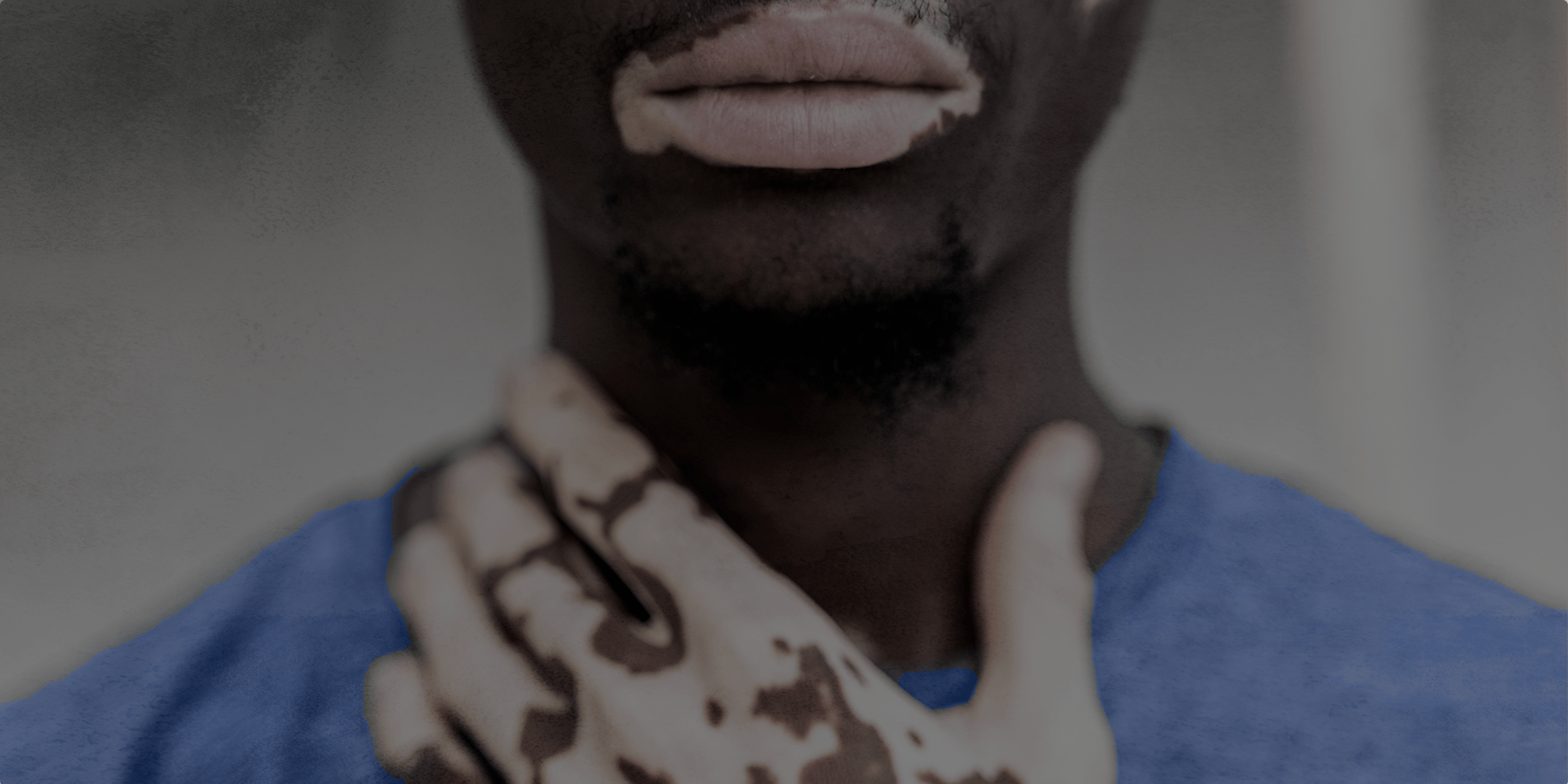
Disparities and inequities pervade every area of health, and dermatology is no exception. In fact, insufficient visual representation of conditions that affect darker skin, coupled with many other inequities in healthcare, has led to particularly stark disparities in health outcomes for People of Color.
Although skin cancer tends to affect more non-Hispanic white people than non-Hispanic Black or Asian people, when it does affect People of Color, doctors tend to diagnose it at a much later stage.
For example, doctors diagnose around
The condition is harder to treat at these later stages, resulting in poorer outcomes for People of Color. The 5-year survival rate for people with skin cancer that has not spread to the lymph nodes is 99%, but
According to the most recent statistics from the American Cancer Society, white adults in the United States with melanoma have a 5-year survival rate of
Systemic discrimination and the bias that the medical community often displays toward white skin also mean that white people are
The current pandemic has made cancer screenings even more infrequent, which could exacerbate these disparities. In April 2020, for example, there were
In this context, Medical News Today spoke with Nada Elbuluk, M.D. — a skin of color expert, practicing dermatologist, and dermatology professor at the Keck School of Medicine at the University of Southern California in Los Angeles — about the causes of health disparities in dermatology and how to remedy them.
We also talked to Dr. Elbuluk about Project IMPACT. This is a global initiative that she helped launch to reduce racial disparities and bias in dermatology education and medical practice. Dr. Elbuluk is the director of clinical impact for VisualDx.
We have lightly edited the interview for clarity.
Project IMPACT and ending inequities in dermatology
MNT: What prompted you to start Project IMPACT, and how did the idea come about?
Dr. Elbuluk: Professionally, I have been working for years in the space of dealing with diversity- and inclusion-related issues, issues related to skin of color and populations of color, marginalized communities, [and] underserved communities — and then I joined the VisualDx team in summer 2020.
Part of why I joined them was that they were also trying to do really good work in the area of improving health disparities for patients of color, and they were looking to bring on somebody who had a similar passion and experience.
They said, “Look, we have this great platform to educate people, and we’ve been [working] for decades, but we need to get the word out there, and we want to do more — can you help us do that?” So, that’s how I joined as director of clinical impact last August.
When I joined, I was thinking about these issues related to health disparities for People of Color — for dermatology, obviously, because it’s my own field, but even beyond that. What can we do to make a difference in this area? We’re always talking about it, we know the disparities are there, but how can we address them?
That’s how the idea of Project IMPACT came to me because I thought, “Let’s actually start to build a community of people who are like-minded — individuals, organizations, companies, [and] institutions who want to move the needle and make a difference in health disparities and health equity.”
MNT: What are some of the ways in which we can make this difference and improve health disparities?
Dr. Elbuluk: [There] are so many ways that we can improve health equity — we’re trying to do it through medical education at VisualDx, but other people are doing it through other realms: through research, […], through public health measures and educating the public, through educating primary care doctors who interface with many patients before a specialist.
There are lots of things we can do, so I thought, “Let’s go bigger than us and […] really create something big and powerful that can make a difference not just nationally, but even globally.”
I like the word “impact” because it’s one simple word, but it carries a heavy meaning. “Impact” is about making a difference. It’s about moving the needle.
I also wanted to use the word “impact” […] as an acronym, which stands for “Improving Medicine’s Power to Address Care and Treatment.”
And that’s really what we’re trying to do. [The question we are asking is,] “How can we use and leverage the education and tools that we have in medicine to give better care to patients, to give treatment that provides equitable care and better outcomes for all?”

Pityriasis rosea. Photography courtesy of VisualDx
The importance of primary care physicians
MNT: What can healthcare professionals, in particular, do?
Dr. Elbuluk: [T]here are so many people in the category of health professionals — physicians, nurses, assistants, pharmacists, technicians — it’s a very broad umbrella, […] and I think each person can look from their standpoint and their own profession and field and think, “How do I interface with patients in my role, and what can I do to improve these issues?”
[I] mentioned I’m a dermatologist, but a lot of my patients, before they see me, they see a primary care physician. Close to 65% of dermatology conditions are initially seen by primary care, not by a dermatologist.
In my job, I feel it’s very important to not only continue medical education with my own colleagues but also for primary care [physicians], who are seeing a lot of our patients before us.
[T]hat can have a downstream effect on improving healthcare outcomes, so that people are not misdiagnosed or don’t have a delayed diagnosis, and they get referred to us in the appropriate time frame.
MNT: What would be a core issue that you would like our readers to be most aware of with regards to health inequities, particularly in skin conditions?
Dr. Elbuluk: I think the number one thing I really want people to know is that health disparities do exist. I think there are some people out there who still have some denial about that.
Disparities do exist, not because of simple differences in biology or genetics — there are some diseases, yes, that are related to that — but a lot of disparities exist because of inequity in treatment, because of systemic issues in our society, because of issues related to socioeconomic status or education level, [and because of] biases related to people’s race and background. So, we have to first acknowledge that this problem exists.
And then I think we have to acknowledge why it’s a problem and the downstream effects that all of those issues lead to.
People often have worse disease burden, increased morbidity, [and] increased mortality, so these are the outcomes, and that’s why it matters that we acknowledge and address these problems.
And when it relates specifically to dermatology and skin of color, we have to acknowledge that many diseases look different in skin of color, and people need to be educated about what that presentation looks like. Unfortunately, a lot of our [textbooks, journals, and educational material] for a long time [have] disproportionately shown the diseases in lighter skin color.
People have been educated and trained to recognize these conditions in lighter skin to the point where often it’s considered the “classic” or “typical” presentation, [but] that’s not necessarily what’s classic or typical in darker skin. So, it is really the responsibility of all of us in healthcare to make sure that the educational materials that are out there are representative of all skin types and backgrounds.
There are diseases and conditions in dermatology [that] include skin, hair, and nails that disproportionately affect People of Color or uniquely affect People of Color. And I think people also need to be aware of those conditions, [so these] are the things that I would say, from an education standpoint, I would want readers to recognize.
The importance of education
MNT: As you’ve highlighted, a lack of education is a key aspect that accounts for a lot of the delays in diagnosis and misdiagnosis of conditions that primarily affect skin of color. What are some of the initiatives that Project IMPACT has taken to tackle this and increase awareness?
Dr. Elbuluk: There are a couple [of] things we’re doing. [S]o, if you go on the Project IMPACT page, you can see images of different conditions in lighter and darker skin side by side — a rolling slide deck.
We also have a section that’s highlighting some of these disparities that I’m talking about. If you go deeper down into our page, we have what’s called our “Spotlight series.” [In this series], every month, we are highlighting a condition [that] disproportionately affects skin [of] color or [that] uniquely presents in skin of color.
[A]nd we’re going to continue to do that with many conditions, over time, so that’s an area where people can educate themselves. We also have a very extensive library that we’re building. There is a section of journal articles, and we have different subheadings that articles are being collected under: One is skin of color dermatology, another one is disparity-related work, another one is skin cancer.
There are a couple of journal articles that are highlighted on the main page, but there’s also an archive you can click on. That will give you many other really high-impact, quality journal articles and peer-reviewed journals covering these topics, and these will cover tons of things related to skin of color. We also have another reference section of textbooks covering the same topics.
For anybody who really wants to educate themselves or learn more, Project IMPACT is meant to be a one-stop shop where somebody can read articles, find textbooks, [and] see blog posts and imaging — all of that to really educate themselves more so they have a starting point, even for someone who has no idea where to start.
[T]here are also some patient-facing applications. [We] have a link to different patient handouts, which are created by different organizations, including The Skin of Color Society and VisualDx. There’s a patient-facing [resource] called SkinSight, which patients can also access for free online. So, these are resources that physicians can also share with their patients.
And we want them to feel empowered about understanding what diagnoses they have and what treatments are involved.

Lyme disease. Photography courtesy of VisualDx
Underrepresentation in clinical trials
MNT: I have seen a series of webinars that aims to tackle disparities that exist within the research community as well. We know that sometimes, even in conditions that disproportionately affect People of Color, these populations are severely underrepresented in clinical trials. What changes would you like to see in this area?
Dr. Elbuluk: I think that’s a really important area where patients of color are underrepresented — in research — and research is the foundation of how we gain knowledge about our conditions and what works and what doesn’t and how to address them. So, if patients of color aren’t being addressed in research, then we’re not really learning about what is best and most appropriate for those populations.
I think the first thing that needs to happen is just more research even related to skin […] conditions in populations of color, as there is a massive shortage in this kind of research.
There’s an article I co-published [where Simone Montgomery and I] looked at the top conditions that brought People of Color into a dermatology office — which are typically discoloration, acne, eczema — and then we looked across the literature that’s been published, for years, to see how many articles were actually published in those areas on skin of color. And it was in the single digits!

Eczema (atopic dermatitis). Photography courtesy of VisualDx
So, part of the problem is [that] people aren’t even focusing on it. Research dollars and time are being spent on a lot of other areas. [T]here is a lot in medicine that we need to research, absolutely, but we can’t forget to also research things that affect communities of color. So, I think that’s the first issue: looking at where our [time, money, and energies] are being focused in the research world.
The second thing is one that you mentioned already, which is the people that are then involved in research studies. When you look at a lot of these clinical trials that are happening, the percentage of patients of color who are enrolled is very small, unfortunately.
If we’re not including a population that’s representative of the U.S. population, or of the global population, then how can we make general inferences? I think [the] recruitment of patients of color into these studies is a challenging issue too, because, unfortunately, historically, there has been abuse of People of Color in medical studies and patients being put into studies without their consent.
Unfortunately, many horrible things that happened in history have created a lot of mistrust among communities of color about medical professionals and medicine in general, so that also is a barrier in terms of trying to increase enrollment.
The importance of trust and cultural humility
MNT: You mentioned earlier that a lot of the diagnoses in dermatology would come through primary care. Is there anything in particular that primary care physicians specifically could do to amend “earned” mistrust and to help rebuild confidence in medicine for patients of color?
Dr. Elbuluk: Yes, I think there are a couple [of] things. Trust is essential, and I think having a relationship of trust as a physician with your patient is everything. If you don’t have that, […] you’re less likely to have compliance, and you’re less likely to have a good successful outcome.
[A]nd how do you build trust? Part of it is through having cultural competence. When patients come to see me, part of it is understanding who they are, what their background is, [and] what’s important to them.
And their race and ethnicity [are] one part of that, and that includes other things too — their occupation, how they spend their day, their socioeconomic status, what they can afford when it comes to treatments, all of these things.
Having that cultural competence — or “cultural humility,” which is the other term being used more recently — is really important, because when patients feel that they’re seen and they’re heard and they’re acknowledged, it makes a difference.
[T]hose things carry a lot of weight for patients, and if I’m a patient of color and my physician understands what’s pertinent to me, to my background, [and] to how I take care of my hair or my skin, all of that is so important in making a connection.
I’ve had patients say that something was recommended or prescribed to them that totally doesn’t fit with their [skin or hair care] routine.
[S]o, in terms of what primary care doctors and dermatologists can do to really improve this experience for patients, I think [it]’s building trust and rapport and making that connection.
[G]etting back to the whole point about education and images, part of why I love using VisualDx so much is that it has such a rich database of images and patients of color. So, when I tell my patient, “This is your diagnosis,” I pull up photos of it.
When I pull up the photo to show patients the images that look like their skin color, it makes a big difference because, when someone sees a picture of someone that looks like them, with the disease that looks like what they have, they [think], “O.K., that does look like me, I’m not alone.”