Promacta is a brand-name prescription drug that’s used to treat certain blood disorders.
Promacta contains the active ingredient eltrombopag, which is a type of medication known as a thrombopoietin receptor agonist. (Thrombopoietin is a hormone involved in making platelets, which are parts of your blood that help it clot.)
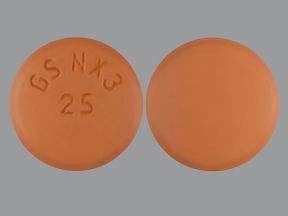
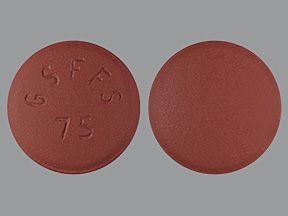
Promacta comes in two forms. One is a tablet that you swallow. It’s available in these strengths: 12.5 mg, 25 mg, 50 mg, and 75 mg.
The second form is a packet of powder. You’ll mix it with water to create a suspension (liquid) and use this with an oral syringe. The packet is available in these strengths: 12.5 mg and 25 mg.
What it does
Promacta is FDA-approved to treat these conditions:
- Thrombocytopenia (low platelet count) in adults as well as children ages 1 year and older who have chronic immune thrombocytopenia. With chronic immune thrombocytopenia (ITP), low levels of platelets cause bleeding that appears as rashes. To be prescribed Promacta for this condition, you must have already tried treatments that didn’t work. These treatments include immunoglobulins (injections of proteins), corticosteroids, or splenectomy (the removal of your spleen). Even when other treatment options have failed, you should take Promacta only if you have an increased risk for bleeding.
- Thrombocytopenia in adults with chronic hepatitis C who need to start taking a medication called interferon for their condition. (Chronic hepatitis C is a type of liver infection.) You should use Promacta only if you haven’t been able to start taking or keep taking interferon for chronic hepatitis C without Promacta.
- Severe aplastic anemia. With severe aplastic anemia (SAA), the stem cells in your bone marrow become damaged. Promacta is used in two ways to treat SAA:
- It’s used with immunosuppressive therapy in adults as well as children ages 2 years and older. This is a kind of treatment that decreases the activity of your immune system.
- It’s used to treat SAA in adults that’s refractory.A condition is called refractory when it hasn’t been helped by previous treatment. In this case, people with SAA have tried immunosuppressive therapy in the past, but it wasn’t successful.
Promacta shouldn’t be used to treat myelodysplastic syndrome (MDS), a group of cancers of the blood and bone marrow. And it’s not known whether it’s safe and effective to use Promacta to treat chronic hepatitis C with drugs called direct-acting antiviral agents, but without interferon.
Effectiveness
Clinical studies of adults with chronic ITP compared Promacta with a placebo (treatment with no active drug). The success of treatment was based on desired platelet count increases at any point during treatment. (A desired platelet count increase is the amount your platelets should increase while taking the medication.) The increases were found in 59% to 70% of adults who took Promacta compared with 11% to 16% of those who took a placebo.
For information about the effectiveness of Promacta in treating other conditions, see the “Promacta uses” section below.
Promacta is available only as a brand-name medication. It’s not currently available in generic form. A generic drug is an exact copy of the active drug in a brand-name medication.
Promacta contains one active drug ingredient: eltrombopag. This means eltrombopag is the ingredient that makes Promacta work.
Promacta can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Promacta. These lists don’t include all possible side effects.
For more information on the possible side effects of Promacta, talk with your doctor or pharmacist. They can give you tips on how to deal with any side effects that may be bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs they have approved. If you would like to report to the FDA a side effect you’ve had with Promacta, you can do so through MedWatch.
Mild side effects
Many of these mild side effects occurred in people who were taking other medications with Promacta. So it’s hard to say whether Promacta caused all these side effects.
The mild side effects of Promacta that are more common* can include:
- mild anemia (low count of red blood cells or unhealthy red blood cells)
- nausea
- fever
- cough
- fatigue (lack of energy)
- headache
- diarrhea
- small increases in the level of a liver enzyme called alanine aminotransferase (ALT), which may be a symptom of liver damage
The mild side effects of Promacta that are less common** can include:
- vomiting
- upper respiratory infection (URI), such as the common cold
- urinary tract infection
- muscle aches
- sore throat
- back pain
- flu
- tickling, burning, or prickling feeling on the skin
- rash
- hair loss
- dry mouth
- small increases in the level of a liver enzyme called aspartate aminotransferase (AST), which may be a symptom of liver damage
- changes in skin color, including darker patches or yellowing of skin
* occurred in 20% or more of people in clinical studies
** occurred in less than 20% of people in clinical studies
Serious side effects
Many of these serious side effects occurred in people who were taking other medications with Promacta. So it’s hard to say whether Promacta caused all these side effects.
Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include:
- Cataracts (an eye problem). Symptoms can include:
- cloudy or blurry vision
- sudden change in eyesight
- Hemorrhage (bleeding). Symptoms can include:
- bleeding
- bruising
- blood in urine or stool
- dizziness
- weakness
- Thromboembolism (a blood clot in a blood vessel). Symptoms can include:
- swelling, pain, or tenderness in an arm or leg
- shortness of breath
- pain in your belly area with nausea, vomiting, or diarrhea
- Severe anemia. Symptoms can include:
- weakness
- extreme tiredness
- pale skin
- dizziness
Other serious side effects, explained in more detail below in “Side effect details,” include:
- allergic reaction
- hepatotoxicity (harm to the liver)*
* Promacta has
Side effects in children
Side effects reported in children were similar to those seen in adults.
Studies looked at how often upper respiratory infections (URIs) occurred in children who took Promacta or a placebo (treatment with no active drug). In children ages 1 year and older with chronic immune thrombocytopenia (ITP), 17% of those who took Promacta had URIs. This was compared with 6% of children who took a placebo.
Studies also looked at how often diarrhea occurred. In children ages 1 year and older with chronic ITP, 9% of those who took Promacta had diarrhea. This was compared with 2% of those who took a placebo.
For more details about side effects, please see the side effects lists above and side effect details below.
Side effect details
You may wonder how often certain side effects occur with this drug. Here’s some detail on several of the side effects this drug may cause.
Allergic reaction
As with most drugs, some people can have an allergic reaction after taking Promacta. However, it’s not known how often allergic reactions occur with Promacta. Clinical studies don’t include reports of allergic reactions or the frequency of such reactions.
Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (warmth and redness in your skin)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing or speaking
Call your doctor right away if you have a severe allergic reaction to Promacta. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Upper respiratory infection
URIs may occur with Promacta. Studies looked at how often URIs occurred in adults who took Promacta or a placebo (treatment with no active drug). In adults with chronic immune thrombocytopenia (ITP), URIs were reported in 7% of adults who took Promacta. This was compared with 6% of adults who took a placebo.
URIs can cause common cold symptoms, such as:
- cough
- runny or stuffy nose
- sore throat
These symptoms should usually go away within 1 to 2 weeks. But if you develop symptoms that bother you, tell your doctor. They can suggest ways to help treat your URI.
Nausea
It’s fairly common to have nausea when taking Promacta. Studies showed that nausea occurred in about 9% of adults with chronic ITP who took Promacta. This was compared with 3% of adults who took a placebo.
The studies also looked at how often nausea occurred in adults with chronic hepatitis C and those with severe aplastic anemia (SAA). Information on these studies is available in the Promacta prescribing information.
If you have nausea that causes you discomfort, trouble with day-to-day activities, or is severe, tell your doctor. They can prescribe medication to help you feel better or recommend other treatment options for your condition.
Diarrhea
Diarrhea may occur with Promacta. Studies of adults with chronic ITP found that 9% of people who took Promacta had diarrhea. This was compared with 7% of adults who took a placebo.
The studies also looked at how often nausea occurred in adults with chronic hepatitis C and those with SAA. Information on these studies is available in the Promacta prescribing information.
If you have diarrhea that bothers you or is severe, tell your doctor. It’s important you don’t become dehydrated. So drink plenty of fluids and be sure to follow up with your doctor if your diarrhea continues or worsens. They can recommend ways to help ease your symptoms or suggest a different treatment option for you.
Loss of liver function in people with chronic hepatitis C
If you have chronic hepatitis C, it’s possible that taking Promacta can cause your liver to work less well.* This is called hepatic decompensation. It can result in ascites (fluid buildup in your belly) or encephalopathy, which affects the brain and causes foggy or confused thinking.
In studies of those with chronic hepatitis C, people took peginterferon (PegIntron, Pegasys) and ribavirin (Rebetol) with or without Promacta. About 7% of those who took Promacta had ascites and encephalopathy. This was compared to 4% of those who didn’t take Promacta.
Changes to liver function can be very serious. If you have fluid buildup in your belly or notice changes in your thinking, tell your doctor right away. They’ll likely have you stop your Promacta treatment.
* Promacta has a
Risk of liver damage
It’s not common, but it’s possible that taking Promacta can cause damage to the liver.* In clinical studies, 1% or less of people had liver damage due to medication. Some of these people were taking Promacta with other drugs, so it’s hard to say whether Promacta caused the liver damage.
During your Promacta treatment, your doctor will monitor your liver function by looking at liver enzymes such as ALT and AST. (Enzymes are proteins that aid chemical changes in your body.) Your doctor will also look at your bilirubin level. (Bilirubin is made when blood cells break down.) They’ll check your ALT, AST, and bilirubin levels before you start taking Promacta, every 2 weeks while your dose is being adjusted, and at least monthly after that.
Signs and symptoms of liver problems can include:
- large increases in levels of the liver enzymes ALT and AST
- increased level of bilirubin
- fluid in the belly
- urine that’s darker than usual
- confusion
- tiredness
- yellowing of skin or the white of your eyes
- itchiness
- loss of appetite
- pain in upper stomach area
If you notice any of these signs or symptoms, tell your doctor. They’ll want to check your ALT, AST, and bilirubin levels. If the levels are high, your doctor may recheck you in a few days or have you stop taking Promacta.
* Promacta has a
The Food and Drug Administration (FDA) approves prescription drugs such as Promacta to treat certain conditions. Promacta may also be used off-label for other conditions. Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.
Promacta for ITP
Promacta is FDA-approved for the treatment of thrombocytopenia (low platelet count) in adults as well as children ages 1 year and older who have chronic immune thrombocytopenia (ITP). You must have already tried treatments that didn’t work.Examples of these treatments include immunoglobulins (injections of proteins), corticosteroids, and splenectomy (the removal of your spleen). Even when other treatment options have failed, you should take Promacta only if you have an increased risk for bleeding.
With chronic ITP, blood doesn’t clot as expected. It’s an autoimmune condition in which the body’s immune system mistakenly works against itself. People with chronic ITP don’t have enough platelets. (Another name for platelets is thrombocytes.) Platelets help form blood clots when they’re needed, such as when your skin is cut.
People without enough platelets are more likely to have bleeding issues. Examples of these issues include:
- bruising that you can see on the skin
- nosebleeds
- menstrual bleeding that’s heavier than usual
- other external or internal bleeding that isn’t expected in people who don’t have chronic ITP
Chronic ITP lasts at least 6 months, while acute ITP has a shorter time frame.
Effectiveness
Clinical studies of adults with chronic ITP compared Promacta with a placebo (treatment with no active drug). The success of treatment was based on desired platelet count increases (amount your platelets should increase while taking the medication) at any point during treatment. Desired platelet count increases were found in 59% to 70% of adults who took Promacta compared with 11% to 16% of those who took a placebo.
Promacta for thrombocytopenia in people with chronic hepatitis C
Promacta is approved by the FDA for the treatment of thrombocytopenia in people with chronic hepatitis C who need to start taking a medication called interferon for their condition. These people can’t take interferon due to their thrombocytopenia. Promacta helps treat their thrombocytopenia, so they can start and keep taking interferon.
Chronic hepatitis C is an infection caused by a virus that affects your liver. If you have chronic hepatitis C, it may cause you to develop thrombocytopenia. This drop in the platelet level occurs in people with hepatitis C for several reasons. Examples include possible side effects from treatment medications and a decrease in a hormone called thrombopoietin, which is involved in making platelets.
Thrombocytopenia can cause bleeding issues and prevent you from being able to take the medications you need to treat your hepatitis C. For these reasons, your doctor may prescribe Promacta. The drug may help decrease your bleeding risk and allow you take the medications you need for hepatitis C.
Effectiveness
In clinical studies of adults with chronic hepatitis C and thrombocytopenia, people took Promacta or a placebo. They were also taking peginterferon (PegIntron, Pegasys) and ribavirin (Rebetol) medications for their condition.
Success was defined as a sustained virologic response (SVR) after treatment. This is when the hepatitis virus can no longer be found in a person’s blood. SVR rates for people who took Promacta ranged from 19% to 23% compared with 13% to 14% for people who took a placebo. Most (76%) of people who took Promacta met goal platelet counts compared with 19% of those who took a placebo. Goal platelet counts are the platelet levels that the doctor wanted the person to reach.
Promacta for severe aplastic anemia with immunosuppressive therapy
Promacta is FDA-approved for the treatment of severe aplastic anemia (SAA) in adults as well as children ages 2 years and older. The drug is to be used with immunosuppressive therapy, which is a kind of treatment that decreases the activity of your immune system. Immunosuppressive treatment may include horse antithymocyte globulin (h-ATG) and cyclosporine (Neoral, Sandimmune).
Aplastic anemia causes a decrease in the levels of red blood cells, white blood cells, and platelets. This occurs when the stem cells in bone marrow have been harmed. The damage may be due to:
- having an autoimmune condition, in which your immune system works against itself
- taking certain medications, such as chemotherapy
- having been exposed to certain chemicals in the environment, such as benzene, pesticides, or insecticides
Taking Promacta along with immunosuppressive treatment may help improve your platelet counts and decrease the risk of bleeding.
Effectiveness
Clinical studies looked at adults as well as children ages 2 and older with SAA. They took Promacta in addition to h-ATG and cyclosporine. Success was considered having a complete response in the levels of cells called neutrophils, platelets, and hemoglobin. A complete response meant that the blood counts met the goals the doctor set. A complete response occurred in 44% of people in the studies. Promacta wasn’t compared with a different treatment or a placebo.
Promacta for severe aplastic anemia that’s refractory
Promacta is FDA-approved for the treatment of SAA that’s refractory. Refractory means the condition hasn’t been helped by previous treatment. In this case, the previous treatment was immunosuppressive therapy.
For details on aplastic anemia, please see the section “Promacta for severe aplastic anemia with immunosuppressive therapy” above.
Effectiveness
A clinical study looked at adults ages 17 to 77 years with SAA. They had previously tried immunosuppressive therapy, but the treatment didn’t fully work. Researchers looked at how people’s bodies responded to Promacta after 12 weeks of treatment. The response was based on:
- certain goals for platelet count
- hemoglobin level
- a decreased need for red blood cell transfusions
- absolute neutrophil count (the number of neutrophils, which are a kind of white blood cell)
In the study, 40% of the people responded to Promacta, meaning that the drug worked for them. Promacta wasn’t compared with a different drug or a placebo.
Promacta for other conditions
In addition to the uses listed above, you may wonder if Promacta is used for certain other conditions. Here we describe a condition that Promacta isn’t used to treat.
Promacta for MDS (not an approved use)
Promacta isn’t approved for the treatment of myelodysplastic syndrome (MDS), which includes certain cancers of the blood and bone marrow. Taking Promacta for MDS may increase the risk of MDS becoming acute myelogenous leukemia (AML).
A study looked at people with MDS who took azacitidine (Vidaza) with either Promacta or a placebo. Researchers studied how often MDS became AML. In the Promacta group, MDS became AML in 12% of the people. This was compared with 6% of people in the placebo group.
Studies such as
Promacta and children
Promacta is FDA-approved to treat:
- thrombocytopenia in children ages 1 year and older who have chronic immune thrombocytopenia (ITP)
- severe aplastic anemia (SAA) in children ages 2 years and older. Promacta is to be used with immunosuppressive therapy, which is a kind of treatment that decreases the activity of the immune system.
The drug has been shown to be safe and effective in these children.
A clinical study looked children ages 1 year and older with chronic ITP who took Promacta or a placebo. Treatment was considered to be successful based on having a certain platelet count for at least 6 out of 8 weeks. About 40% of children who took Promacta reached this platelet goal compared with 3% of those who took a placebo.
Promacta is often used with other medications. How it’s used with other medications depends on the conditions you have. In some cases, taking Promacta lets you be able to use important medications for another condition, such as chronic hepatitis C.
Sometimes Promacta is used as an add-on medication to manage thrombocytopenia in people with severe aplastic anemia (SAA). The drug is used with immunosuppressive therapy, which is a kind of treatment that decreases the activity of your immune system.
For a condition called chronic immune thrombocytopenia (ITP), Promacta is used after other treatments have failed. These treatments include immunoglobulins (injections of proteins), corticosteroids, and splenectomy (the removal of your spleen).
For more information about how Promacta is used with other medications, see the “Promacta uses” section above.
The Promacta dosage your doctor prescribes will depend on several factors. Dosing guidelines vary and depend on the following:
- the type and severity of the condition you’re using Promacta to treat
- your age
- the form of Promacta you take
- other medical conditions you may have
- Asian ancestry
Typically, your doctor will start you on a low dosage. Then they’ll adjust it over time to reach the amount that’s right for you. Your doctor will ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to fit your needs.
Drug forms and strengths
Promacta comes in two forms:
- A tablet that you swallow. It’s available in these strengths: 12.5 mg, 25 mg, 50 mg, and 75 mg.
- A packet of powder. You’ll mix it with water to create a suspension (liquid) that’s to be used with an oral syringe. The packet is available in these strengths: 12.5 mg and 25 mg.
Dosage for ITP
The dosage for chronic immune thrombocytopenia (ITP) will typically be 50 mg once a day.If you’re of Asian ancestry (such as Chinese, Japanese, Taiwanese, or Korean), your starting dosage will usually be 25 mg once a day.
If you have liver problems, your doctor may recommend a dosage of Promacta that’s different than the typical dosage. Talk with your doctor to see what’s right for you.
Your doctor will adjust your Promacta dosage for you to reach a goal platelet count to reduce the risk for bleeding. During your treatment, they’ll give you blood tests often to monitor your progress and adjust your dosage, if necessary.
Dosage for thrombocytopenia in people with chronic hepatitis C
The starting dose for the treatment of thrombocytopenia in people with chronic hepatitis C is 25 mg once a day. Your doctor will usually adjust the dose every 2 weeks to meet platelet count goals that they’ll set. The maximum dose for this condition is 100 mg of Promacta a day.
Your doctor will have you stop taking Promacta when you stop your antiviral treatment for hepatitis C.
Dosage for severe aplastic anemia with immunosuppressive therapy
The recommended dosage of Promacta for the treatment of severe aplastic anemia (SAA) is 150 mg once a day for 6 months. Promacta will be used with immunosuppressive therapy, which is a kind of treatment that decreases the activity of your immune system. If you’re of Asian ancestry (such as Chinese, Japanese, Taiwanese, or Korean), your starting dosage will usually be 75 mg a day for 6 months.
If you have liver problems, your doctor may recommend a dosage of Promacta that’s different than the typical dosage. Talk with your doctor to see what’s right for you.
You shouldn’t take more than the dosage that your doctor recommends. They’ll decrease or pause your dosage based on your platelet counts. And to make these changes, your doctor will need to monitor you closely.
Dosage for severe aplastic anemia that’s refractory
The usual starting dosage for SAA that’s refractory (hasn’t gotten better with other treatment) is 50 mg a day. If you’re of Asian ancestry (such as Chinese, Japanese, Taiwanese, or Korean), your starting dose will be 25 mg a day.
Your doctor will typically adjust the dosage every 2 weeks based on your platelet count. The maximum recommended dosage for this condition is 150 mg once a day. If Promacta doesn’t seem to be helping you after 16 weeks, your doctor will likely have you stop the treatment.
If you have liver problems, your doctor may recommend a dosage of Promacta that’s different than the typical dosage. Talk with your doctor to see what’s right for you.
Pediatric dosage
Promacta is approved to be used in children with chronic ITP and SAA.
ITP
Here are the typical recommended starting dosages of Promacta for children:
- ages 6 years and older: 50 mg once a day. If your child is of Asian ancestry (such as Chinese, Japanese, Taiwanese, or Korean), their starting dosage will usually be 25 mg once a day.
- ages 1 year to 5 years: 25 mg once a day
Your child’s doctor will adjust the Promacta dosage for your child to reach a goal platelet count to reduce the risk for bleeding. During your child’s treatment, the doctor will give them blood tests often to monitor their progress and adjust their dosage, if necessary.
If your child has liver problems, their doctor may recommend a dosage of Promacta that’s different than the typical dosage. Talk with your child’s doctor to learn more.
Severe aplastic anemia with immunosuppressive therapy
Here are the recommended dosages of Promacta for children:
- ages 12 years and older: 150 mg once a day for 6 months. If your child is of Asian ancestry (such as Chinese, Japanese, Taiwanese, or Korean), their starting dose will usually be 75 mg a day for 6 months.
- ages 6 years to 11 years: 75 mg once a day for 6 months. If your child is of Asian ancestry (such as Chinese, Japanese, Taiwanese, or Korean), their starting dose will usually be 37.5 mg a day for 6 months.
- ages 2 years to 5 years: 2.5 mg/kg once a day for 6 months. Your child’s doctor will determine how much Promacta your child will take based on their weight. If your child is of Asian ancestry (such as Chinese, Japanese, Taiwanese, or Korean), their starting dose will usually be 1.25 mg/kg a day for 6 months.
Promacta will be used with immunosuppressive therapy, which is a kind of treatment that decreases the activity of your child’s immune system.
You shouldn’t give your child more than the dosage that their doctor recommends. The doctor will decrease or pause the dosage based on your child’s platelet counts. And to make these changes, your child’s doctor will need to monitor them closely.
If your child has liver problems, their doctor may recommend a dosage of Promacta that’s different than the typical dosage. Talk with your child’s doctor to learn more.
What if I miss a dose?
If you miss a dose of Promacta, take it as soon as you remember unless it’s close to your next dose. Don’t take more than one Promacta dose in 24 hours.
To help make sure that you don’t miss a dose, try setting a reminder on your phone. A medication timer may be useful, too.
Will I need to use this drug long term?
Promacta is meant to be used as a long-term treatment. If you and your doctor determine that Promacta is safe and effective for you, you’ll likely take it long term. The length of time you take the medication will depend on the condition being treated as well as how your body responds to the medication.
Promacta is used to treat thrombocytopenia, which is a low platelet count that can lead to bleeding. Platelets are the parts of your blood that help it clot. So if you have fewer platelets, you’re more likely to bleed.
Thrombocytopenia can be a very serious condition. Treatment is often needed, especially if the condition is severe or chronic (long term). Promacta works by binding to a protein called thrombopoietin receptor. This receptor tells the body to make more platelets, which increases platelet levels. Through this process, Promacta helps prevent bleeding problems.
How long does it take to work?
How long Promacta takes to work depends on the condition the drug is treating.
ITP
In studies of people with chronic immune thrombocytopenia (ITP) who took Promacta for thrombocytopenia, platelet counts generally increased within 1 to 2 weeks of treatment.
Thrombocytopenia in people with chronic hepatitis C
In studies of people with chronic hepatitis C who took Promacta for thrombocytopenia, platelet counts usually started to increase within 1 week of starting to take the drug.
Severe aplastic anemia with immunosuppressive therapy
It’s not known how soon Promacta starts to work in people with severe aplastic anemia (SAA) who also used immunosuppressive therapy. (This is a kind of treatment that decreases the activity of your immune system.)
Severe aplastic anemia
For people with severe aplastic anemia that hasn’t been helped by immunosuppressive therapy, it may take up to 16 weeks of Promacta use for the medication to increase blood counts. This is according to studies. The 16-week time frame includes dosage adjustments.
You should take Promacta according to your doctor’s or healthcare provider’s instructions.
Promacta comes in two forms. One is a tablet that you swallow. The other is a packet of powder that you’ll mix with water to create a suspension (liquid). The suspension is to be used with an oral syringe.
If your doctor prescribes the suspension form of Promacta, your doctor or pharmacist can show you how to prepare the doses. Keep in mind that you shouldn’t use hot water to mix the powder. Also, it’s important to take the dose within 30 minutes of preparing it. After that, you should dispose of the suspension.
When to take
You’ll take Promacta once a day on an empty stomach (1 hour before or 2 hours after a meal).
It’s also important to take Promacta at least 2 hours before or 4 hours after consuming:
- foods or drinks that contain a lot of calcium, such as milk, yogurt, cottage cheese, and fortified juice
- medications, such as antacids, that contain calcium or magnesium
- supplements that contain iron, calcium, aluminum, magnesium, selenium, or zinc, including some multivitamins
If you’re not sure what your supplement contains, look at the ingredients or ask your pharmacist or doctor.
To help make sure that you don’t miss a dose of Promacta, try setting a reminder on your phone. A medication timer may be useful, too.
Taking Promacta with food
You shouldn’t take Promacta with food. Instead, take your dose at least 1 hour before or 2 hours after a meal.
It’s also important to take Promacta at least 2 hours before or 4 hours after consuming foods and drinks that contain with a lot of calcium. These can include milk, yogurt, cottage cheese, and fortified juice.
If you’re not sure whether your foods or drinks are high in calcium, ask your pharmacist or doctor.
Can Promacta be crushed, split, or chewed?
No, you shouldn’t crush, split, or chew Promacta tablets or mix them with food or liquid. Swallow Promacta tablets whole.
No direct interactions between Promacta and alcohol have been found. However, alcohol can cause or worsen liver problems. And Promacta is known to cause liver problems in people with a liver infection called chronic hepatitis C.* So drinking alcohol with Promacta could make liver damage more likely.
If you have concerns about your alcohol use or wonder if it’s safe to drink while taking Promacta, talk with your doctor.
* Promacta has a
Promacta can interact with several other medications. It can also interact with certain supplements as well as certain foods.
Different interactions can cause different effects. For instance, some interactions can interfere with how well a drug works. Other interactions can increase the number of side effects or make them more severe.
Promacta and other medications
Below is a list of medications that can interact with Promacta. This list doesn’t contain all drugs that may interact with Promacta.
Before taking Promacta, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Promacta and antacids containing calcium or magnesium
Taking over-the-counter antacids containing calcium or magnesium too close to your Promacta dose can prevent you from absorbing Promacta. So you should take Promacta at least 2 hours before or 4 hours after using an antacid. This helps prevent the level of Promacta in your body from becoming lower.
If you’re not sure whether your antacid contains calcium or magnesium, check the ingredients. You can also ask your pharmacist or doctor.
Promacta and certain cholesterol medications
Promacta may raise the levels of certain cholesterol medications. And higher levels of the cholesterol drugs may increase the risk of side effects from them.
Examples of these cholesterol medications include:
- atorvastatin (Lipitor)
- ezetimibe (Zetia)
- fluvastatin (Lescol XL)
- pitavastatin (Livalo)
- pravastatin (Pravachol)
- rosuvastatin (Crestor)
- simvastatin (Zocor)
If you’re taking a cholesterol drug, tell your doctor before using Promacta. They may recommend other treatments for you.
Promacta and certain blood pressure medications
Promacta may raise the levels of certain blood pressure drugs. And higher levels of the medications may increase the risk of side effects from them.
Promacta is known to interact with these blood pressure medications:
- bosentan (Tracleer)
- olmesartan (Benicar)
- valsartan (Diovan)
If you’re taking any blood pressure medications, talk with your doctor before using Promacta. They may prescribe other treatments for you.
Promacta and certain diabetes medications
Promacta may raise the levels of certain diabetes medications. And higher levels of the drugs may increase the risk of side effects from them.
Promacta is known to interact with these diabetes medications:
- glyburide (DiaBeta)
- repaglinide
If you’re taking any diabetes medications, talk with your doctor before you use Promacta. They may recommend other treatments for you.
Promacta and rifampin
Promacta may raise the level of an antibiotic called rifampin (Rifadin). A higher level of rifampin may increase the risk of side effects from the drug. If you’re taking rifampin, tell your doctor before using Promacta. They may recommend a different treatment for you.
Promacta and certain breast cancer treatments
Promacta may raise the levels of certain breast cancer drugs. And higher levels of the medications may increase the risk of side effects from them.
Promacta may interact with the following breast cancer treatments:
- imatinib (Gleevec)
- irinotecan (Camptosar)
- lapatinib (Tykerb)
- methotrexate (Xatmep, Trexall)
- mitoxantrone
- topotecan (Hycamtin)
If you’re taking any breast cancer medications, check with your doctor before using Promacta. They may prescribe other treatments for you.
Promacta and sulfasalazine
Promacta may raise the level of an ulcerative colitis medication called sulfasalazine (Azulfidine). A higher level of sulfasalazine may increase the risk of side effects from the drug. Before you take Promacta, tell your doctor if you’re using sulfasalazine. They may recommend a different treatment for you.
Promacta and herbs and supplements
Supplements that contain certain minerals can interact with Promacta and decrease the level of Promacta in the body. So it’s important to take Promacta at least 2 hours before or 4 hours after taking supplements that contain these minerals.
Minerals that can interact with Promacta include:
Keep in mind that multivitamins often contain some of these minerals. If you have questions about any of the supplements you’re taking, talk with your doctor or pharmacist.
There aren’t any herbs that have been specifically reported to interact with Promacta. However, you should still check with your doctor or pharmacist before using any of these products while taking Promacta.
Promacta and foods
Foods and drinks that are high in calcium can prevent you from absorbing Promacta, which can decrease the level of the drug in your body. (Calcium-rich foods and drinks can include milk, yogurt, cottage cheese,and fortified juice.) So it’s important to take Promacta at least 2 hours before or 4 hours after consuming food or drinks that are high in calcium.
If you have questions about the calcium levels in any of the foods you’re eating, talk with your doctor or pharmacist.
As with all medications, the cost of Promacta can vary. The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
It’s important to note that you’ll have to get Promacta at a specialty pharmacy. This type of pharmacy is authorized to carry specialty medications. These are drugs that may be expensive or may require help from healthcare professionals to be used safely and effectively.
Your insurance plan may require you to get prior authorization before approving coverage for Promacta. This means that your doctor and insurance company will need to communicate about your prescription before the insurance company will cover the drug. The insurance company will review the request and let you and your doctor know if your plan will cover Promacta.
If you’re not sure if you’ll need to get prior authorization for Promacta, contact your insurance company.
Financial and insurance assistance
If you need financial support to pay for Promacta, or if you need help understanding your insurance coverage, help is available.
Novartis Pharmaceuticals Corporation, the manufacturer of Promacta, offers programs called Patient Assistance Now Oncology and Co-pay Assistance 4U. For more information and to find out if you’re eligible for support, call 844-776-6228 or visit the Promacta resources website.
Other drugs are available that can treat your condition. Some may be a better fit for you than others. If you’re interested in finding an alternative to Promacta, talk with your doctor. They can tell you about other medications that may work well for you.
Note: Some of the drugs listed below are used off-label to treat these specific conditions. Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.
Alternatives for thrombocytopenia
Thrombocytopenia can be caused by different conditions. Your doctor will choose the best treatment for your thrombocytopenia based on your condition and medical history.
Examples of other drugs that may be used to treat thrombocytopenia include:
- corticosteroids, such as prednisone or dexamethasone
- rituximab (Rituxan, Truxima)
- immune globulin
- anti-Rh (D) immunoglobulin
- romiplostim (Nplate)
Alternatives for severe aplastic anemia
Your doctor will choose the best treatment for your aplastic anemia based on the severity and causes of your condition as well as your medical history.
Examples of other drugs that may be used to treat severe aplastic anemia (SAA) include:
- antithymocyte globulin (h-ATG, Thymoglobulin)
- cyclosporine (Neoral, Sandimmune)
- cyclophosphamide
- tacrolimus (Prograf)
The medications listed above are forms of immunosuppressive therapy, which is a kind of treatment that decreases the activity of your immune system. In some cases, Promacta may be used in addition to immunosuppressive therapy. If your condition doesn’t improve enough with immunosuppressive therapy, your doctor may recommend that you take Promacta by itself.
You may wonder how Promacta compares with other medications that are prescribed for similar uses. Here we look at how Promacta and dexamethasone are alike and different.
Ingredients
Promacta and dexamethasone don’t contain the same active ingredients, and they belong to different medication classes. (A class of medications is a group of drugs that work in a similar way.)
Promacta contains the active ingredient eltrombopag and belongs to a medication class called thrombopoietin receptor agonists.
Dexamethasone contains the active ingredient dexamethasone and belongs to a medication class known as steroids.
Uses
Both Promacta and dexamethasone have several uses.
Promacta uses
The Food and Drug Administration (FDA) has approved Promacta to treat these conditions:
- Thrombocytopenia (low platelet count) in adults as well as children ages 1 year and older who have chronic immune thrombocytopenia. With chronic immune thrombocytopenia (ITP), low levels of platelets cause bleeding that appears as rashes. To be prescribed Promacta for this condition, you must have already tried treatments that didn’t work. These treatments include immunoglobulins (injections of proteins), corticosteroids, or splenectomy (the removal of your spleen). Even when other treatment options have failed, you should take Promacta only if you have an increased risk for bleeding.
- Thrombocytopenia in adults with chronic hepatitis C who need to start taking a medication called interferon for their condition. (Chronic hepatitis C is a type of liver infection.) You should use Promacta only if you haven’t been able to start taking or keep taking interferon for chronic hepatitis C without Promacta.
- Severe aplastic anemia. With severe aplastic anemia (SAA), the stem cells in your bone marrow become damaged. Promacta is used in two ways to treat SAA:
- It’s used with immunosuppressive therapy in adults as well as children ages 2 years and older. This is a kind of treatment that decreases the activity of your immune system.
- It’s used to treat SAA in adults that’s refractory.A condition is called refractory when it hasn’t been helped by previous treatment. In this case, people with SAA have tried immunosuppressive therapy in the past, but it wasn’t successful.
Promacta shouldn’t be used to treat myelodysplastic syndrome (MDS), a group of cancers of the blood and bone marrow. And it’s not known whether it’s safe and effective to use Promacta to treat chronic hepatitis C with drugs called direct-acting antiviral agents, but without interferon.
Dexamethasone uses
Dexamethasone is used off-label for the treatment of ITP. (Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.)
Dexamethasone is FDA-approved for the treatment of numerous conditions, including:
- allergic reactions
- inflammation
- pretreatment for chemotherapy to ease inflammation and side effects from cancer drugs
- adrenal insufficiency (a condition in which the adrenal glands don’t make enough hormones)
- skin diseases, such as severe erythema multiforme (Stevens-Johnson syndrome), pemphigus, exfoliative dermatitis, severe seborrheic dermatitis, bullous dermatitis herpetiformis, mycosis fungoides, and severe psoriasis
- rheumatoid arthritis and other rheumatic diseases, including ankylosing spondylitis, acute gouty arthritis, psoriatic arthritis, juvenile rheumatoid arthritis, and lupus
- flare-ups of myasthenia gravis and multiple sclerosis
- flare-ups of intestinal disease, such as ulcerative colitis
Drug forms and administration
Promacta comes in two forms. One is a tablet that you swallow. The other is a packet of powder that you’ll mix with water to create a suspension (liquid). The suspension is to be used with an oral syringe.
The forms of dexamethasone that are usually used to treat thrombocytopenia are a tablet or liquid solution that you swallow. You’ll take these forms of dexamethasone once a day. An injectable form is also available that a healthcare provider would need to give you.
Side effects and risks
Promacta and dexamethasone can cause some very similar and some very different side effects. Below are examples of these side effects.
Mild side effects
These lists contain examples of mild side effects that can occur with Promacta, with dexamethasone, or with both drugs (when taken individually).
- Can occur with Promacta:
- fatigue (lack of energy)
- diarrhea
- vomiting
- upper respiratory infection (URI), such as the common cold
- urinary tract infection
- muscle aches
- sore throat
- back pain
- flu
- dry mouth
- changes in skin color (including darker patches or yellowing of skin)
- Can occur with dexamethasone:
- high blood pressure
- decreased or increased heart rate
- dry skin
- increased sweating
- increased blood sugar level
- changes in menstruation, such as an irregular cycle
- hypokalemia (low level of potassium)
- depression
- emotional ups and downs
- trouble sleeping
- weight gain
- swelling or fluid retention
- Can occur with both Promacta and dexamethasone:
- rash
- hair loss
- small increases in the levels of liver enzymes called alanine aminotransferase (ALT) and aspartate aminotransferase (AST), which may be symptoms of liver damage
- tickling, burning, or prickling feeling on the skin
Serious side effects
These lists contain examples of serious side effects that can occur with Promacta, with dexamethasone, or with both drugs (when taken individually).
- Can occur with Promacta:
- hepatotoxicity (harm to the liver)*
- hemorrhage (bleeding)
- severe anemia
- Can occur with dexamethasone:
- abnormal heart rhythms (heartbeat that’s too fast, too slow, or uneven)
- cardiac arrest (your heart stops beating)
- Can occur with both Promacta and dexamethasone:
- thromboembolism (a blood clot in a blood vessel)
- cataracts (an eye problem)
* Promacta has
Effectiveness
The only condition both Promacta and dexamethasone are used to treat is thrombocytopenia.
These drugs haven’t been directly compared in clinical studies, but studies have found both Promacta and dexamethasone to be effective for treating thrombocytopenia.
Promacta may be used after other treatment options haven’t worked well. These options include corticosteroids such as dexamethasone.
Costs
Promacta is a brand-name drug. Dexamethasone is available as a generic drug. Brand-name medications usually cost more than generics.
Promacta tablets cost significantly more than dexamethasone tablets. The actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
You may wonder how Promacta compares with other medications that are prescribed for similar uses. Here we look at how Promacta and Thymoglobulin are alike and different.
Ingredients
Promacta and Thymoglobulin don’t contain the same active ingredients, and they belong to different medication classes. (A class of medications is a group of drugs that work in a similar way.)
Promacta contains the active ingredient eltrombopag and belongs to a medication class called thrombopoietin receptor agonists.
Thymoglobulin contains the active ingredient antithymocyte globulin and belongs to the immunoglobulin G medication class.
Uses
Here’s some information about the uses of Promacta and Thymoglobulin.
Promacta uses
The Food and Drug Administration (FDA) has approved Promacta to treat these conditions:
- Thrombocytopenia (low platelet count) in adults as well as children ages 1 year and older who have chronic immune thrombocytopenia. With chronic immune thrombocytopenia (ITP), low levels of platelets cause bleeding that appears as rashes. To be prescribed Promacta for this condition, you must have already tried treatments that didn’t work. These treatments include immunoglobulins (injections of proteins), corticosteroids, or splenectomy (the removal of your spleen). Even when other treatment options have failed, you should take Promacta only if you have an increased risk for bleeding.
- Thrombocytopenia in adults with chronic hepatitis C who need to start taking a medication called interferon for their condition. (Chronic hepatitis C is a type of liver infection.) You should use Promacta only if you haven’t been able to start taking or keep taking interferon for chronic hepatitis C without Promacta.
- Severe aplastic anemia. With severe aplastic anemia (SAA), the stem cells in your bone marrow become damaged. Promacta is used in two ways to treat SAA:
- It’s used with immunosuppressive therapy in adults as well as children ages 2 years and older. This is a kind of treatment that decreases the activity of your immune system.
- It’s used to treat SAA in adults that’s refractory.A condition is called refractory when it hasn’t been helped by previous treatment. In this case, people with SAA have tried immunosuppressive therapy in the past, but it wasn’t successful.
Promacta shouldn’t be used to treat myelodysplastic syndrome (MDS), a group of cancers of the blood and bone marrow. And it’s not known whether it’s safe and effective to use Promacta to treat chronic hepatitis C with drugs called direct-acting antiviral agents, but without interferon.
Thymoglobulin uses
Thymoglobulin is used off-label for the treatment of SAA. (Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.)
Thymoglobulin is FDA-approved to help prevent and treat transplant rejection in people who are receiving a kidney transplant. The drug is meant to be used with other immunosuppressive treatments.
Drug forms and administration
Promacta comes in two forms. One is a tablet that you swallow. The other is a packet of powder that you’ll mix with water to create a suspension (liquid). The suspension is to be used with an oral syringe.
Thymoglobulin comes as an infusion, which is an injection into your vein that’s slowly dripped in over time. The drug is given by a healthcare professional.
Side effects and risks
Promacta and Thymoglobulin can cause some very similar and some very different side effects. Below are examples of these side effects.
Mild side effects
These lists contain examples of mild side effects that can occur with Promacta, with Thymoglobulin, or with both drugs (when taken individually).
- Can occur with Promacta:
- fatigue (lack of energy)
- small increases in the levels of liver enzymes called alanine aminotransferase (ALT) and aspartate aminotransferase (AST), which may be symptoms of liver damage
- sore throat
- flu
- tickling, burning, or prickling feeling on the skin
- hair loss
- dry mouth
- changes in skin color (including darker patches or yellowing of skin)
- Can occur with Thymoglobulin:
- belly pain
- shortness of breath
- chills
- increased levels of potassium (can be serious if untreated or severe)
- low levels of platelets or white blood cells (can be serious if severe or untreated)
- infusion reactions (pain, swelling, or redness where the infusion was injected)
- swelling
- Can occur with both Promacta and Thymoglobulin:
- mild anemia (low count of red blood cells or unhealthy red blood cells)
- vomiting
- upper respiratory infection (URI), such as the common cold
- muscle aches
- rash
Serious side effects
These lists contain examples of serious side effects that can occur with Promacta, with Thymoglobulin, or with both drugs (when taken individually).
- Can occur with Promacta:
- hepatotoxicity (harm to the liver)*
- cataracts (an eye problem)
- hemorrhage (bleeding)
- thromboembolism (a blood clot in a blood vessel)
- severe anemia
- Can occur with Thymoglobulin:
- cancers, such as kidney cancer and certain lymphomas
- decreased ability of immune system to fight serious infections
- severe infusion reactions that cause heart or breathing problems
- high levels of lipids (fat) in the blood
- Can occur with both Promacta and Thymoglobulin:
* Promacta has
Effectiveness
Promacta and Thymoglobulin have different FDA-approved uses, but they’re both used to treat SAA.
These drugs haven’t been directly compared in clinical studies, but studies have found both Promacta and Thymoglobulin to be effective for treating aplastic anemia.
Promacta is often used with immunosuppressive therapy, which is a kind of treatment that decreases the activity of your immune system. This therapy includes Thymoglobulin. Promacta may also be used after other treatment options, such as Thymoglobulin and cyclosporine, have failed.
Costs
Promacta and Thymoglobulin are both brand-name drugs. There are currently no generic forms of either drug. Brand-name medications usually cost more than generics.
Your cost for either drug may depend on the condition you’re using it to treat and your dosage. The actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
It’s not known whether Promacta is safe to use during pregnancy. Animal studies have shown that there’s possible harm to babies when the drug is given to pregnant mothers during pregnancy. Butanimal studies don’t always predict what will occur in humans.
If you’re pregnant or thinking about becoming pregnant, talk with your doctor. They can talk with you about the right treatment options for your condition.
It’s not known whether Promacta is safe to take during pregnancy. If you’re sexually active and you or your partner can become pregnant, talk with your doctor about your birth control needs while you’re using Promacta.
It’s recommended that you and your partner use effective birth control while either of you are taking Promacta and for at least 7 days after stopping treatment. (“Effective” means that the birth control has a pregnancy rate of less than 1%.)
It’s recommended that you avoid taking Promacta while breastfeeding. This is due to possible medication side effects in breastfed children. Animal studies have shown that the drug can pass into the breast milk of animals. But animal studies don’t always predict what will occur in humans.
If you’re breastfeeding, talk with your doctor. They can suggest treatment options other than Promacta for your condition.
Here are answers to some frequently asked questions about Promacta.
Is Promacta a chemotherapy drug?
No, chemotherapy usually refers to medications that are used to treat cancer directly. So in this case, Promacta isn’t chemotherapy.
However, Promacta is often used in people having chemotherapy for the treatment of cancer. Common side effects of certain cancers and cancer treatments include anemia and thrombocytopenia, and Promacta helps treat these conditions. Anemia is a low level of red blood cells, and thrombocytopenia is a low level of platelets (parts of your blood that help it clot).
If you have questions about Promacta, chemotherapy, or other cancer-related treatments, talk with your doctor.
Can Promacta cure my condition?
It depends. Promacta is used to treat chronic immune thrombocytopenia (ITP), thrombocytopenia in people with chronic hepatitis C, and severe aplastic anemia (SAA). These conditions are often related to the activity of your immune system (your body’s defense against infection) or hepatitis C, which is a chronic (long-term) condition. This means that your need for treatment, including Promacta, may vary. You may have times when your platelet counts or red blood cell counts rise to healthy levels, and you can stop taking Promacta.
If you have questions about what to expect with Promacta treatment, talk with your doctor. Your treatment plan can depend on other conditions you have, your medical history, and other treatments you’re using.
Why do I have to tell my doctor if I’m Asian before I can use Promacta?
If you’re of Asian ancestry (such as Chinese, Japanese, Taiwanese, or Korean), you’ll likely need a dose of Promacta that’s lower than the typical dose. Studies have shown that people of Asian descent are more sensitive to the drug, so it stays at higher levels in their system. This could result in a greater risk of side effects. (For more about side effects, see the “Promacta side effects” section above.)
Before you take Promacta, be sure to tell your doctor your heritage so they can safely adjust your dose, if needed.
How will my doctor monitor my condition to see if Promacta is working?
Your doctor will give you blood tests throughout your Promacta treatment to see how the drug is working for you. The type of blood test depends on the condition your doctor is treating. So the blood tests may include checks of your platelet or red blood cell counts, and the hepatitis C virus. How often and when you have the tests depend on when you started taking Promacta, other blood test results, and possibly other medications you’re using.
If you’re wondering about any tests while taking Promacta, ask your doctor.
Should I avoid foods and drinks that are high in calcium while I’m taking Promacta?
You may not have to completely avoid food and drinks that are high in calcium, but you shouldn’t consume them when you take a dose of Promacta. You should take the drug at least 2 hours before and 4 hours after consuming high-calcium foods or drinks. Otherwise, they can decrease the level of Promacta that your body can absorb. And this might make the medication less effective.
If you’re wondering which foods and drinks are high in calcium, check with your doctor.
This drug comes with several precautions.
FDA warnings
This drug has
- Liver problems in people with chronic hepatitis C. If you have a liver infection called chronic hepatitis C, taking Promacta with the medications interferon and ribavirin may increase your risk for liver problems. These include ascites, which is a buildup of fluid in your belly, and encephalopathy, a brain condition.
- Liver damage. Promacta can be dangerous to the liver, and taking the drug may increase your risk for serious or life threatening liver damage. Your doctor will closely monitor your liver during your treatment and may have you stop taking the drug, if needed.
Other precautions
Before taking Promacta, talk with your doctor about your health history. Promacta may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Pregnancy. It’s not known whether it’s safe to take Promacta during pregnancy. For more information, please see the “Promacta and pregnancy” section above.
- Breastfeeding. It’s recommended that you avoid taking Promacta while breastfeeding. For more information, please see the “Promacta and breastfeeding” section above.
- Blood clots. Although Promacta can lead to clotting issues and serious blood clots in people who take the medication, certain people may be more likely to develop a clot. So if you’ve had blood clots in the past, have chronic liver disease, or have a blood clotting condition such as Factor V Leiden or an antithrombin III (AT-III) deficiency, tell your doctor. They may choose to monitor you more closely or recommend other treatment options.
- Liver disease. Taking Promacta can increase your risk for liver problems, including a rise in the level of liver enzymes, ascites (fluid in the belly) and encephalopathy (brain condition). If you have or have had liver problems in the past, tell your doctor. This includes hepatitis. Taking certain medications for hepatitis with Promacta can also increase your risk for liver side effects. Your doctor may choose to monitor you more closely or recommend other treatment options for you.
- Myelodysplastic syndrome. Promacta isn’t approved for the treatment of myelodysplastic syndrome (MDS), which includes certain cancers of the blood and bone marrow. For more information, see “Promacta for MDS (not an approved use)” in the “Promacta uses” section above.
- Cataracts. Taking Promacta may lead you to have new or worsening cataracts (an eye problem). Tell your doctor if you have eye issues, including cataracts, before you take Promacta. Your doctor will likely give you eye exams before you start using Promacta and throughout your treatment.
Note: For more information about the potential negative effects of Promacta, see the “Promacta side effects” section above.
Using more than the recommended dosage of Promacta can lead to serious side effects.
Don’t use more Promacta than your doctor recommends. You shouldn’t take more than one dose of Promacta in 24 hours.
Overdose symptoms
Symptoms of an overdose can include:
- large increases in the level of platelets (blood cells that help your blood clot), leading to serious and potentially life threatening blood clots
- rash
- decreased heart rate
- increases in the levels of liver enzymes, which may be a sign of liver damage
- fatigue (lack of energy)
What to do in case of overdose
If you think you’ve taken too much of this drug, call your doctor. You can also call the American Association of Poison Control Centers at 800-222-1222 or use their online tool. But if your symptoms are severe, call 911 or go to the nearest emergency room right away.
When you get Promacta from the pharmacy, the pharmacist will add an expiration date to the label on the bottle. This date is typically 1 year from the date they dispensed the medication.
The expiration date helps guarantee that the medication is effective during this time. The
Storage
How long a medication remains good can depend on many factors, including how and where you store the medication.
You should store Promacta tablets at room temperature between 68°F to 77°F (20°C to 25°C). If needed, you can keep the medication between 59°F to 86°F (15°C to 30°C) for a short time. Store Promacta in a tightly sealed container away from light. Avoid keeping this medication in areas where it could get damp or wet, such as in bathrooms.
Disposal
If you no longer need to take Promacta and have leftover medication, it’s important to dispose of it safely. This helps prevent others, including children and pets, from taking the drug by accident. It also helps keep the drug from harming the environment.
The
The following information is provided for clinicians and other healthcare professionals.
Indications
The Food and Drug Administration (FDA) has approved Promacta to treat the following conditions:
- Thrombocytopenia in adults as well as children ages 1 year and older with chronic immune thrombocytopenia (ITP) who have not been helped by other treatment options. Even when other treatment options have failed, Promacta should only be used for people who have an increased risk for bleeding.
- Thrombocytopenia in people with chronic hepatitis C who need to start interferon medication for their condition. Promacta should be used only for people who have not been able to start or continue interferon use for hepatitis C without Promacta.
- Severe aplastic anemia (SAA) in adults as well as children ages 2 years and older, in addition to standard immunosuppressive treatment.
- Severe aplastic anemia in people who have not been helped by immunosuppressive therapy.
Promacta shouldn’t be used to treat myelodysplastic syndrome (MDS), which includes certain cancers of the blood and bone marrow. And it’s not known whether Promacta is safe and effective to use with direct-acting antiviral agents if interferon is not also used to treat chronic hepatitis C.
For more specific information about a particular indication, please see the “Promacta uses” section, which also includes a discussion about the effectiveness of Promacta for each condition.
Mechanism of action
Promacta works as a thrombopoietin receptor agonist, prompting an increased production of platelets (thrombocytes).
Pharmacokinetics and metabolism
The absorption of Promacta is significantly impacted by ingestion of medications, foods, and supplements containing calcium, magnesium, aluminum, iron, selenium, and zinc. It is important to remind your patients to avoid supplements, antacids, and foods containing high concentrations of these minerals. Taking these will dramatically decrease the level of Promacta available for absorption. Patients should be counseled to take Promacta at least 2 hours before or 4 hours after taking anything in these categories.
Steady-state concentrations of Promacta are reached within about 1 week. This doesn’t necessarily equate to when the impact on platelet counts would be observed. For information about expected response times, see “How long does it take to work?” in the “How Promacta works”section.
Contraindications
There are no specific contraindications provided for Promacta. For additional information about considerations for Promacta prescribing and dosing, see the “FDA warnings” and “Promacta precautions” sections.
Storage
Promacta should be dispensed in the original bottle and stored at room temperature between 68°F to 77°F (20°C to 25°C). Variations in temperature are allowed between 59°F to 86°F (15°C to 30°C).
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.