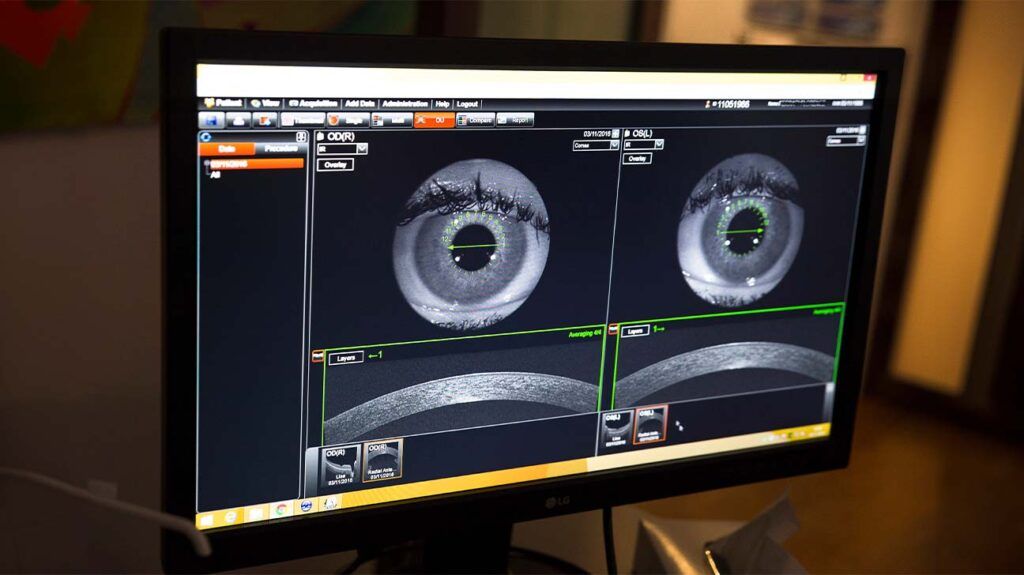
Optical coherence tomography (OCT) is a type of noninvasive imaging test. Ophthalmologists use OCT to create high-resolution, cross-sectional images of the inside of a person’s eye.
OCT can help an ophthalmologist see the different layers of the retina. This helps them map and measure the thickness of these layers.
Measuring the thickness of the different layers of a person’s retina can help an ophthalmologist diagnose a number of medical conditions, such as age-related macular degeneration (AMD) and glaucoma.
Read on to learn more about how OCT works. This article also explains the conditions that OCT can help with and what happens during the procedure.
During OCT, an ophthalmologist
The OCT device then uses these measurements to create images of a person’s retina that are cross-sectional and three-dimensional.
OCT can allow an ophthalmologist to:
- see each of the retina’s layers
- map and measure the layers of the retina
- take pictures of blood vessels beneath the retina
- evaluate changes to the fibers of the optic nerve
By allowing an ophthalmologist to do all the above, OCT can help them diagnose certain eye disorders and guide specific treatments.
Ophthalmologists can use OCT to help diagnose a number of eye conditions. These include:
- AMD
- glaucoma
- macular hole
- macular pucker
- macular edema
- abnormal blood vessels
- blood vessel blockage
- central serous retinopathy
- diabetic retinopathy
- vitreous traction
OCT can also help medical professionals diagnose optic nerve disorders. This is because an ophthalmologist can use OCT to spot changes to the fibers of the optic nerve.
An ophthalmologist may use OCT to help confirm a diagnosis if a person is displaying symptoms of certain eye conditions. Below are the symptoms that may lead an ophthalmologist to use OCT.
Symptoms of macular disorders
The macula is a small area in the center of the retina. It plays a role in helping people clearly see the details of objects.
There are a number of disorders that can affect the macula. OCT can help a medical professional diagnose:
- Macular hole: A macular hole occurs when
an opening forms in the macula. This can cause a person to develop a blur or blind spot in their central vision. - Macular pucker: A macular pucker occurs
when a membrane forms on the surface of the retina and wrinkles or “puckers.” This can occur because of vitreous detachment, which is a condition where the clear gel that fills the eye shrinks and pulls away from the retina. Symptoms of a macular pucker include:- vision that is wavy or distorted
- straight lines may appear bent or wavy
- letters or words may be difficult to read
- having difficulty seeing small details
- Macular edema: Macular edema occurs
when blood vessels leak into the macula. This causes the macula to swell. Macula edema can lead to a person developing blurred vision that worsens over time. - AMD: AMD is a
common condition that occurs when aging leads to macula damage. This can cause the following symptoms to develop:- blurred vision
- blank spots in the vision
- colors may seem less bright than usual
- trouble seeing in low lighting
Learn more about signs of macular degeneration.
Symptoms of glaucoma
Glaucoma is a group of eye diseases that
If an ophthalmologist suspects a person has glaucoma, they may use OCT of the optic nerve to confirm their diagnosis.
A person may not experience any symptoms if they have early stage glaucoma. Over time, a person may slowly experience vision loss.
Over time, this vision loss can worsen and may cause blindness.
Learn more about what glaucoma vision looks like.
Symptoms of central serous retinopathy
Central serous retinopathy is a condition that occurs when fluid builds up under the retina. Medical professionals may also refer to this condition as central serous chorioretinopathy.
Central serous retinopathy can distort a person’s vision. This can cause symptoms such as:
- vision that is:
- distorted
- dimmed
- blurred centrally
- seeing a dark area in the central vision
- having straight lines appear bent or crooked
- seeing objects that appear smaller or further away than they actually are
- seeing white objects with a brown tint to them
If an ophthalmologist suspects a person has central serous retinopathy, they may use OCT to confirm their diagnosis.
Symptoms of diabetic retinopathy
Diabetic retinopathy occurs
Prolonged high blood sugar levels can damage the retina. This occurs when diabetes damages the blood vessels that supply the retina with blood.
In its early stages, diabetic retinopathy usually does not cause symptoms. Some people may notice changes in their vision, such as problems seeing things that are far away.
In its later stages, diabetic retinopathy can cause a person to see dark, floating spots or streaks in their vision.
Without treatment, diabetic retinopathy can lead to blindness. OCT can help a medical professional diagnose diabetic retinopathy.
Learn about the stages of diabetic retinopathy.
Symptoms of vitreous traction
Vitreous is the substance that fills the middle of the eye. Posterior vitreous detachment (PVD)
PVD can cause a person to develop vitreous traction. This is a condition that occurs when part of the vitreous remains stuck to the macula during PVD. This part of the vitreous then pulls on the macula, causing symptoms of vitreous traction.
Some medical professionals refer to vitreous traction as vitreomacular traction.
Symptoms of vitreous traction include:
- distorted vision
- seeing straight lines that appear:
- wavy
- blurry
- blank
- seeing flashes of light in the vision
- seeing objects that are smaller than they actually are
OCT can help a medical professional diagnose vitreous traction.
There are no steps a person needs to take to prepare themselves for OCT.
In some cases, an ophthalmologist
During the procedure, a person will sit in front of the OCT machine. They will then rest their head on the support.
They must then remain still and follow the instructions of the person carrying out the procedure. These instructions will direct the person to look in certain directions throughout the scan.
During the scan, a person may focus on a target within the scanner. They may also see a red line appear during the scan.
OCT is a quick test. The entire procedure will take
If a person has received dilating eye drops during OCT, their eye may be sensitive to light for several hours after the procedure.
OCT is a
OCT uses light rays to create its images. There is no contact during the procedure, and it does not hurt.
Here are some frequently asked questions about OCT.
Does OCT scan show AMD?
A medical professional can use OCT to help diagnose AMD. It
Is optical coherence tomography the same as a computed tomography scan?
OCT is not the same as a computed tomography (CT) scan. OCT uses light rays to create images, and CT scans
During a CT scan, a medical professional aims the X-rays at a part of the person’s body and quickly rotates them around the body. The CT scanner processes the signals that these X-rays produce. The CT scanner then creates cross-sectional images.
Optical coherence tomography (OCT) is a form of noninvasive imaging test that creates high-resolution, cross-sectional images of the inside of a person’s eye.
The procedure can help an ophthalmologist see the different layers of the retina.
OCT can help an ophthalmologist diagnose a number of medical conditions including problems with the macula, AMD, glaucoma, and different types of retinopathy.
