Ventricular fibrillation (VFib or VF) and ventricular tachycardia (v-tach or VT) are two types of heart arrhythmia that occur in the heart’s lower chambers called the ventricles.
The ventricles receive blood from the heart’s upper chambers — the atria — and pump it to the rest of the body.
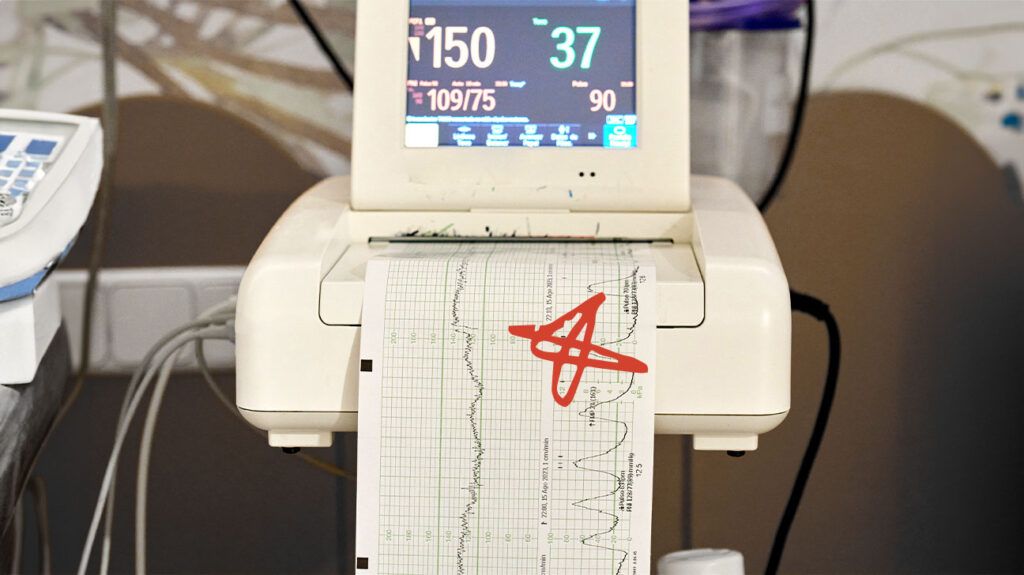
This article describes VF and VT, including their similarities and differences and how each appears on an electrocardiogram (ECG) reading. It also discusses the causes, diagnostic processes, treatments, and outlooks for each condition.
Both VF and VT are types of heart arrhythmia. Although VF and VT are different, they can both cause sudden cardiac arrest. This is a
VF
The
VT
In VT, the ventricles contract rapidly, resulting in the heart beating three or more consecutive beats of
The VT may be sustained or nonsustained:
- Sustained VT: The heart beats rapidly for more than 30 seconds or leads to hemodynamic instability within 30 seconds. Hemodynamic instability is the medical term for insufficient blood flow to the body. Sustained VT can cause cardiac arrest and requires immediate medical intervention.
- Nonsustained VT: The heart beats rapidly for less than 30 seconds, and the incident does not lead to hemodynamic instability. Nonsustained VT resolves without the need for immediate medical intervention.
The key difference between VF and VT is how the ventricles contract.
In VF, the ventricles contract in an
Importantly, VF can also cause a rapid heartbeat or tachycardia. However, its distinguishing feature is that the ventricular contractions are uncoordinated.
Below are some potential causes of VF and VT.
VF causes
Some potential causes of VF
- insufficient blood flow to the heart muscle
- very high or very low potassium levels in the blood
- angina
- heart attack
- heart damage
- problems with the aorta, the main artery that carries blood from the heart to the rest of the body
- cardiomyopathy
- congenital heart disease
- sudden cardiac death from a sudden blow to the area directly over the heart
- heart surgery
- electrocution accidents
- drug toxicity
- sepsis
VT causes
Ischemic heart disease (IHD) is the
Other potential causes of VT include:
- cardiomyopathies
- structural heart disease
- certain inherited heart conditions
- electrolyte imbalances, such as:
- use of illegal drugs, such as cocaine or methamphetamine
- digitalis toxicity, which can occur from a heart medication called digitalis
This section outlines the different diagnostic procedures for VF and VT.
VF diagnosis
When diagnosing VF, a doctor will conduct an ECG to assess the person’s heart rhythm.
Once the individual is in the recovery phase, doctors may also request
- a description of the person’s symptoms before and during the cardiac event
- a family history
- a full medical history
- blood tests to check the following:
- electrolyte levels
- cardiac enzymes
- toxicology
Doctors may also request an echocardiogram and an emergency angiogram to test for underlying heart issues or coronary artery disease (CAD).
VT diagnosis
When diagnosing VT, a doctor may conduct
- a medical history
- a family history
- an ECG to assess the heart’s rhythm
- an echocardiogram to evaluate heart structure and function
- other noninvasive imaging tests, such as cardiac CT scan and cardiac MRI scan
- an invasive coronary angiogram to evaluate suspected CAD
- genetic testing for individuals with a family history of certain heart issues
Below are the treatment approaches for VF and VT.
VF treatments
Ventricular fibrillation is the
According to a
If medics confirm that a person has VF but no pulse, they will deliver direct current cardioversion (DCC). This involves using a defibrillator to send an electric current through the heart to regulate its rhythm.
If VF continues after the person has received three shocks to the heart, medics may administer epinephrine along with medication to stabilize the heart rhythm.
VT treatments
Sustained VT can cause cardiac arrest. People who experience cardiac arrest require defibrillation, emergency resuscitation, and life support. Those who do not experience cardiac arrest but lack sufficient blood flow will require DCC.
Some people with structural heart disease may experience a VT storm. This is the medical term for three or more episodes of sustained VT within
- intravenous (IV) antiarrhythmic drugs
- IV beta-blockers
- antitachycardia pacing
- DCC
Long-term therapies may also be necessary to help manage VT or prevent its recurrence. Treatment will likely include medications to stabilize the heart rhythm.
If this is unsuccessful, a person may require a catheter ablation procedure. This involves destroying a small section of heart tissue responsible for the arrhythmia.
Depending on the cause of the VT, some people may require an implantable cardioverter defibrillator (ICD). This is a battery-powered device that monitors the heart rate.
The
The outlooks for VF and VT are as follows.
VF outlook
The
A
Cardiac defibrillators are now widely available outside hospital settings, improving VF survival rates. However, while defibrillation can reverse VF, its success rate declines at a rate of 5–10% for every minute the treatment is delayed.
Even under ideal circumstances, only 30–40% of people with VF survive. However, many of these individuals develop neurological issues due to the lack of oxygen reaching the brain at the time of cardiac arrest.
Full recovery from VF is rare.
VT outlook
The
VT related to ischemic cardiomyopathy (IC) carries the least favorable outlook. Without treatment, it may cause death within 2 years in up to 30% of cases. However, an ICD significantly improves survival rates.
The review adds that idiopathic VT carries an excellent outlook, with life expectancies almost equal to that of the general population. Idiopathic VT is when it occurs without a known cause.
Is one worse than the other?
VF is the
VF and VT are heart arrhythmias that involve the heart’s lower chambers. VF involves uncoordinated ventricular contractions, while VT involves coordinated but rapid ventricular contractions. Both conditions can result in insufficient blood flow to the rest of the body.
Without immediate treatment, both VF and VT can cause sudden cardiac arrest. This is a potentially fatal condition in which the heart suddenly stops beating.
The immediate treatment for cardiac arrest is defibrillation, which sends an electric shock to the heart to help regulate its rhythm.
The outlook for VF is unfavorable, but the earlier a person with VF receives defibrillation, the better their chance of survival.
The outlook for VT depends on its underlying cause. Ischemic cardiomyopathy-related VT carries the least favorable outlook, though an implantable cardioverter defibrillator can significantly improve survival. Idiopathic VT has the best outlook, with survival rates almost equaling those of the general population.
