Preeclampsia may develop gradually or suddenly. While it most often occurs after 20 weeks of pregnancy, a person may develop preeclampsia during delivery and up to 6 weeks after giving birth.
Anyone can develop preeclampsia during or in the weeks following pregnancy.
The
However, people with a history of high blood pressure, diabetes, and other health conditions are at a greater risk for the condition.
This article looks at preeclampsia and how quickly it can develop.
While it can develop anytime during pregnancy, preeclampsia typically occurs after
Doctors usually diagnose postpartum preeclampsia within 48 hours of delivery.
However, it is also possible for preeclampsia to occur during delivery as well as up to
Preeclampsia may develop gradually or suddenly. For some people, preeclampsia may flare up in just a few hours. Additionally, some may spend weeks or even months unaware of any signs or symptoms, making it seem as if the condition occurred quite suddenly.
As long as there are no severe preeclampsia symptoms present, a person’s OB-GYN may treat and manage them as an outpatient rather than admit them to the hospital.
Additionally, their OB-GYN may discuss inducing labor around 37 weeks of pregnancy. However, they may need to deliver earlier if test results show the fetus is having development issues.
Along with high blood pressure, some common signs of preeclampsia include:
- protein in the urine
- persistent headache
- vision changes, including blurred vision and seeing spots
- upper abdominal pain or shoulder pain
- nausea or vomiting in the second half of pregnancy
- swelling of the face or hands
- sudden weight gain
- difficulty breathing
When preeclampsia worsens, those symptoms become more severe, and a person’s doctor may discover additional symptoms, including:
- fluid in the lungs
- atypical liver or kidney function
- a low number of blood platelets
High blood pressure alone does not define preeclampsia. A person’s obstetrician will look for accompanying symptoms before diagnosing the condition.
Additionally, some people with preeclampsia may experience no signs or may mistake them for typical pregnancy symptoms.
It is best for a pregnant person to keep regular appointments and contact an obstetrician whenever anything feels suspicious.
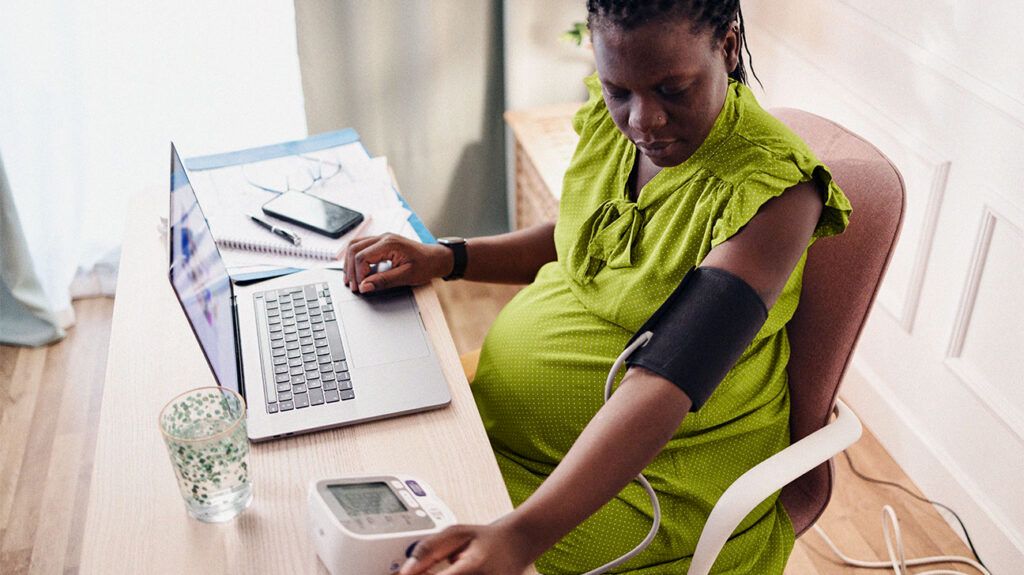
Pregnant people and their OB-GYNs should keep a close eye on blood pressure and other preeclampsia-related symptoms. Some factors put people at a greater risk of developing the condition.
Someone may have a higher risk of developing preeclampsia if they:
- had preeclampsia during a past pregnancy
- are carrying more than one fetus
- have certain other health conditions or illnesses such as diabetes, chronic hypertension, kidney disease, or autoimmune conditions
A person may have a moderate risk for developing preeclampsia if they:
- are pregnant for the first time or if it has been 10 years or longer since their last pregnancy
- had complications during a previous pregnancy
- are aged 35 or older
- have a body mass index over 30
- have a family history of preeclampsia
- became pregnant with IVF
Note that having more than one of these moderate risk factors increases a person’s risk of developing preeclampsia.
Additionally, health disparities regarding race, ethnicity, and
Preeclampsia complications can be severe and even life threatening for both the pregnant person and the fetus.
A few possible complications of preeclampsia include:
- eclampsia, a severe complication of preeclampsia involving seizures
- HELLP syndrome, which causes:
- hemolysis, a breakdown of red blood cells
- elevated liver enzymes
- low platelet count, leading to liver damage, bleeding, and other serious health issues
- placental abruption, which refers to the separation of the placenta from the uterine wall before delivery
- nutrient and oxygen restriction, resulting in fetal growth restriction and potential health complications
Generally, an OB-GYN will help identify preeclampsia risk factors and guide prevention strategies.
Overall, regular prenatal care is critical. Keeping up with appointments allows OB-GYNs to monitor vital signs, including blood pressure, throughout the pregnancy.
Typically, an OB-GYN will work with a pregnant person regarding:
- eating a balanced diet
- staying hydrated
- maintaining a moderate weight
- safe exercises
- relaxation and stress reduction techniques
When a person is high risk, an OB-GYN
Treating mild preeclampsia typically consists of the OB-GYN:
- regularly checking the person’s blood pressure and urine
- having the person check their blood pressure at home regularly
- advising the person on how to monitor the baby’s movements, for example, counting kicks
If the person is at least 37 weeks pregnant, their doctor may recommend inducing labor.
Treating severe preeclampsia may involve:
- hospital admission to monitor vitals
- medications to speed up the baby’s lung development
- medications to control the pregnant person’s blood pressure and prevent seizures
If the preeclampsia worsens and the person is at least 34 weeks pregnant, their doctor may recommend inducing labor or performing a C-section.
Preeclampsia is a potentially serious pregnancy complication that can develop anytime during pregnancy and even several weeks after delivery.
Regular prenatal care, including monitoring blood pressure and urine protein levels, is crucial for early detection. Additionally, in some cases, early delivery can reduce the potential risks for both the pregnant person and the fetus.
Preventive measures, such as a nutritious diet, weight management, approved physical activity and reduced salt intake, can help lower the risk.
Proactive management and, in severe cases, early delivery can lessen the potential risks for both the mother and the baby.
