinical trials, highlighting the importance of following weight-based dosing recommendations provided by the manufacturer.
Although the manufacturer doesn’t offer specific pharmacokinetic information with regard to duration of effect, clinical studies have shown that ANC takes approximately 10 to 14 days from the date of chemotherapy administration to recover to normal levels when Neulasta is administered the day following chemotherapy.
Neulasta peak concentration
After subcutaneous administration, peak Neulasta concentrations occur around 16 to 120 hours post-dose.
Contraindications
Neulasta is contraindicated in patients with history of serious allergic reaction to either pegfilgrastim or filgrastim.
Storage
Neulasta prefilled syringes should be refrigerated between 36°F and 46°F (2°C and 8°C). The syringes should be kept in the original carton to protect from light. Syringes left at room temperature for longer than 48 hours should be disposed of.
Do not freeze the syringes. But if the syringes become frozen, defrost them in a refrigerator before using. Dispose of any syringes that have been frozen more than one time.
Neulasta Onpro kits should be refrigerated between 36°F and 46°F (2°C and 8°C) until 30 minutes before using them. Don’t keep the kits at room temperature for more than 12 hours before using them. If the kits are kept at room temperature for longer than 12 hours, dispose of them.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.