Ulcerative colitis (UC) can lead to various complications. However, following the right treatment and management plan can help reduce these health risks.
UC is a chronic inflammatory condition and the
Without treatment, the inflammation caused by UC can damage the intestines and other organs, leading to other health issues.
Research has found that treatment delays for UC can
This article examines some possible complications of UC to be aware of when discussing treatment options.
Anemia — a low red blood cell count — is one of the most common complications of UC. It can result from a variety of factors, such as:
- inadequate absorption of vitamins and minerals in the gut
- intestinal bleeding
- certain medications that help treat UC
People who have a certain type of anemia, known as iron deficiency anemia, may benefit from iron therapy. Iron supplementation is available as oral or intravenous options, which a person can discuss with a healthcare professional.
Inflammation is the body’s typical response to wound healing, which involves clotting to prevent bleeds. When inflammation remains unmanaged for too long, it can increase the likelihood of developing blood clots.
Blood clots can also develop due to dehydration, fluid loss, and inactivity during disease flares. Some medications doctors use to help treat UC — including corticosteroids and JAK inhibitors — may also increase blood clot risk.
Up to 60% of people with IBD have lower than average bone density, which can increase the likelihood of developing bone issues such as osteoporosis.
Low bone density may result from nutritional deficiencies related to intestinal inflammation or dietary changes. It can also be due to steroids that doctors prescribe to help treat UC.
People with UC may need periodic bone mineral density screening if they are at increased risk for osteoporosis. Calcium and vitamin D supplements can help support bone health.
Inflammation in the intestines increases the likelihood of developing certain types of bowel cancers, including colorectal cancer.
Research estimates that
Experts recommend regular screening — every 1–2 years — with colonoscopy for people with UC.
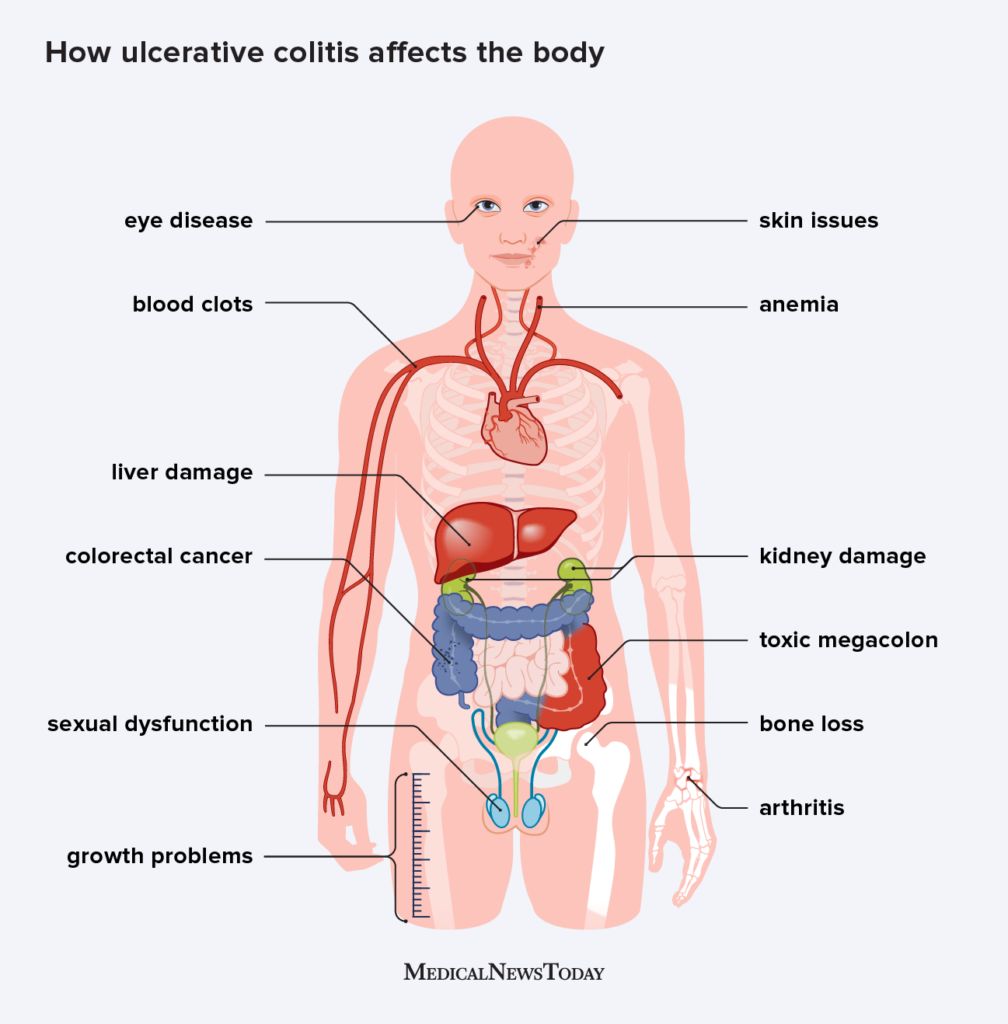
Some people with UC may experience inflammation affecting other parts of their body that can lead to extra-intestinal complications or health issues affecting organs outside the gut. Other specialists may need to help manage these complications.
The most common extra-intestinal inflammatory conditions include:
- arthritis
- skin problems — particularly around the openings of the digestive canal, such as the mouth and anus
- eye diseases
- liver or kidney damage
Among these, primary sclerosing cholangitis is a serious potential extra-intestinal complication. In this condition, inflammation damages the bile ducts of the liver and digestive system, which can increase the risk of colorectal cancer and the need for a liver transplant.
Fulminant colitis is an acute form of UC affecting some people with severe disease. Symptoms
- more than 10 bowel movements a day
- continuous bleeding
- severe abdominal pain or swelling
- symptoms of toxicity, such as fever or an increased heart rate
Fulminant colitis can also lead to other, more severe complications. These include severe anemia and toxic megacolon. Toxic megacolon is a rare condition in which inflammation becomes so intense that gases become trapped, causing swelling and enlargement of the intestines. If not treated quickly, it can cause the intestines to rupture and may require surgery to repair.
Some people who develop UC in childhood may experience issues related to growth.
Growth delays may be due to nutritional problems resulting from decreased appetite and other digestive symptoms that affect food intake and diet. It can also result from decreased absorption of nutrients due to inflammation in the gut, which can contribute to malnutrition.
Inflammation can also influence hormone levels, including growth hormone. Changes in hormone levels can also affect the onset of puberty in young people with UC.
An effective treatment plan may help
A growing body of research suggests that UC may affect aspects of both
This can make the treatment process for people with severe symptoms more complicated. On one hand, treating the symptoms of UC may improve sexual health and satisfaction. However, on the other hand, certain types of treatment — including both medications and surgery — may increase the likelihood of sexual dysfunction.
Managing concerns related to sexual health in UC may involve a multidisciplinary care team, including a gastroenterologist as well as a urologist or OB-GYN, and mental health professionals.
The effects of UC extend beyond the intestines. People living with this condition may be at risk for various health complications. Many are due to inflammation and nutritional problems, but certain UC treatments can also lead to complications.
Management of UC requires a holistic approach to care that addresses the underlying inflammation and symptoms of disease alongside the potential complications. A gastroenterologist can discuss treatment options and make referrals to other specialists to help a person manage all aspects of their health and well-being.