Antifungal resistance occurs when fungi evolve the ability to survive the drugs that should kill them. Because only a few antifungal drugs exist, this may restrict the amount of treatment options people can access.
Resistance occurs for several reasons. Some fungi have natural resistance to some types of antifungal drugs, but others develop resistance over time from exposure to the medication.
This article discusses antifungal resistance in more detail, including its causes, who is most at risk from fungal infections, and examples of fungal superbugs. The article also explores what scientists are doing to overcome antifungal resistance and how people can help prevent it.
Antifungal drugs treat fungal infections. When fungi evolve the ability to survive these drugs, doctors may describe them as “antifungal resistant.” In some instances, this
The two main ways antifungal drugs work is
Antifungal resistance may have the most significant effects on public health in comparison with drug resistance to other antimicrobial medications because there are so few antifungal drugs. The reason for this is that humans and fungi both have eukaryotic cells, which are structurally similar, so finding drugs that specifically target fungi with minimal side effects
Bacteria, on the other hand, have prokaryotic cells, which are structurally different from human cells. Prokaryotic cells can be easier to target, which is why antibiotics are more readily available than antifungals.
However, all forms of antimicrobial resistance pose significant threats to human health.
Researchers have proposed several reasons for the rise in antifungal resistance, including:
- Climate change: Changing environments due to factors such as global warming can drive evolution in many species, including fungi.
- Lack of new antifungals: The limited discovery of new antifungal drugs reduces the amount of available treatment options.
- Overuse of fungicides in agriculture: The continued use of fungicides to protect crops and treat fungal infections in livestock drives resistance in some fungi species.
- Overprescription of antifungals: Higher rates of antifungal prescriptions may increase the likelihood of fungi adapting and developing resistance.
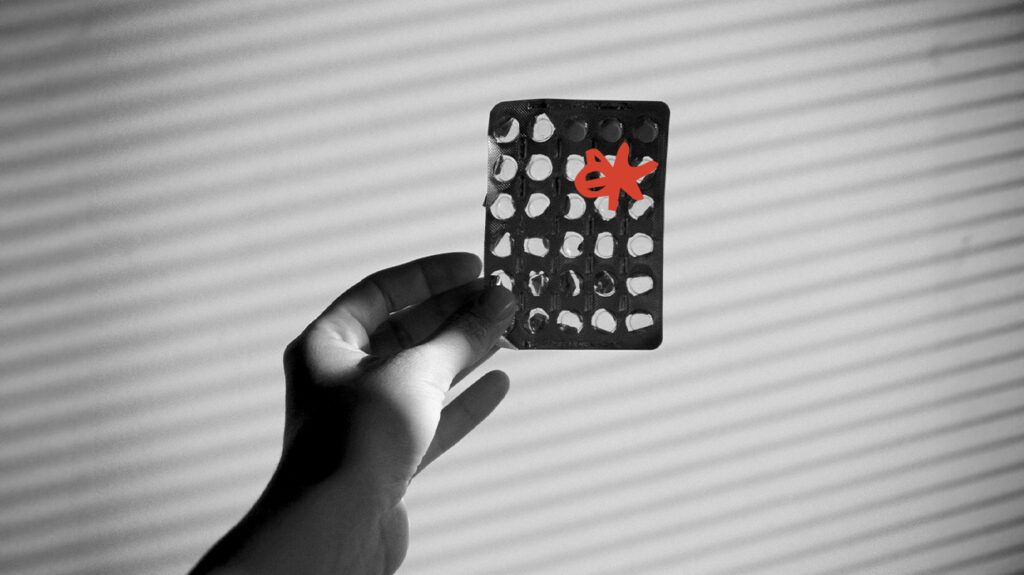
- People not finishing antifungal treatments: Not finishing the entire course of an antifungal treatment can allow stronger strains of fungi to emerge.
- Incorrect disposal of antifungal medicines: Allowing antifungals to enter the environment increases their exposure to fungi, which may lead to more species developing antifungal resistance.
Most people will experience some type of fungal infection in their lives, as fungi are opportunistic.
However, some fungal infections are more serious than others, and they tend to occur in people who are living with a weakened immune system.
Conditions and treatments that can increase a person’s risk of developing a serious fungal infection
- HIV and AIDS
- cancer
- chemotherapy
- immunosuppressant drugs, which people may take after an organ transplant, for example
The fungi associated with life threatening infections in immunocompromised individuals include, but are not limited to:
- Candida
- Aspergillus
- Cryptococcus
- mucormycetes
There are several types of fungi that doctors may have difficulty treating with antifungal drugs. They
- Candida: There are several species of Candida fungus, or yeast, and some of them are resistant to antifungal treatments. They include Candida auris, Candida glabrata, and Candida parapsilosis. People with compromised immune systems
could be at risk of meningitis if a candidiasis infection reaches their brain. - Aspergillus: Aspergillosis can become a life threatening lung infection when Aspergillus
enters the bloodstream . Aspergillus is a common mold that can live indoors and outdoors. Aspergillus fumigatus is one species that is resistant to certain antifungal medications. - Trichophyton indotineae: This
treatment-resistant fungus causes ringworm, which is typically a harmless infection. However, in people with weakened immune systems, the risk of amore severe infection increases.
To help stop the spread of antifungal resistance, the
The five strategic areas to help prevent and stop the spread of resistant fungi include:
- Prevention: Working alongside hospitals and other healthcare facilities to monitor and help prevent the spread of antifungal resistance.
- One Health surveillance: Using tracking and other technologies to
monitor spikes in resistant strains and detect patterns of spread in both hospital and agricultural environments. - Advanced diagnostics: Developing and validating new lab tests to quickly detect new antifungal-resistant strains.
- Research: Understanding how strains develop and studying the different factors that affect spread.
- Collaboration: Working with international partners to help detect and manage spread.
There are
Healthcare professionals
In a healthcare setting, doctors and other healthcare teams can:
- only prescribe antifungal drugs when necessary
- test for treatment-resistant fungi in people whose bodies do not respond well to first-line antifungal drugs
- be aware of the risk factors for treatment-resistant fungi in local communities and healthcare facilities
People staying in the hospital
In hospitals and the community, people can help prevent the spread of antifungal-resistant infections by:
- washing their hands regularly
- finishing their course of antifungal drugs according to a doctor’s guidance
- taking antifungal drugs exactly as prescribed
- talking with their doctor if they do not experience a reduction in symptoms
Antifungal resistance is an increasingly serious public health issue. This is due to several factors, including climate change, overuse of agricultural fungicides, and overprescription of antifungal medications.
Because fungi share a similar cellular structure to humans, developing new antifungal treatments is challenging, as these treatments could unintentionally affect healthy cells throughout a person’s body.
To help reduce the rise in antifungal resistance, the CDC has developed ARSI. This five-point plan aims to stop the spread of antifungal resistance and develop new antifungals to treat infections.
A person can help prevent antifungal-resistant infections by finishing the full course of antifungal medications, washing their hands regularly, and speaking with a doctor if their symptoms do not ease while using antifungal drugs.
