Duchenne muscular dystrophy (DMD) is a genetic disorder in which a person experiences progressive muscle degeneration and weakness.
DMD is one of the
This article outlines the causes, symptoms, treatment, and outlook for DMD.
A note about sex and gender
Sex and gender exist on spectrums. This article will use the terms “male,” “female,” or both to refer to sex assigned at birth. Click here to learn more.
DMD is the result of mutations in the dystrophin gene located on the X chromosome. These mutations lead to the absence or dysfunction of the dystrophin protein, which is
DMD is an X-linked recessive disorder, meaning it primarily affects males. Females can carry the mutated gene, and it can pass to their children, but they typically do not develop the condition themselves.
Males born to females who carry the gene have a 50% risk of inheriting the mutated gene and developing DMD. Females born to carriers have a 50% risk of being carriers themselves.
Common symptoms of DMD include:
- Muscle weakness: Progressive muscle weakness is the hallmark symptom of DMD. It typically begins in the pelvic muscles and then spreads to the shoulders and upper limbs. Children with DMD may have difficulty getting up from the floor, climbing stairs, or lifting objects.
- Calf enlargement: An early sign of DMD is the
enlargement of the calf muscles due to the replacement of muscle tissue with fatty and connective tissue. - Cardiac issues: DMD can also affect the heart muscle, leading to cardiomyopathy (weakened heart). Cardiac symptoms may include fatigue, chest pain, and heart palpitations.
- Contractures: Joint contractures can develop as the disease progresses. These cause abnormal shortening of muscles and tendons that
can lead to joint stiffness and limited range of motion. - Difficulty walking: Children with DMD
often have a characteristic waddling or “duck-like” gait. They may have trouble walking and may fall more frequently than their peers. - Gower’s sign: To compensate for weaker leg muscles, children with DMD
may use their hands and arms to “walk” up their own body from a seated position. This maneuver is known as Gower’s sign. - Respiratory problems: DMD can affect the respiratory muscles, leading to breathing difficulties. Individuals with DMD may experience shortness of breath, especially during physical activity, and may require respiratory support as the disease advances.
- Scoliosis: Scoliosis (curvature of the spine) is
common in individuals with DMD and may require orthopedic interventions.
DMD is a progressive condition, meaning muscle degeneration and weakness worsen over time. This can lead to significant mobility limitations and loss of muscle function.
In the past, people with DMD typically lost the ability to walk unaided by
There are five general stages in DMD. These are:
- diagnosis (infancy/childhood)
- early ambulatory (childhood)
- late ambulatory (late childhood/adolescence/young adulthood)
- early nonambulatory (adolescence/young adulthood)
- late nonambulatory (adulthood)
Ambulatory refers to the ability to walk unaided. As the disease progresses, it further affects a person’s ability to move around without assistance. People with DMD may experience respiratory or cardiac complications leading to death in their
Symptoms of DMD typically manifest in early childhood, often appearing between
These can include:
- Creatine kinase (CK) blood test: An elevated CK level can indicate muscle damage. A high CK level is not a definitive diagnostic tool but can prompt further evaluation.
- Genetic testing: Genetic testing is the most accurate and definitive method for diagnosing DMD. It involves analyzing a blood sample to identify mutations or changes in the dystrophin gene.
- Muscle biopsy: A muscle biopsy may help identify muscle abnormalities, including the absence of dystrophin protein in the muscle fibers, which is a characteristic of DMD.
Early diagnosis allows for early intervention and access to resources that can improve a person’s quality of life and outlook.
Currently, there is no cure for DMD, but different treatments can help manage symptoms and improve quality of life. These include:
- Cardiac care: DMD can affect the heart muscle. Regular cardiac monitoring and medications
may help to manage heart-related complications. - Corticosteroids: Doctors
often prescribe corticosteroids such as prednisone or deflazacort to help reduce inflammation and slow the progression of muscle weakness. They can help improve muscle strength and function. - Orthopedic interventions: Orthopedic procedures,
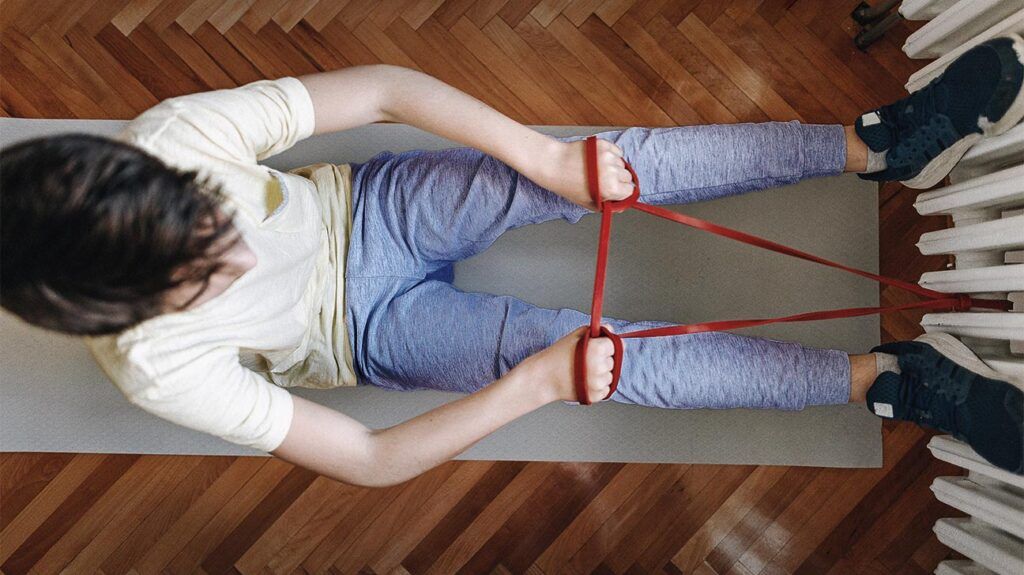
such as bracing or surgical correction of abnormalities, may help to address issues such as scoliosis or joint contractures. - Physical therapy: Physical therapy is
essential for maintaining muscle strength and mobility. It can help people with DMD optimize their physical abilities and reduce the risk of joint contractures. - Respiratory support: As the disease progresses, people with DMD may require respiratory support, including mechanical ventilators or breathing assistance devices.
- Exon skipping medications: These are relatively new drugs that help the body create more dystrophin. Examples are Vyondys 53 and Viltepso. They are not suitable for everyone with DMD, so it is important to undergo genetic testing to determine compatibility.
The outlook for people with DMD has improved over the years due to advances in medical care and supportive therapies. With early intervention and comprehensive care, individuals with DMD
However, DMD
Here are the answers to some common questions about DMD.
Why is it important for someone to know their specific Duchenne mutation?
Different mutations in the dystrophin gene
Where can I find support to cope with DMD?
Sources of support and resources available to help people cope with a diagnosis of DMD
- Muscular Dystrophy Association: This is a nonprofit organization that provides a wide range of resources and support for people affected by neuromuscular diseases, including DMD. They offer educational materials, support groups, and assistance with medical equipment and clinical care.
- Parent Project Muscular Dystrophy: This nonprofit provides information, support, and opportunities for connecting with others who are going through similar experiences. It also funds research and helps to broaden treatment options.
DMD is a progressive neuromuscular condition caused by mutations in the dystrophin gene located on the X chromosome.
People with DMD experience progressive muscle weakness, heart problems, breathing difficulties, and other symptoms.
While there is no cure for DMD, many people living with the condition can lead fulfilling lives with appropriate treatment and palliative care. People affected by DMD should seek support to live with this condition.
