Xultophy 100/3.6 is a brand-name prescription medication. It’s approved to lower blood sugar levels in adults with type 2 diabetes when used in combination with a healthy diet and exercise.
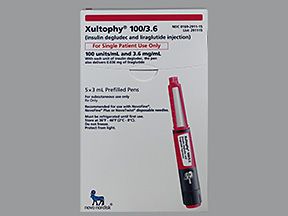
Xultophy 100/3.6 comes as a liquid solution in a prefilled pen. It’s injected under your skin (called a subcutaneous injection) once each day.
Xultophy 100/3.6 pens hold 3 mL of solution that contains these active drugs:
- Insulin degludec. Xultophy 100/3.6 contains 100 units of this form of insulin in each milliliter (mL) of solution. Insulin degludec is a long-acting insulin that’s very similar to the insulin made naturally by your body.
- Liraglutide. Xultophy 100/3.6 contains 3.6 milligrams (mg) of this drug in each mL of solution. Liraglutide belongs to a class of medications called glucagon-like peptide 1 (GLP-1) receptor agonists. It works with insulin to help lower your blood sugar.
Effectiveness
Xultophy 100/3.6 has been found effective in improving blood sugar levels in people with type 2 diabetes who weren’t able to improve their blood sugar levels enough with other diabetes drugs.
A person’s response to diabetes treatment is often measured by testing hemoglobin A1c (HbA1c). This measurement shows your average blood sugar levels over the past two to three months. The American Diabetes Association recommends a HbA1c goal of less than 7.0% for most adults.
In several clinical studies, people took either Xultophy 100/3.6 or comparison drugs, in combination with diabetes medications taken by mouth. After 26 weeks, people had a decrease in their HbA1c of:
- 1.67% to 1.94% with Xultophy 100/3.6, compared to 1.05% to 1.16% with long-acting insulins
- 1.31% with Xultophy 100/3.6, compared to 0.36% with liraglutide
- 1.81% with Xultophy 100/3.6, compared to 1.35% with insulin degludec and 1.21% with liraglutide
- 1.42% with Xultophy 100/3.6, compared to 0.62% with placebo
- 1.97% with Xultophy 100/3.6, compared to 1.59% with insulin glargine
Xultophy 100/3.6 is available only as a brand-name medication. It’s not currently available in generic form.
Xultophy 100/3.6 contains two active drug ingredients: insulin degludec and liraglutide. Both of these drugs are also available in different strengths as separate brand-name drugs. Insulin degludec is available as Tresiba, and liraglutide is available as Victoza.
The Xultophy 100/3.6 dosage your doctor prescribes will depend on several factors. These include:
- the severity of your type 2 diabetes
- whether you have taken either of the drugs contained in Xultophy 100/3.6 (either long-acting insulin or liraglutide) in the past
- other medical conditions you may have
If you’re currently taking any medications that have the same drug ingredients found in Xultophy 100/3.6 (either insulin or liraglutide), you may need to stop using those medications before starting Xultophy 100/3.6. Your doctor will recommend whether you need to do this or not.
Typically, your doctor will start you on a low dosage of Xultophy 100/3.6. Then they’ll adjust your dose over time to reach the amount that’s right for you. Your doctor will ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to suit your needs.
Drug forms and strengths
Xultophy 100/3.6 comes as a liquid solution in a prefilled pen. It’s injected under your skin (called a subcutaneous injection) once each day.
Xultophy 100/3.6 pens hold 3 mL of solution that contains these active drugs:
- Insulin degludec. Xultophy 100/3.6 contains 100 units of this form of insulin in each mL of solution.
- Liraglutide. Xultophy 100/3.6 contains 3.6 mg of this drug in each mL of solution.
Each Xultophy 100/3.6 pen should only be used by one person. You shouldn’t share your Xultophy 100/3.6 pen with other people who are using the drug, even if you use a new needle. Sharing your Xultophy 100/3.6 pen or needles with other people can spread infections.
Dosage for type 2 diabetes
The typical dosage for Xultophy 100/3.6 for type 2 diabetes is as follows:
- If you’ve never taken either drug ingredient contained in Xultophy 100/3.6 (either long-acting insulin or liraglutide), your starting dosage may be 10 units each day. (This amount of Xultophy 100/3.6 contains 10 units of insulin degludec and 0.36 mg of liraglutide.)
- If you’re currently taking either of the drug ingredients contained in Xultophy 100/3.6 (either long-acting insulin or liraglutide), your starting dosage may be 16 units each day. (This amount of Xultophy 100/3.6 contains 16 units of insulin degludec and 0.58 mg of liraglutide.) Before starting Xultophy 100/3.6, your doctor may have you stop using insulin or liraglutide, if you’re already taking either of them.
The maximum daily dose of Xultophy 100/3.6 is 50 units, which contains 50 units of insulin degludec and 1.8 mg of liraglutide.
What if I miss a dose?
If you miss a dose of Xultophy 100/3.6, it’s best to wait to take the drug until your next scheduled dose. This helps prevent your blood sugar level from becoming too low, which can happen if you take two doses of the drug close to each other.
To help make sure that you don’t miss a dose, try setting a reminder on your phone. A medication timer may be useful, too.
Will I need to use this drug long term?
Xultophy 100/3.6 is meant to be used as a long-term treatment. If you and your doctor determine that Xultophy 100/3.6 is safe and effective for you, you’ll likely take it long term.
Xultophy 100/3.6 can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Xultophy 100/3.6. These lists do not include all possible side effects.
For more information on the possible side effects of Xultophy 100/3.6, talk with your doctor or pharmacist. They can give you tips on how to deal with any side effects that may be bothersome.
More common side effects
The more common side effects of Xultophy 100/3.6 can include:
- hypoglycemia (low blood sugar)
- infections, such as a cold
- headache
- nausea
- diarrhea
Most of these side effects may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk with your doctor or pharmacist.
Serious side effects
Serious side effects from Xultophy 100/3.6 aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include the following:
- Pancreatitis (inflammation in your pancreas). Symptoms can include:
- severe pain in the middle part of your upper belly
- vomiting
- Kidney damage or failure. Symptoms can include:
- nausea or vomiting
- feeling very tired or weak
- swelling in your legs, ankles, or feet
- confusion
- trouble breathing
- Gallbladder damage. Symptoms can include:
- belly pain (usually in the middle part of your upper belly)
- nausea or vomiting
- yellowing of the whites of your eyes or your skin
- fever
- Hypokalemia (low potassium level). Symptoms can include:
- muscle cramps or spasms (sudden muscle contractions)
- muscle aches or stiffness
- feeling extremely tired or weak
- fast or irregular heartbeat
- tingling or numbness in your arms, hands, legs, or feet
Other serious side effects, which are discussed in detail below, include the following:
- Severe hypoglycemia (very low blood sugar level)
- Severe allergic reaction
- Possible risk of thyroid cancer*
* Xultophy 100/3.6 has a
Side effect details
You may wonder how often certain side effects occur with this drug, or whether certain side effects pertain to it. Here’s some detail on several of the side effects this drug may or may not cause.
Allergic reaction
Some people have reported having severe allergic reactions while taking Xultophy 100/3.6, However, there aren’t any clinical studies that show for sure if Xultophy 100/3.6 causes allergic reactions. And it’s not known how often allergic reactions happen in people using this drug.
Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (warmth and redness in your skin)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
Call your doctor right away if you have a severe allergic reaction to Xultophy 100/3.6. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency.
Thyroid cancer
This drug has a boxed warning for thyroid tumors and a type of thyroid cancer called medullary thyroid carcinoma (MTC). Boxed warnings are the most serious type of warning given by the FDA.
Liraglutide, one of the active ingredients in Xultophy 100/3.6, has been shown to increase the risk of thyroid tumors in animals. However, it’s not known whether Xultophy 100/3.6 will cause thyroid tumors in humans.
In animal studies, liraglutide caused thyroid tumors and cancer in rats and mice. While animal studies don’t predict what will happen in humans, MTC has been reported in some people after taking liraglutide. However, it’s not known for sure if liraglutide caused the thyroid cancer in these people.
In clinical studies, people were given Victoza (a diabetes drug that contains liraglutide). In the study, seven people taking Victoza developed papillary thyroid cancer. This was compared to only one person who developed thyroid cancer while taking metformin with another diabetes drug called rosiglitazone (Avandia).
Your doctor will discuss with you the possible risk of thyroid tumors and cancer while you’re using Xultophy 100/3.6. You should let your doctor know if you have any symptoms of thyroid cancer, which may include:
- having a lump in your neck
- trouble breathing or swallowing
- constantly having a raspy voice
You shouldn’t take Xultophy 100/3.6 if you have multiple endocrine neoplasia syndrome type 2 (MEN 2), which is a condition that causes tumors in your endocrine glands. You should also avoid taking Xultophy 100/3.6 if you or a family member currently has or has had MTC in the past.
If you have concerns about your risk of thyroid cancer while using Xultophy 100/3.6, talk with your doctor. They can discuss the risks and benefits of using this drug to treat type 2 diabetes.
Hypoglycemia
You may develop hypoglycemia (low blood sugar) while you’re using Xultophy 100/3.6. This is the most common side effect of medications that contain insulin, such as Xultophy 100/3.6.
In clinical studies, 14.4% to 37.2% of people had at least one episode of hypoglycemia while taking Xultophy 100/3.6. In these studies, people with a blood sugar level less than 54 mg/dL were considered to have hypoglycemia.
Symptoms of hypoglycemia can include:
- feeling dizzy, lightheaded, weak, or shaky
- feeling drowsy or confused
- difficulty seeing or speaking
- feeling anxious, moody, or irritated
- hunger
- headache
- fast heartbeat
- sweating
If you have episodes of low blood sugar, talk with your doctor. They may recommend that you take a lower dose of Xultophy 100/3.6 or any other diabetes drugs you’re using, or that you monitor your blood sugar levels more often.
Upper respiratory infections
You may have upper respiratory infections, such as the common cold, while you’re using Xultophy 100/3.6. These infections are a common side effect of the drug. In a clinical study, 5.7% of people taking Xultophy 100/3.6 had an upper respiratory infection.
While there isn’t a known cure for colds, you can do certain things to help improve your symptoms, such as:
- drink plenty of water and other fluids (for example, soup)
- rest as much as possible
- eat healthy foods
If your cold lasts longer than 7 to 10 days, or if your symptoms worsen, talk with your doctor or pharmacist. They’ll recommend possible ways to improve your symptoms, and they’ll advise whether you need medical care.
Headache
You may have headaches while you’re taking Xultophy 100/3.6. In a clinical study, 9.1% of people taking Xultophy 100/3.6 got this side effect. Headaches can also be a sign of hypoglycemia (low blood sugar). See the “Hypoglycemia” section above for more details.
If you have headaches while you’re taking Xultophy 100/3.6, talk with your doctor or pharmacist. Let them know if your headaches are severe or if they occur often. Your doctor or pharmacist may be able to recommend medications that can help improve your headaches.
Diarrhea
You may have diarrhea while you’re taking Xultophy 100/3.6. This is one of the more common side effects in people taking the drug. In a clinical study, 7.5% of people taking Xultophy 100/3.6 had diarrhea.
Mild diarrhea that only lasts for a couple of days isn’t very concerning. However, diarrhea can lead to dehydration (fluid loss from your body) if it happens often or lasts for a longer period of time.
If you have diarrhea, be sure to drink plenty of water and other fluids. Avoid eating or drinking things that contain a lot of sugar (for example, juice and soda). These items can make your diabetes symptoms worse by raising your blood sugar level.
If you have diarrhea after starting Xultophy 100/3.6, it should get better after a few weeks of being on the drug. If you still have diarrhea after being on Xultophy 100/3.6 for a month, or if your diarrhea occurs often, talk with your doctor. They can recommend ways to manage this side effect.
Weight loss or weight gain
Weight loss wasn’t a side effect of Xultophy 100/3.6 during clinical studies. However, Xultophy 100/3.6 is meant to be used in combination with a healthy diet and exercise to treat your diabetes. These measures can lead to weight loss in some people.
Weight gain can actually occur when people use insulin (one of the drugs in Xultophy 100/3.6). In a 26-week clinical trial, people gained an average of 4.4 pounds when they switched from taking liraglutide (Victoza) only to taking Xultophy 100/3.6 (a combination of liraglutide and insulin).
If you have concerns about weight loss while you’re using Xultophy 100/3.6, talk with your doctor. They may refer you to a nutritionist or dietitian. These providers can also help manage your diabetes.
Other drugs are available that can treat type 2 diabetes. Some may be better suited for you than others. If you’re interested in finding an alternative to Xultophy 100/3.6, talk with your doctor. They can tell you about other medications that may work well for you.
Examples of drugs that may be used as alternatives to Xultophy 100/3.6 to treat type 2 diabetes include:
- biguanides, such as:
- metformin (Glucophage, Glumetza, Riomet)
- sulfonylureas, such as:
- glimepiride (Amaryl)
- glipizide (Glucotrol)
- glyburide (DiaBeta, Glynase)
- thiazolidinediones (TZDs), such as:
- pioglitazone (Actos)
- rosiglitazone (Avandia)
- dipeptidyl peptidase-4 (DPP-4) inhibitors, such as:
- sitagliptin (Januvia)
- alogliptin (Nesina)
- linagliptin (Tradjenta)
- saxagliptin (Onglyza)
- meglitinides, such as:
- repaglinide (Prandin)
- nateglinide (Starlix)
- sodium-glucose cotransporter 2 (SGLT2) inhibitors, such as:
- glucagon-like peptide 1 (GLP-1) receptor agonists, such as:
- insulin (long-acting forms), such as:
Combination medications that are similar to Xultophy 100/3.6 are also available. These medications contain a combination of drugs that work together to help regulate your blood sugar levels.
In addition to Xultophy 100/3.6, another combination medication called Soliqua 100/33 (which contains insulin glargine and lixisenatide) is also available to treat diabetes. This alternative drug is described in more detail below.
You may wonder how Xultophy 100/3.6 compares to other medications that are prescribed for similar uses. Here we look at how Xultophy 100/3.6 and Soliqua 100/33 are alike and different.
About
Xultophy 100/3.6 contains insulin degludec and liraglutide. Soliqua 100/33 contains insulin glargine and lixisenatide.
Uses
Both Xultophy 100/3.6 and Soliqua 100/33 are approved to lower blood sugar levels in adults with type 2 diabetes. These medications are meant to be used in combination with a healthy diet and exercise.
Drug forms and administration
Xultophy 100/3.6 and Soliqua 100/33 both come as liquid solutions inside prefilled pens. These medications are both given as injections under your skin (called a subcutaneous injection) once each day.
Side effects and risks
Xultophy 100/3.6 and Soliqua 100/33 both contain drugs that are in the same class of medications (a long-acting insulin and a glucagon-like peptide-1 agonist). So both medications can cause very similar side effects. Below are examples of these side effects.
More common side effects
The more common side effects that can occur with Xultophy 100/3.6 and Soliqua 100/33 (when they’re taken individually) include:
- hypoglycemia (low blood sugar)
- infections, such as a cold
- headache
- nausea
- diarrhea
Serious side effects
These lists contain examples of serious side effects that can occur with Xultophy 100/3.6, with Soliqua 100/33, or with both drugs (when taken individually).
- Can occur with Xultophy 100/3.6:
- gallbladder damage
- possible risk of thyroid cancer*
- Can occur with Soliqua 100/33:
- immunogenicity (your body makes immune cells that can cause allergic reactions)
- Can occur with both Xultophy 100/3.6 and Soliqua 100/33:
- pancreatitis (inflammation in your pancreas)
- severe hypoglycemia (very low blood sugar level)
- kidney damage or failure
- serious allergic reaction
- hypokalemia (low potassium level)
* Xultophy 100/3.6 has a
Effectiveness
The only condition both Xultophy 100/3.6 and Soliqua 100/33 are approved to treat is type 2 diabetes.
These drugs haven’t been directly compared in clinical studies. But separate studies have found both Xultophy 100/3.6 and Soliqua 100/33 to be effective for treating type 2 diabetes.
Costs
Xultophy 100/3.6 and Soliqua 100/33 are both brand-name drugs. There are currently no generic forms of either drug. Brand-name medications usually cost more than generics.
Soliqua 100/33 costs less than Xultophy 100/3.6. The actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
You may wonder how Xultophy 100/3.6 compares to other medications that are prescribed for similar uses. Here we look at how Xultophy 100/3.6 and Lantus are alike and different.
About
Xultophy 100/3.6 contains a combination of insulin degludec and liraglutide, while Lantus contains insulin glargine.
Uses
Xultophy 100/3.6 is approved to lower blood sugar levels in adults with type 2 diabetes. It’s meant to be used in combination with a healthy diet and exercise.
Lantus is approved to lower blood sugar levels in adults and children with type 1 diabetes, and in adults with type 2 diabetes.
Drug forms and administration
Xultophy 100/3.6 comes as a liquid solution inside prefilled pens. Lantus also comes as a liquid solution, which is available in prefilled pens and vials.
Xultophy 100/3.6 and Lantus are both given as injections under your skin (called a subcutaneous injection) once each day.
Side effects and risks
Xultophy 100/3.6 and Lantus both contain long-acting insulin. So both medications can cause very similar side effects. Below are examples of these side effects.
More common side effects
These lists contain examples of more common side effects that can occur with Xultophy 100/3.6, with Lantus, or with both drugs (when taken individually).
- Can occur with Xultophy 100/3.6:
- nausea
- diarrhea
- Can occur with Lantus:
- no unique common side effects
- Can occur with both Xultophy 100/3.6 and Lantus:
- injection site reaction (redness, pain, or swelling at the site of your injection)
- skin thickening near the sites of your injections
- hypoglycemia (low blood sugar)
- weight gain
- infections, such as a cold
- headache
Serious side effects
These lists contain examples of serious side effects that can occur with Xultophy 100/3.6, with Lantus, or with both drugs (when taken individually).
- Can occur with Xultophy 100/3.6:
- pancreatitis (inflammation in your pancreas)
- kidney damage or failure
- gallbladder damage
- possible risk of thyroid cancer*
- Can occur with Lantus:
- few unique side effects
- Can occur with both Xultophy 100/3.6 and Lantus:
- severe hypoglycemia (very low blood sugar)
- serious allergic reaction
- hypokalemia (low potassium level)
* Xultophy 100/3.6/a> has a
Effectiveness
Xultophy 100/3.6 and Lantus have different FDA-approved uses, but they’re both used to treat type 2 diabetes in adults.
The use of Xultophy 100/3.6 and insulin glargine (the active drug in Lantus) in treating type 2 diabetes has been directly compared in two clinical studies. In these studies, people’s hemoglobin A1C (HbA1c) and fasting blood sugar were measured. HbA1c is an average measurement of your blood sugar levels over the past three months. Your fasting blood sugar level is measured after you haven’t eaten anything for at least 8 hours.
One clinical study looked at people who were taking oral diabetes drugs (which are taken by mouth), but who still didn’t have good control of their blood sugar levels. One group took Xultophy 100/3.6, while the other group took insulin glargine. All of these people continued taking their oral diabetes medication during the study.
After 26 weeks, people taking the Xultophy 100/3.6 combination had lowered their HbA1c by 1.97% and had lowered their fasting blood sugar by 63.8 mg/dL. People taking the insulin glargine combination had lowered their HbA1c by 1.59% and had lowered their fasting blood sugar by 59.9 mg/dL.
The second clinical study looked at people who were taking insulin glargine, but who still didn’t have good control of their blood sugar levels. One group received Xultophy 100/3.6, while the other group continued to take insulin glargine. All of these people also took metformin (a diabetes drug taken by mouth).
After 26 weeks of treatment, people taking the Xultophy 100/3.6 combination had lowered their HbA1c by 1.67%. These people also had lowered their fasting blood sugar by 49.9 mg/dL. People using the insulin glargine combination had lowered their HbA1c by 1.16% and had lowered their fasting blood sugar by 49.6 mg/dL.
Costs
Xultophy 100/3.6 and Lantus are both brand-name drugs. There are currently no generic forms of either drug. Brand-name medications usually cost more than generics.
Lantus costs much less than Xultophy 100/3.6. The actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
The Food and Drug Administration (FDA) approves prescription drugs such as Xultophy 100/3.6 to treat certain conditions.
Xultophy 100/3.6 is approved to lower blood sugar levels in adults with type 2 diabetes. It’s meant to be used in combination with a healthy diet and exercise.
With type 2 diabetes, your body can’t use insulin properly. Insulin is a hormone that controls your blood sugar levels. When insulin isn’t used properly, your blood sugar level rises. Over time, high blood sugar can lead to serious complications if it’s not treated. Complications of diabetes can include foot amputations and blindness.
Effectiveness for type 2 diabetes
Xultophy 100/3.6 has been found effective in improving blood sugar levels in people with type 2 diabetes who weren’t able to improve their blood sugar levels enough with other diabetes drugs.
A person’s response to diabetes treatment is often measured by testing hemoglobin A1c (HbA1c). This measurement shows your average blood sugar levels over the past two to three months. The American Diabetes Association recommends a HbA1c goal of less than 7.0% for most adults.
In several clinical studies, people took either Xultophy 100/3.6 or comparison drugs, in combination with diabetes medications taken by mouth. After 26 weeks, people had a decrease in HbA1c of:
- 1.67% to 1.94% with Xultophy 100/3.6, compared to 1.05% to 1.16% with long-acting insulins
- 1.31% with Xultophy 100/3.6, compared to 0.36% with liraglutide
- 1.81% with Xultophy 100/3.6, compared to 1.35% with insulin degludec, and 1.21% with liraglutide
- 1.42% with Xultophy 100/3.6, compared to 0.62% with placebo
- 1.97% with Xultophy 100/3.6, compared to 1.59% with insulin glargine
Xultophy 100/3.6 may be used with other medications to help lower your blood sugar. It’s common to take more than one medication to treat diabetes if using one drug alone doesn’t lower your blood sugar levels enough.
Examples of drugs that can be used with Xultophy 100/3.6 include the following:
Alcohol can affect the way Xultophy 100/3.6 works on regulating your blood sugar. Since alcohol contains sugar, it can also increase your blood sugar level.
You should avoid drinking alcohol, or use extreme caution while drinking alcohol, until you’re comfortable with your Xultophy 100/3.6 dosing.
If you drink alcohol, talk with your doctor about how you should manage your diabetes treatment. Your doctor may recommend that you adjust your dose of Xultophy 100/3.6. Or they may have you check your blood sugar levels more often when you’re drinking alcohol.
Xultophy 100/3.6 can interact with several other medications. It can also interact with certain supplements as well as certain foods.
Different interactions can cause different effects. For instance, some interactions can interfere with how well a drug works. Other interactions can increase side effects or make them more severe.
Xultophy 100/3.6 and other medications
Below are lists of medications that can interact with Xultophy 100/3.6. These lists do not contain all the drugs that may interact with Xultophy 100/3.6.
Before taking Xultophy 100/3.6, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
Taking Xultophy 100/3.6 with certain medications can lead to severe hypoglycemia (low blood sugar level), mask the symptoms of hypoglycemia, or cause hyperglycemia (high blood sugar level).
If you take any of the medications listed below, your doctor may change your dose of the medication. Your doctor may also recommend that you check your blood sugar levels more often while you’re using any of these drugs with Xultophy 100/3.6.
Xultophy 100/3.6 and diabetes medications
Taking Xultophy 100/3.6 with other diabetes drugs can lead to changes in your blood sugar level.
Diabetes drugs that lower your blood sugar
Taking Xultophy 100/3.6 with other diabetes drugs that work to lower your blood sugar can increase your risk of hypoglycemia (low blood sugar). In some cases, hypoglycemia can be severe. See the section “Side effect details” above for more information.
See the section “Alternatives to Xultophy 100/3.6” above for examples of diabetes medications that can increase your risk of hypoglycemia if taken with Xultophy 100/3.6.
Glucagon
Taking Xultophy 100/3.6 with glucagon (GlucaGen, Baqsimi) can increase your risk of hyperglycemia (high blood sugar). Glucagon is used as a rescue medication to treat severe hypoglycemia (low blood sugar) in people with diabetes. It works by raising your blood sugar level.
Thiazolidinediones
Taking Xultophy 100/3.6 with diabetes drugs that belong to a class of medications called thiazolidinediones (TZDs) may increase your risk of heart failure. Taking these drugs together can cause your body to retain fluid, which can increase your risk of heart failure.
If you already have heart failure, taking Xultophy 100/3.6 with TZDs can worsen your condition.
Examples of TZDs which may increase your risk of fluid retention and heart failure if taken with Xultophy 100/3.6 include:
- pioglitazone (Actos)
- rosiglitazone (Avandia)
If you’re taking a TZD, talk with your doctor about your risk of complications if you continue to take the drug while using Xultophy 100/3.6.
Xultophy 100/3.6 and certain heart medications
Taking Xultophy 100/3.6 with certain heart medications can change your blood sugar level. Some heart medications can increase your risk of hypoglycemia (low blood sugar) when taken with Xultophy 100/3.6, while others can increase your risk of hyperglycemia (high blood sugar).
And, some drugs can mask the symptoms of hypoglycemia that you may have. This can make it difficult for you to know if your blood sugar level is getting low.
Examples of heart medications that can increase your risk of hypoglycemia if taken with Xultophy 100/3.6 include:
- certain high blood pressure medications, including:
- angiotensin-converting enzyme (ACE) inhibitors, such as lisinopril (Zestril)
- angiotensin II receptor blockers (ARBs), such as valsartan (Diovan)
- certain cholesterol medications, such as fenofibrate (Lipofen)
- certain arrhythmia (irregular heartbeat) medications, such as disopyramide (Norpace)
Examples of heart medications that can increase your risk of hyperglycemia if taken with Xultophy 100/3.6 include:
- certain diuretics, such as furosemide (Lasix)
- certain cholesterol medications, such as niacin (Niaspan)
Examples of high blood pressure medications can mask your symptoms of hypoglycemia or change how Xultophy 100/3.6 works if they’re taken with Xultophy 100/3.6 include:
- certain alpha agonists, such as:
- clonidine (Catapres)
- beta-blockers, such as:
- metoprolol (Lopressor)
- atenolol (Tenormin)
Xultophy 100/3.6 and certain mental health medications
Taking Xultophy 100/3.6 with certain medications used to treat mental health conditions can change your blood sugar levels. If used with Xultophy 100/3.6, some of these drugs may increase your risk of low blood sugar (hypoglycemia), while other drugs may increase your risk of high blood sugar (hyperglycemia).
Examples of mental health medications that can increase your risk of hypoglycemia when taken with Xultophy 100/3.6 include:
- certain selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine (Prozac)
- monoamine oxidase inhibitors (MAOIs), such as phenelzine (Nardil)
- certain mood stabilizers, such as lithium salts (Lithobid)
Examples of mental health medications that can increase your risk of hyperglycemia when taken with Xultophy 100/3.6 include:
- antipsychotics, such as olanzapine (Zyprexa) and chlorpromazine
- certain mood stabilizers, such as lithium salts (Lithobid)
Xultophy 100/3.6 and hormone medications
Taking Xultophy 100/3.6 with certain medications that contain hormones can change your blood sugar levels. If used with Xultophy 100/3.6, some of these drugs may increase your risk of low blood sugar (hypoglycemia), while other drugs may increase your risk of high blood sugar (hyperglycemia).
One hormone medication called octreotide (Sandostatin) can increase your risk of hypoglycemia if it’s taken with Xultophy 100/3.6. Octreotide is a type of drug called a somatostatin analog.
Examples of hormone medications that can increase your risk of hyperglycemia if taken with Xultophy 100/3.6 include:
- estrogen, such as conjugated estrogens (Premarin)
- certain androgens or testosterone, such as danazol
- growth hormones, such as somatropin (Humatrope)
- thyroid hormones, such as levothyroxine (Synthroid)
- certain adrenal hormones, such as epinephrine (EpiPen)
- oral contraceptives (birth control pills), which contain a form of progestin (such as drospirenone, levonorgestrel, or others) and, in some cases, ethinyl estradiol
Antibiotics, antivirals, and other anti-infective medications
Taking Xultophy 100/3.6 with certain drugs used to treat infections can change your blood sugar levels. If used with Xultophy 100/3.6, some of these drugs may increase your risk of low blood sugar (hypoglycemia), while other drugs may increase your risk of high blood sugar (hyperglycemia).
Examples of drugs that can increase your risk of hypoglycemia if taken with Xultophy 100/3.6 include:
- certain sulfonamide antibiotics, such as sulfamethoxazole/trimethoprim (Bactrim)
- certain anti-infectives, such as pentamidine (Pentam)*
Examples of drugs that can increase your risk of hyperglycemia if taken with Xultophy 100/3.6 include:
- certain antivirals, such as atazanavir (Reyataz)
- certain anti-infectives, such as isoniazid or pentamidine (Pentam)*
* With pentamidine (Pentam), you could experience hypoglycemia first, which could then turn into hyperglycemia.
Xultophy 100/3.6 and other drugs that may cause hypoglycemia
If used with Xultophy 100/3.6, certain other drugs may increase your risk of low blood sugar (hypoglycemia). Examples of these drugs include:
- pain medications, such as salicylates (aspirin)
- vasodilators (used to treat poor blood circulation), such as pentoxifylline
Xultophy 100/3.6 and other drugs that may cause hyperglycemia
If used with Xultophy 100/3.6, certain other drugs may increase your risk of high blood sugar (hyperglycemia). Examples of these drugs include:
- corticosteroids, such as budesonide (Entocort EC, Uceris) and prednisone (Deltasone, Rayos)
- drugs used to treat asthma, such as albuterol (Ventolin) or terbutaline
Xultophy 100/3.6 and herbs and supplements
There aren’t any herbs or supplements that are known to interact with Xultophy 100/3.6. However, you should still check with your doctor or pharmacist before using any of these products while taking Xultophy 100/3.6.
Xultophy 100/3.6 and foods
There aren’t any foods that are known to interact with Xultophy 100/3.6. However, consuming foods that contain carbohydrates and sugars can increase your blood sugar level. Your doctor may adjust your dose of Xultophy 100/3.6, or they may recommend that you check your blood sugar levels more often, depending on your diet.
As with all medications, the cost of Xultophy 100/3.6 can vary.
The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
Financial and insurance assistance
If you need financial support to pay for Xultophy 100/3.6, or if you need help understanding your insurance coverage, assistance is available.
Novo Nordisk, the manufacturer of Xultophy 100/3.6, offers a copay card that may help lower the cost of Xultophy 100/3.6. Visit the drug’s website or call 866-310-7549 to find out more information about the cost of Xultophy 100/3.6 or to apply for a savings card.
You should take Xultophy 100/3.6 according to your doctor or healthcare provider’s instructions. Xultophy 100/3.6 should be injected under your skin (called a subcutaneous injection) once each day. It should be injected into your thighs, abdomen, or upper arms.
The manufacturer of Xultophy 100/3.6 has an instructional video available on their website. This video shows you how to prepare your pen and administer your injection.
Xultophy 100/3.6 is taken using a prefilled, disposable pen. You’ll use a new needle with your pen for each injection. It’s important not to share your pen with anyone else, even if the needle is changed. Using new needles and not sharing your pen with anyone else helps to protect you from getting infections.
For more details on how to safely dispose of your used pens and needles, see the “Xultophy 100/3.6 expiration, storage, and disposal” section below.
When to take
You can take Xultophy 100/3.6 at any time of the day, but you should try to take it at the same time each day.
If you miss a dose of Xultophy 100/3.6, it’s best to wait to take it until your next scheduled dose. You shouldn’t take more than one dose at a time. Doing so can cause your blood sugar level to become too low.
To help make sure that you don’t miss a dose, try setting a reminder in your phone. A medication timer may be useful, too.
Xultophy 100/3.6 is approved to lower blood sugar levels in adults with type 2 diabetes. It’s meant to be used in combination with a healthy diet and exercise.
What type 2 diabetes is
With type 2 diabetes, your body can’t use insulin properly. Insulin is a hormone that controls your blood sugar levels. Insulin allows sugar to move from your bloodstream into your cells. The cells then use sugar for energy.
When insulin isn’t used properly, your blood sugar level rises. And your cells can’t use the sugar for the energy that they need to function the right way.
What Xultophy 100/3.6 does
Xultophy 100/3.6 contains two active drugs that work in the following ways:
- Insulin degludec. Insulin degludec is a long-acting insulin that’s very similar to the insulin made naturally by your body. Insulin works to lower your blood sugar levels. It does this by moving sugar (glucose) from your bloodstream into your cells, such as your muscle and fat cells. Insulin also works by helping to stop your liver from making and releasing more glucose into your bloodstream.
- Liraglutide. Liraglutide works to lower your blood sugar levels by increasing your body’s release of insulin. The drug also decreases glucagon levels in your body. (Glucagon is a hormone that increases your blood sugar. It works in the opposite way that insulin does.) Liraglutide also works by slowing your stomach from emptying after you’ve eaten. This helps your body absorb the sugar from food at a slower, more steady rate. You may also feel fuller for a longer amount of time.
How long does it take to work?
Xultophy 100/3.6 starts to work within several hours after you inject your dose. However, you may not see the full effects of Xultophy 100/3.6 on your average blood sugar levels for a few months.
In animal studies, liraglutide (one of the drugs in Xultophy 100/3.6) caused birth defects and death in some fetuses whose mothers were given the drug. Insulin degludec (the other drug in Xultophy 100/3.6) did not cause birth defects or death in animal fetuses whose mothers were given the drug.
Keep in mind that animal studies don’t always predict what will happen in humans. There isn’t enough information about Xultophy 100/3.6 use in pregnant women to know if it’s safe to take the drug during pregnancy.
However, diabetes can sometimes be harmful during pregnancy. If you’re pregnant or planning to become pregnant, talk with your doctor about the benefits and risks of using this medication and other treatment options for diabetes during pregnancy.
It’s not known if Xultophy 100/3.6 is safe to take during pregnancy. If you’re sexually active, and you or your partner can become pregnant, talk with your doctor about your birth control needs while you’re using Xultophy 100/3.6.
Xultophy 100/3.6 can interact with birth control pills, which may cause high blood sugar levels (hyperglycemia). If you’re taking birth control pills with Xultophy 100/3.6, your doctor may change your dose of Xultophy 100/3.6. Your doctor may also recommend that you check your blood sugar levels more often to monitor for this side effect.
In animal studies, both liraglutide and insulin degludec (both contained in Xultophy 100/3.6) passed into the breastmilk of rats. However, animal studies don’t always predict what will happen in humans. There isn’t enough information available to know if it’s safe to take Xultophy 100/3.6 while you’re breastfeeding.
If you are breastfeeding, or planning to breastfeed, talk with your doctor about whether it’s safe to use this medication while breastfeeding.
Here are answers to some frequently asked questions about Xultophy 100/3.6.
Can I use Xultophy 100/3.6 if I have type 1 diabetes?
No, you shouldn’t use Xultophy 100/3.6 if you have type 1 diabetes. This drug isn’t approved to treat that condition. Xultophy 100/3.6 is only approved to treat type 2 diabetes in adults, when it’s used in combination with a healthy diet and exercise.
Does it matter if I take Xultophy 100/3.6 in the morning or at night?
No, it doesn’t matter. You can take Xultophy 100/3.6 at any time of the day.
However, it’s important to take it at the same time each day to keep Xultophy 100/3.6 levels consistent in your body. The drug lasts in your body for about a day.
Will I still need to use my mealtime insulin if I’m taking Xultophy 100/3.6?
Probably not. It’s not known for sure if Xultophy 100/3.6 can be used with mealtime insulin. Taking more than one diabetes medication together can increase your risk of low blood sugar levels (hypoglycemia).
See the “Xultophy 100/3.6 interactions” section above for more details about drugs that interact with Xultophy 100/3.6.
Can I take Xultophy 100/3.6 if I’ve never taken insulin before?
Yes, you can take Xultophy 100/3.6 even if you’ve never taken insulin in the past. But your starting dose may be different than the dose for someone who’s taken insulin before. Your doctor will recommend the dose of Xultophy 100/3.6 that’s best for you.
This drug comes with several precautions.
FDA warning: thyroid tumor risk
This drug has a
Taking Xultophy 100/3.6 may increase your risk of thyroid tumors and a type of thyroid cancer called medullary thyroid carcinoma (MTC). One of the active drugs in Xultophy 100/3.6 is liraglutide, which has been shown to increase the risk of thyroid tumors in animals. It’s not known if Xultophy 100/3.6 can cause thyroid tumors in humans.
Your doctor will discuss with you the possible risks of thyroid tumors and MTC. Your doctor will also advise that you watch for any symptoms of thyroid tumors or cancer. Symptoms can include having a lump in your neck, trouble breathing or swallowing, or constantly having a raspy voice.
If you develop thyroid tumors or MTC, your doctor may have you stop taking this drug and switch to a different medication. You shouldn’t take Xultophy 100/3.6 if you have multiple endocrine neoplasia syndrome type 2 (MEN 2), which is a condition that causes tumors in your endocrine glands. You should also avoid taking Xultophy 100/3.6 if you or a family member currently has MTC or has had the condition in the past.
Other warnings
Before taking Xultophy 100/3.6, talk with your doctor about your health history. Xultophy 100/3.6 may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Kidney, pancreas, or gallbladder problems. If you have problems with your kidneys, pancreas, or gallbladder, taking Xultophy 100/3.6 may worsen your condition. It could even lead to organ failure (when the organ stops working). Depending on how severe your condition is, your doctor may recommend that you avoid using Xultophy 100/3.6.
- Heart failure. If you have heart failure, taking Xultophy 100/3.6 with other diabetes medications called thiazolidinediones (TZDs) could worsen your condition. If you have new or worsening heart failure during treatment, your doctor may monitor your symptoms or lower your dose of Xultophy 100/3.6. Depending on how severe your heart failure is, they may also recommend that you stop taking Xultophy 100/3.6. See the “Xultophy 100/3.6 interactions” section above for more information.
- Hypokalemia (low potassium). If you have low potassium levels, taking Xultophy 100/3.6 could worsen your condition. Your doctor may monitor your potassium levels while you’re taking Xultophy 100/3.6. If you develop hypokalemia, your doctor may monitor your symptoms or lower your dose of Xultophy 100/3.6. They may also recommend that you stop taking Xultophy 100/3.6, depending on how severe your condition is.
- Hypoglycemia or hyperglycemia. If you have frequent episodes of either hypoglycemia (low blood sugar level) or hyperglycemia (high blood sugar level), Xultophy 100/3.6 can worsen your condition. Your doctor may adjust your dose of Xultophy 100/3.6, recommend that you check your blood sugar levels more often, or switch your diabetes medication altogether.
- Severe allergy. If you’re allergic to any of the ingredients in Xultophy 100/3.6, it may not be safe for you to take Xultophy 100/3.6. Your doctor will recommend other diabetes medications that you can take.
- Pregnancy. There isn’t enough information to know if Xultophy 100/3.6 is safe for people to take during pregnancy. For more information, please see the “Xultophy 100/3.6 and pregnancy” section above.
- Breastfeeding. There isn’t enough information to know if Xultophy 100/3.6 is safe to take while you’re breastfeeding. For more information, please see the “Xultophy 100/3.6 and breastfeeding” section above.
Note: For more information about the potential negative effects of Xultophy 100/3.6, see the “Xultophy 100/3.6 side effects” section above.
Using more than the recommended dosage of Xultophy 100/3.6 can lead to serious side effects.
Overdose symptoms
Symptoms of an overdose can include:
- severe nausea and vomiting
- severe hypoglycemia (low blood sugar level), which may cause:
- dizziness, lightheadedness, weakness, or shakiness
- drowsiness or confusion
- difficulty seeing or speaking
- feeling anxious, moody, or irritated
- hunger
- headache
- fast heartbeat
- sweating
What to do in case of overdose
If you take too much Xultophy 100/3.6, you may develop severe hypoglycemia. If your blood sugar starts dropping very quickly, use a rescue medication such as glucagon (GlucaGen, Baqsimi) to increase your blood sugar level.
But even after using a rescue medication, you should call 911 or go to the nearest emergency room right away. This is because Xultophy 100/3.6 contains a long-acting insulin that may work to lower your blood sugar level for a longer time than the rescue medication works to increase your blood sugar level.
When you get Xultophy 100/3.6 from the pharmacy, the pharmacist will add an expiration date to the label on package of pens. This date is typically 1 year from the date they dispensed the medication.
The expiration date helps guarantee the effectiveness of the medication during this time. The
Storage
How long a medication remains good can depend on many factors, including how and where you store the medication.
Xultophy 100/3.6 pens should be stored in their packaging, away from heat and light. Xultophy 100/3.6 pens shouldn’t be frozen. Don’t use the drug if your pens have been frozen. You should store unopened Xultophy 100/3.6 pens in the refrigerator (36°F to 46°F/2°C to 8°C). You can keep unopened pens refrigerated until their expiration date.
Once you’ve opened a Xultophy 100/3.6 pen, you can store it for up to 21 days at:
- room temperature (59°F to 86°F/15°C to 30°C), or
- in the refrigerator (36°F to 46°F/2°C to 8°C)
After a Xultophy 100/3.6 pen has been opened for 21 days, you’ll need to dispose of the pen.
You should remove the needle from your pen and discard it after each injection of Xultophy 100/3.6. The Xultophy 100/3.6 pen should be stored without the needle attached. This helps prevent infections, and it also prevents medication from leaking out of the pen.
Disposal
If you no longer need to take Xultophy 100/3.6 and have leftover medication, it’s important to dispose of it safely. This helps prevent others, including children and pets, from taking the drug by accident. It also helps keep the drug from harming the environment.
The
You’ll also need to safely dispose of the needles you use for each injection and any emptied pens. Needles and emptied pens should be discarded into a container with a puncture-resistant lid and sides. You can purchase a sharps container at your local pharmacy.
Talk with your doctor or pharmacist for more information on how to safely dispose of your Xultophy 100/3.6 pens and needles.
The following information is provided for clinicians and other healthcare professionals.
Indications
Xultophy 100/3.6 is approved to treat type 2 diabetes in adults, when used in addition to diet and exercise.
Mechanism of action
Xultophy 100/3.6 contains insulin degludec (long-acting insulin) and liraglutide (a glucagon-like peptide 1 agonist). Insulin regulates glucose metabolism by stimulating glucose uptake and blocking glucose production in the liver. Liraglutide increases insulin release, decreases glucagon secretion, and slows stomach emptying.
Pharmacokinetics and metabolism
Steady state of Xultophy 100/3.6 is achieved after about 2 to 3 days of daily dosing. The half-life of insulin degludec is about 25 hours, while the half-life of liraglutide is about 13 hours.
Contraindications
Xultophy 100/3.6 is contraindicated in people with:
- a personal or family history of medullary thyroid carcinoma (MTC)
- a personal history of multiple endocrine neoplasia syndrome type 2 (MEN 2)
- hypersensitivity to any ingredient in Xultophy 100/3.6
- an active hypoglycemia episode
Storage
Prior to using Xultophy 100/3.6, pens should be stored in the refrigerator between 36˚F to 46˚F (2˚C to 8˚C) until their expiration date. After opening Xultophy 100/3.6 pens, they can be stored for up to 21 days either at room temperature (59˚F to 86˚F/15˚C to 30˚C) or in the refrigerator (36˚F to 46˚F/2˚C to 8˚C).
Store Xultophy 100/3.6 pens in their carton, away from heat and light. Do not freeze Xultophy 100/3.6. Avoid using any drug that has been frozen.
Remove the injector needle after each use, and store the Xultophy 100/3.6 pens without the needle attached.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up-to-date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.