Ozempic is a brand-name subcutaneous injection prescribed to help manage blood sugar levels and lower the risk of cardiovascular problems. Ozempic contains the active drug semaglutide and belongs to the GLP-1 agonists drug class.
Ozempic is FDA-approved to:
- improve blood sugar levels in adults with type 2 diabetes, along with diet and exercise
- lower the risk of serious cardiovascular problems in adults with cardiovascular disease and type 2 diabetes
Ozempic may be used by itself or in combination with other diabetes medications. This drug is not used to treat type 1 diabetes and typically isn’t prescribed for people who’ve had pancreatitis. See the “Ozempic uses” section below for details.
Drug details
You’ll find key information about Ozempic below.
- Drug class: glucagon-like peptide-1 receptor agonists (GLP-1 agonists)
- Drug form: solution in a pen that you’ll self-inject by subcutaneous injection
- Generic available? no
- Prescription required? yes
- Controlled substance? no
- Year of FDA approval: 2017
Ozempic is only available as a brand-name medication. It contains the drug semaglutide, which is not currently available in a generic form.
As with all medications, the cost of Ozempic can vary. The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
Drug coupons. You can visit Optum Perks for price estimates of Ozempic. These estimates are based on the use of Optum Perks coupons. Note: Optum Perks coupons cannot be used with any insurance copays or benefits.
Financial and insurance assistance. If you need financial support to pay for Ozempic, or if you need help understanding your insurance coverage, help is available.
An Ozempic Savings Card is available, which can help you pay less for each prescription refill. For more information and to find out if you’re eligible for the card, call 1-877-304-6855 or visit the program website.
A patient assistance program is also available for Ozempic, which can provide no-cost medication to people who qualify. You can learn about this resource here.
Generic version. Ozempic is not available in a generic form. A generic drug is an exact copy of the active drug in a brand-name medication. Generics tend to cost less than brand-name drugs.
To learn more about saving money on prescriptions, check out this article. You can also see this article for information about Ozempic’s cost.
Save on your Ozempic prescription
Save on Ozempic without insurance.
Enter your information:
Location
47201
Dosage
1.5ml ozempic (1 Pen)
Save money without using insurance
Simply show the Optum Perks coupon at your preferred pharmacy or order online and instantly save up to 80% without using insurance. The coupon doesn't expire, so be sure to save it for refills.
Retail price refers to the manufacturer’s published list price and is up to date as of 3/2023. Retail and discounted prices are U.S.-only and can vary based on region and pharmacy. We cannot guarantee that the discounted price listed here will exactly match the price at your pharmacy. Please contact your pharmacy for the exact price.
Optum Perks and Healthline are subsidiaries of RVO Health.
Pricing source:Perks.optum.com

Typically, your doctor will start you on a low dosage and adjust it over time to reach the dosage that’s right for you. They’ll ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to suit your needs.
You can also read this article for more information about Ozempic’s dosage.
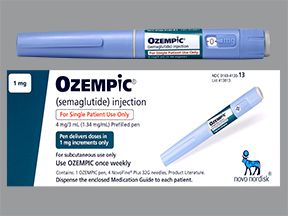
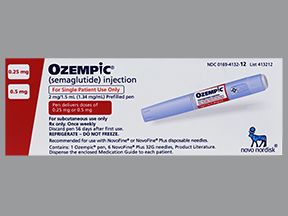
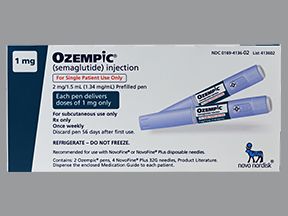
Drug forms and strengths
Ozempic comes as a pen that you use to self-inject the medication. The strengths and doses dispensed by each pen are described in the following table:
| Strength | Dose delivered per injection | Number of doses the pen can inject |
| 2 mg/3 mL (2 milligrams of semaglutide in 3 milliliters of solution), which may also be written as 0.68 mg/mL | 0.25 mg or 0.5 mg | four to eight doses |
| 4 mg/3 mL (1.34 mg/mL) | 1 mg | four doses |
| 8 mg/3 mL (2.68 mg/mL) | 2 mg | four doses |
When you first start Ozempic treatment, you’ll likely use the 2 mg/3 mL pen. If you need a higher dose of Ozempic to help manage your blood sugar levels, your doctor might prescribe a higher strength.
Each Ozempic pen comes with several needles. You’ll use a new needle each time you give yourself an injection.
Ozempic pens are used multiple times, but you should never share a pen with another person.
Dosage for type 2 diabetes
When you first start using Ozempic, you’ll inject 0.25 mg once weekly for 4 weeks. After this, you’ll use 0.5 mg once weekly for 4 weeks.
After 4 weeks, if your blood sugar levels are well-managed, you’ll continue to inject 0.5 mg once weekly. If you need to lower your blood sugar levels even more, your doctor may increase your dosage to 1 or 2 mg once weekly. The maximum recommended dosage of Ozempic is 2 mg once weekly.
You should administer your Ozempic injection on the same day each week. However, you can give the injection at any time of day, with or without meals.
If needed, you can change the day you give your injection. If you do, you must have taken your last dose at least 48 hours before the new day you plan to administer the injection.
What if I miss a dose?
If you miss a dose, take it as soon as you remember, as long as it’s within five days of the date of the missed dose. Then take your next dose on its regular schedule.
But if more than 5 days have passed, or if the date of your next scheduled dose is only 1 or 2 days away, don’t take the missed dose. Instead, just take the next dose on its scheduled day.
Will I need to use this drug long term?
Yes, this drug is typically used long term to help manage type 2 diabetes and to lower the risk of cardiovascular problems.
Ozempic can cause mild or serious side effects. The following list contains some of the key side effects that may occur while using Ozempic. This list does not include all possible side effects.
For more information on the possible side effects of Ozempic or tips on how to manage a troubling side effect, talk with your doctor or pharmacist. You can also read this article for details about Ozempic’s potential side effects.
More common side effects
The more common side effects of Ozempic can include:
- nausea*
- headache
- vomiting
- diarrhea
- stomach pain
- upset stomach
- constipation
- flatulence (passing gas)
These side effects may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk with your doctor or pharmacist.
* For more information on this side effect, see “Side effect details” below.
Serious side effects
Serious side effects from Ozempic aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include the following:
- Pancreatitis (inflammation of the pancreas). Symptoms can include:
- pain in your back and abdomen
- nausea
- vomiting
- unintended weight loss
- fever
- swollen abdomen
- Hypoglycemia (low blood sugar). Symptoms can include:
- drowsiness
- headache
- confusion
- weakness
- hunger
- irritability
- sweating
- feeling jittery
- fast heartbeat
- Diabetic retinopathy (diabetes-related eye problems). Symptoms can include:
- blurred vision
- vision loss
- seeing dark spots
- poor night vision
- Kidney damage. Symptoms can include:
- reduced urination
- swelling in your legs or ankles
- confusion
- fatigue
- nausea
- Gallbladder disease. Symptoms can include:
- gallstones, which can cause pain in your abdomen, nausea, vomiting, and fever
- cholecystitis (inflammation in your gallbladder)
- Thyroid cancer.*
- Allergic reaction.*
* Ozempic has a boxed warning for this side effect. A boxed warning is the most serious warning from the FDA. To learn more, see the “Side effect details” section below.
† For more information on this side effect, see “Side effect details” below.
Side effect details
You may wonder how often certain side effects occur with this drug. Here’s some detail on some of the side effects this drug may cause.
Allergic reaction
As with most drugs, some people can have an allergic reaction after receiving Ozempic. Symptoms of a mild allergic reaction can include:
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- difficulty breathing
It’s not known how often allergic reactions may have occurred in people using Ozempic in clinical trials. However, serious allergic reactions to Ozempic have been reported.
Call your doctor right away if you have a severe allergic reaction to Ozempic. Call 911 or your local emergency number if your symptoms feel life threatening or if you think you’re having a medical emergency.
Nausea
Nausea is the most common side effect of Ozempic. It’s most likely to occur when you first start Ozempic treatment and when your dosage is increased.
Nausea may decrease or go away with continued use of Ozempic. If it doesn’t go away or it becomes severe, talk with your doctor.
Heartburn
Some people who use Ozempic can have heartburn, but this isn’t common. To find out how often this side effect occurred in clinical trials, see Ozempic’s prescribing information.
This side effect may decrease or go away with continued use of the drug. If it doesn’t go away or it becomes severe, talk with your doctor.
Headache
Headache is a common side effect of Ozempic. This side effect may decrease or go away with continued use of the drug. If it doesn’t go away or it becomes severe, talk with your doctor.
Thyroid cancer
Ozempic has a boxed warning from the Food and Drug Administration (FDA) about possible risk of thyroid cancer. A boxed warning is the most serious warning from the FDA.
In animal studies, Ozempic increased the risk of thyroid tumors. However, it’s not known if Ozempic causes thyroid tumors in humans.
There have been cases of thyroid cancer in people using liraglutide (Victoza), a medication in the same drug class as Ozempic. However, it’s not clear if these cases were caused by liraglutide or something else.
Because of the potential risk of thyroid cancer, you should not use Ozempic if you or an immediate family member have ever had a form of cancer called medullary thyroid carcinoma (MTC), or a rare endocrine condition called multiple endocrine neoplasia syndrome type 2.
If you’re using Ozempic and have symptoms of a thyroid tumor, contact your doctor right away. Symptoms can include:
- a mass or lump in your neck
- difficulty swallowing
- difficulty breathing
- a hoarse voice
The Food and Drug Administration (FDA) approves prescription drugs such as Ozempic to treat certain conditions. Ozempic may also be used off-label for other conditions. Off-label use is when a drug that’s approved to treat one condition is prescribed to treat a different condition.
Ozempic for improving blood sugar levels with type 2 diabetes
Ozempic is FDA-approved to improve blood sugar levels in adults with type 2 diabetes, along with lifestyle improvements in diet and exercise. (Ozempic is also approved to lower the risk of cardiovascular problems, and this use is described just below.)
Ozempic may be prescribed alone or in combination with other diabetes medications.
It’s important to note that Ozempic is not used to treat type 1 diabetes. And it’s not typically prescribed for people who have had pancreatitis in the past.
For more information about diabetes, you can refer to our diabetes hub.
Effectiveness for type 2 diabetes
Ozempic has been found to be effective for treating type 2 diabetes. For information on how Ozempic performed in clinical studies, see the drug’s prescribing information.
Guidelines by the American Diabetes Association (ADA) recommend using a GLP-1 agonist, such as Ozempic, in adults with type 2 diabetes who also have one of the following conditions:
- cardiovascular disease (CVD) or a high risk of developing CVD
- kidney disease
- heart failure
These same guidelines also recommend using another medication, such as a GLP-1 agonist like Ozempic, as an option for treating people with type 2 diabetes in whom metformin doesn’t adequately lower their blood sugar.
Ozempic for lowering risk of cardiovascular problems
Ozempic is FDA-approved to help lower the risk of serious cardiovascular problems in adults with heart disease and type 2 diabetes. These risks include stroke, heart attack, and death due to cardiovascular disease. For more information about cardiovascular problems, you can refer to our cardiovascular health hub.
(Ozempic is also approved to help improve blood sugar levels in adults with type 2 diabetes. This use is described just above.)
It’s important to note that Ozempic is not used for type 1 diabetes. And it’s not typically prescribed for people who have had pancreatitis in the past.
Effectiveness for heart problems
In clinical trials, Ozempic was found to be effective for lowering the risk of cardiovascular problems in certain adults. See Ozempic’s prescribing information for details on the drug’s effectiveness in clinical trials.
Guidelines by the American Diabetes Association (ADA) recommend using a GLP-1 agonist, such as Ozempic, in adults with type 2 diabetes who are at increased risk of cardiovascular disease.
Off-label use
In some cases, doctors may prescribe Ozempic off-label. This means prescribing a drug for a purpose other than what it’s been approved for by the FDA.
Ozempic is not FDA-approved for treating type 1 diabetes and has not been studied in people with this condition. However, in some cases, Ozempic may be used off-label to treat type 1 diabetes.
Some experts say that Ozempic and other medications in the same class should not be used in people with type 1 diabetes. They believe that the risk of side effects from these drugs outweighs the potential benefits when used by people with type 1 diabetes.
Ozempic may also be prescribed off-label for help with weight management. However, the drug is not FDA approved for this purpose. See the “Ozempic off-label use for weight loss” section below for details.
Ozempic can decrease appetite. As a result, many people with diabetes who use the drug lose weight.
That said, Ozempic is not FDA-approved for weight management. However, in some cases, doctors may prescribe this drug off-label for weight management. Off-label drug use means prescribing a drug for a purpose other than what it’s been approved for by the FDA.
Be sure to only use Ozempic as prescribed by your doctor. If you have questions about using Ozempic for weight management, talk with your doctor.
How to buy Ozempic
If you think Ozempic could be a good option for you, talk with your doctor. They can help determine whether Ozempic might be right for you and provide a prescription.
Another easy way to purchase Ozempic is by using a telemedicine provider such as Calibrate or Ro Body. Through these services, a licensed telehealth professional will give you a health evaluation. If the evaluation shows that Ozempic could be a helpful option for you, the telehealth professional will provide an electronic prescription. You can then use this prescription to order the medication through the service’s site. After you start taking the medication, the service will provide coaching and other support.
If you get an Ozempic prescription through Calibrate or Ro Body, we encourage you to tell your doctor. It’s important that your doctor know about all medications you take.
Other drugs are available that can help treat type 2 diabetes or lower the risk of serious cardiovascular problems. Some may be better suited for you than others. If you’re interested in finding an alternative to Ozempic, talk with your doctor to learn more about other medications that may work well for you.
Examples of medications that could be alternatives to Ozempic for type 2 diabetes include the drugs listed below.
Alternatives for improving blood sugar levels and lowering risk of cardiovascular problems
- glucagon-like peptide-1 receptor agonists (GLP-1 agonists) such as:
- dulaglutide (Trulicity)
- exenatide (Bydureon BCise, Byetta)
- liraglutide (Victoza)
- lixisenatide (Adlyxin)
- sodium-glucose co-transporter 2 (SGLT2) inhibitors such as:
- canagliflozin (Invokana)
- dapagliflozin (Farxiga)
- empagliflozin (Jardiance)
- ertugliflozin (Steglatro)
- metformin (Glumetza, Riomet), which is a biguanide
- dipeptidyl peptidase-4 (DPP-4) inhibitors such as:
- alogliptin (Nesina)
- linagliptin (Tradjenta)
- saxagliptin (Onglyza)
- sitagliptin (Januvia)
- thiazolidinediones such as:
In addition, the following drugs are alternative options for improving blood sugar levels:
- alpha-glucosidase inhibitors such as:
- acarbose
- miglitol (Glyset)
- sulfonylureas such as:
- chlorpropamide
- glimepiride (Amaryl)
- glipizide (Glucotrol XL)
- glyburide (Diabeta, Glynase Prestabs)
You may wonder how Ozempic compares to other medications that are prescribed for similar uses. Here we look at how Ozempic and Trulicity are alike and different. You can also see this detailed article that discusses the two medications.
Uses
Ozempic and Trulicity are both FDA-approved to:
- blood sugar levels in adults with type 2 diabetes, along with diet and exercise
- cardiovascular problems in adults with cardiovascular disease and type 2 diabetes
Trulicity can also be used in children ages 10 years and older with type 2 diabetes to help improve blood sugar levels.
Ozempic and Trulicity (dulaglutide) are both in the same class of medications, glucagon-like peptide-1 receptor agonists (GLP-1 agonists). This means they work in the same way to improve blood sugar levels in people with type 2 diabetes.
Drug forms and administration
Ozempic and Trulicity both come as a liquid solution that’s available in a pen. They’re both self-injected subcutaneously once per week.
Side effects and risks
Ozempic and Trulicity have similar effects in the body and therefore cause very similar side effects. Below are examples of these side effects.
| Ozempic and Trulicity | Ozempic | Trulicity | |
| More common side effects | • nausea • vomiting • diarrhea • gas • stomach pain • upset stomach • constipation • fatigue | • headache | • decreased appetite |
| Serious side effects | • thyroid cancer* • pancreatitis • low blood sugar • kidney damage • gallbladder disease • diabetic retinopathy (diabetes-related eye problems) • severe allergic reactions | no unique serious side effects | • severe gastrointestinal disease |
* Ozempic and Trulicity both have a boxed warning from the FDA about possible risk of thyroid cancer. A boxed warning is the most serious warning the FDA requires. It alerts doctors and patients about drug effects that may be dangerous.
Effectiveness
Ozempic and Trulicity have both been found to be effective for treating type 2 diabetes. The drugs were directly compared in one
For information on how each drug performed in other clinical studies, see the prescribing information for Ozempic and Trulicity.
Guidelines by the American Diabetes Association (ADA) recommend using a GLP-1 agonist, such as Ozempic or Trulicity, in adults with type 2 diabetes who also have one of the following conditions:
- cardiovascular disease (CVD) or a high risk of developing CVD
- kidney disease
- heart failure
These same guidelines also recommend using another medication, such as a GLP-1 agonist like Ozempic or Trulicity, as an option for treating people with type 2 diabetes in whom metformin doesn’t adequately lower their blood sugar.
The ADA doesn’t recommend any GLP-1 agonist over another. If your doctor decides to prescribe you a GLP-1 agonist, you’ll work together to determine the best one for you.
Costs
The cost of either Ozempic or Trulicity may vary depending on your treatment plan. The price you’ll pay for either drug will depend on your insurance plan, your location, and the pharmacy you use.
Victoza is another medication used to treat type 2 diabetes. Here we look at how Ozempic and Victoza are alike and different.
Uses
Ozempic and Victoza are both FDA-approved to:
- improve blood sugar levels in adults with type 2 diabetes, along with diet and exercise
- lower the risk of serious cardiovascular problems in adults with cardiovascular disease and type 2 diabetes
Victoza can also be used in children ages 10 years and older with type 2 diabetes to help improve blood sugar levels.
Ozempic and Victoza (liraglutide) are both in the same class of medications, which are called glucagon-like peptide-1 receptor agonists (GLP-1 agonists). This means they work in the same way to improve blood sugar levels in people with type 2 diabetes.
Drug forms and administration
Ozempic comes as a liquid solution that’s available in a pen. It’s self-injected subcutaneously once per week.
Victoza also comes as a liquid solution that’s available in a pen. And it’s also self-injected under the skin, but it must be given once daily.
Side effects and risks
Ozempic and Victoza have similar effects in the body and therefore cause very similar side effects. Below are examples of these side effects.
| Ozempic and Victoza | Ozempic | Victoza | |
| More common side effects | • nausea • diarrhea • vomiting • upset stomach • constipation • headache | • stomach pain • gas | • respiratory tract infection • sore throat • back pain • decreased appetite |
| Serious side effects | • thyroid cancer* • pancreatitis • low blood sugar • kidney damage • gallbladder disease • severe allergic reactions | • diabetic retinopathy (diabetes-related eye problems) | no unique serious side effects |
* Ozempic and Victoza both have a boxed warning from the FDA about possible risk of thyroid cancer. A boxed warning is the most serious warning the FDA requires. It alerts doctors and patients about drug effects that may be dangerous.
Effectiveness
Ozempic and Victoza have both been found to be effective for treating type 2 diabetes. These drugs were directly compared in one clinical study, where they were administered in combination with certain oral medications. The study found semaglutide, the active drug in Ozempic, to be more effective than liraglutide, the active drug in Victoza.
Guidelines by the American Diabetes Association (ADA) recommend using a GLP-1 agonist, such as Ozempic or Victoza, in adults with type 2 diabetes who also have one of the following conditions:
- cardiovascular disease (CVD) or a high risk of developing CVD
- kidney disease
- heart failure
These same guidelines also recommend using another medication, such as a GLP-1 agonist like Ozempic or Victoza, as an option for treating people with type 2 diabetes in whom metformin doesn’t adequately lower their blood sugar.
The ADA doesn’t recommend any GLP-1 agonist over another. If your doctor decides to prescribe you a GLP-1 agonist, you’ll work together to determine the best one for you.
Costs
The cost of either Ozempic or Victoza may vary depending on your treatment plan. The price you’ll pay for either drug will depend on your insurance plan, your location, and the pharmacy you use.
You may wonder how Wegovy compares with Ozempic. These medications contain the same active drug, semaglutide. However, they have different approved uses.
Wegovy is approved by the Food and Drug Administration (FDA) for long-term weight management along with exercise and a low calorie diet. Doctors may prescribe this drug for adults and certain children.
Ozempic is not FDA-approved for weight management. However, in some cases, doctors may prescribe this drug off-label for weight management. Off-label drug use means prescribing a drug for a purpose other than what it’s been approved for by the FDA.
Ozempic is FDA-approved to:
- manage blood sugar levels in adults with type 2 diabetes, along with diet and exercise
- lower the risk of serious cardiovascular problems in adults with cardiovascular disease and type 2 diabetes
Ozempic and Wegovy each come as a pen that you can use to self-inject the medication. They tend to cause many of the same side effects, and each has a boxed warning about the possible risk of thyroid cancer. See the “Ozempic side effects” section above for details.
Your doctor or a pharmacist can provide more information about how these drugs compare.
Ozempic can be prescribed by itself or with other medications to improve blood sugar levels in people with type 2 diabetes. In diabetes treatment, two or more medications may often be used together when one medication doesn’t improve blood sugar levels enough.
Examples of diabetes drugs that may be used with Ozempic include:
- canagliflozin (Invokana)
- dapagliflozin (Farxiga)
- glimepiride (Amaryl)
- glipizide (Glucotrol XL)
- glyburide (Diabeta, Glynase Prestabs)
- insulin glargine (Lantus, Toujeo)
- metformin (Glucophage, Glumetza, Riomet)
- pioglitazone (Actos)
Keep in mind that Ozempic may be prescribed together with an exercise and diet plan that’s healthy for you. Be sure to follow your diabetes treatment plan as prescribed by your doctor.
You should use Ozempic exactly as directed by your healthcare professional.
How to inject
Ozempic comes as a pen that is self-injected subcutaneously. There are several steps involved in giving yourself the injection. For fully detailed instructions on how to use an Ozempic pen, you can see the drug’s website. Here are the basic steps:
Step 1. Get your pen ready.
- First, wash your hands.
- Pull off the pen cap. Set aside.
- Check the pen window to make sure the solution is clear and colorless. (If it isn’t, don’t use that pen.)
- Put a new needle on the pen. (A new needle should be used each time you use the pen.)
- Pull off the outer needle cap. Then, pull off the inner needle cap. Both caps can be discarded in the trash.
Step 2. Check the Ozempic flow.
This should be done before the first injection you do with each new pen. If you have already done this step for previous injections with the pen you’re currently using, you can skip to step 3.
- Hold the pen with the needle pointing up.
- Turn the dose counter until it shows the flow check symbol. (It looks like two dots and a line.)
- Press and hold the dose button until the dose counter shows 0. A drop of Ozempic should appear at the needle tip.
- If you don’t see a drop, repeat the process up to six times. If you don’t see a drop after six tries, replace the needle and try again.
- If no drop ever appears, don’t use the pen. Discard it in your sharps container. (You can get a sharps container at your local pharmacy.)
Step 3. Select your dose.
- Turn the dose selector until you see your dose (either 0.25, 0.5, 1, or 2).
Step 4. Inject the dose.
- Wipe your skin at the injection site with an alcohol swab.
- Insert the needle into your skin and hold it in place.
- Press down and hold the dose button until the dose counter shows 0.
- After the dose counter shows 0, count slowly to six before you remove the needle from your skin. This ensures you get the full dose.
Step 5. Discard the needle.
- Remove the needle from the pen.
- Place the used needle in a sharps container.
- Put the pen cap back onto the pen.
Note: After using an Ozempic pen, you can keep using it for up to 56 days. After 56 days, the medication expires, and you should dispose of the pen.
Where to inject
Ozempic can be injected into your abdomen, thigh, or upper arm. The same area can be used each time you inject Ozempic, but you should change the spot where you inject within that area.
Timing
Ozempic can be used at any time of day. The injection should be given on the same day each week. If needed, you can change the day you give yourself Ozempic injections. If you change the day, make sure to wait at least 2 days between each injection.
Ideally, you should inject the drug at roughly the same time each day, even if you change the day. If you’re concerned about changing the time of your injection, talk with your doctor.
Using Ozempic with food
Ozempic can be injected with or without food.
Using Ozempic with insulin
Your healthcare professional may prescribe Ozempic to be used with insulin. Ozempic and insulin can be given at the same time of day. They can also be injected into the same part of the body, such as the abdomen. However, they should not be injected into the exact same spot.
Avoid drinking excessive amounts of alcohol while receiving Ozempic. Alcohol can change your blood sugar levels and increase your risk of low blood sugar.
If you drink alcohol, talk with your doctor about how much, if any, is safe for you.
Ozempic can interact with several other medications. It can also interact with certain supplements.
Different interactions can cause different effects. For instance, some can interfere with how well a drug works, while others can cause increased side effects.
In addition to the information below, you can see this article to learn more about Ozempic’s interactions.
Ozempic and other medications
Below is a list of medications that can interact with Ozempic. This list does not contain all drugs that may interact with Ozempic.
Before using Ozempic, be sure to tell your doctor and pharmacist about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
- Drugs that increase insulin. Using Ozempic with drugs that increase insulin levels in your body can increase your risk of hypoglycemia (low blood sugar levels). Your doctor may prescribe a lower dose of insulin or drugs that increase insulin levels while you’re also using Ozempic. Examples of these drugs include:
- insulin degludec (Tresiba)
- insulin detemir (Levemir)
- insulin glargine (Lantus, Toujeo)
- glimepiride (Amaryl)
- glipizide (Glucotrol XL)
- glyburide (Diabeta, Glynase Prestabs)
- Certain drugs taken by mouth. Ozempic might make your body less able to absorb certain medications that are taken by mouth. If you take oral medications, take them at least 1 hour before you inject Ozempic.
Ozempic and herbs and supplements
Taking certain herbs or supplements with Ozempic might increase the risk of hypoglycemia (low blood sugar levels). Examples of these include:
Ozempic works to help improve blood sugar levels in people with type 2 diabetes, along with diet and exercise. It also works to lower the risk of serious cardiovascular problems in adults with cardiovascular disease and type 2 diabetes. Ozempic does this by reducing the amount of glucose (sugar) in your blood.
How insulin affects blood sugar and cardiovascular risk
Usually, when you eat food, your body releases a hormone called insulin. Insulin helps transport glucose (sugar) from your bloodstream into the cells of your body. The cells then turn the glucose into energy.
People with type 2 diabetes usually have insulin resistance. This means their body doesn’t respond to insulin the way it should. Over time, people with type 2 diabetes may also stop producing enough insulin.
When your body doesn’t respond to insulin the way it should, or if it doesn’t produce enough insulin, this causes problems.
The cells of your body may not get the glucose they need to work correctly. Also, you may get too much glucose in your blood. This is called hyperglycemia (high blood sugar). Having too much glucose in your blood can damage your body and organs, including your eyes, heart, nerves, and kidneys.
Over time, high blood glucose levels can also increase your risk of cardiovascular problems, including a heart attack or stroke.
What Ozempic does
Ozempic belongs to a class of drugs called glucagon-like peptide-1 receptor agonists (GLP-1 agonists). Its mechanism of action (how a drug works) in people with diabetes is increasing the amount of insulin your body makes when blood sugar levels are high. This increased insulin carries more glucose into your cells, causing your blood sugar levels to go down.
Ozempic also decreases blood sugar levels in other ways. For instance, it blocks a chemical in your body that causes your liver to make glucose. It also makes food move out of your stomach more slowly. This means your body absorbs glucose more slowly, which prevents your blood sugar levels from getting too high.
Over time, keeping your blood glucose levels at a consistently healthy level can also help reduce your risk of serious cardiovascular problems.
How long does it take to work?
Ozempic begins to work right after you inject it. But when you’re first starting to use Ozempic, it takes several weeks for its full effects to build up.
This means that you won’t have the full effects of Ozempic until about four to five weeks after your first injection. After this time, you’ll have a steady amount of Ozempic in your body all the time to help manage your blood sugar levels.
If you can become pregnant or are breastfeeding, it’s important to consider whether Ozempic is a safe choice for you.
You can also refer to this article for more information. If you have additional questions, talk with your doctor.
Here are answers to some frequently asked questions about Ozempic.
Is Ozempic used to treat PCOS?
Ozempic is not FDA-approved for treating polycystic ovary syndrome (PCOS). Ozempic’s use for treating this condition hasn’t been studied.
However, some other drugs in the same class of medications as Ozempic are being studied for this use. This class of drugs is called glucagon-like peptide-1 receptor agonists (GLP-1 agonists).
Is Ozempic available as a pill?
Currently, Ozempic is only available as a pen that you use to self-inject the medication.
A different drug called Rybelsus, which contains the same active ingredient as Ozempic (semaglutide), is available in oral tablet form.
Rybelsus and Ozempic are each approved to manage blood sugar levels in adults with type 2 diabetes, along with diet and exercise. However, Rybelsus is not approved to help lower the risk of serious cardiovascular problems in adults with heart disease and type 2 diabetes. Ozempic is approved for this use.
To find out how Ozempic and Rybelsus compare, see this in-depth article. You can also talk with your doctor about these drugs.
Is Ozempic an insulin?
No, Ozempic is not an insulin. Ozempic belongs to a class of drugs called glucagon-like peptide-1 receptor agonists (GLP-1 agonists). It works in people with diabetes by increasing the amount of insulin your body makes when blood sugar levels are high.
Using too much of this medication can increase your risk of serious side effects.
Overdose symptoms
Symptoms of an overdose of Ozempic can include severe nausea, vomiting, or hypoglycemia (low blood sugar).
What to do in case of overdose
If you think you’ve used too much of this drug, call your doctor or seek guidance from America’s Poison Centers at 800-222-1222 or through its online tool. But if your symptoms are severe, call 911 or go to the nearest emergency room right away.
This drug comes with several precautions.
FDA warning: Thyroid cancer
This drug has a boxed warning about the possible risk of thyroid cancer. A boxed warning is the most serious warning from the Food and Drug Administration (FDA). It alerts doctors and patients about drug effects that may be dangerous.
- In animals, Ozempic can increase the risk of thyroid tumors. It’s not known if Ozempic has this effect in humans. You should not use Ozempic if you or an immediate family member has had thyroid cancer in the past, or if you have a rare form of cancer called multiple endocrine neoplasia syndrome type 2.
- If you’re using Ozempic and have symptoms of a thyroid tumor, contact your doctor right away. Symptoms can include a mass or lump in your neck, difficulty swallowing or breathing, and a hoarse voice.
Other warnings
Before starting Ozempic, talk with your doctor about your health history. Ozempic may not be right for you, depending on whether you have certain medical conditions or other factors. These factors include:
- Allergic reaction to Ozempic or other GLP-1 agonists. If you’ve had a severe allergic reaction to other medications in the same drug class as Ozempic (GLP-1 agonists), you may be more likely to have a severe allergic reaction to Ozempic. Talk with your doctor before using Ozempic if you’ve had a severe reaction in the past to one of these drugs.
- Diabetes-related eye disease. If you’ve had diabetic retinopathy in the past, Ozempic may worsen this condition. Diabetic retinopathy is eye damage related to diabetes.
- Pancreas disease. Ozempic has not been studied in people with a history of pancreas disease. Ozempic may cause pancreatitis (inflammation of the pancreas). If you have pancreas disease or a history of pancreas problems, talk with your doctor about this before starting Ozempic. They can help determine whether Ozempic is right for you.
- Kidney disease. If you have kidney disease, Ozempic may worsen your condition. If your condition worsens, you may need to stop Ozempic treatment. If you have severe kidney disease, you may not be able to use Ozempic.
- Using insulin or insulin-increasing drugs with Ozempic. Using Ozempic along with insulin or medications that increase your body’s production of insulin can increase your risk of hypoglycemia, including severe hypoglycemia. Be sure to talk with your doctor about all the medications you take before starting Ozempic treatment. (See the “Ozempic interactions” section above for some examples.) If you notice signs of hypoglycemia after using Ozempic (including drowsiness, headache, weakness, and hunger), talk with your doctor. They may recommend a lower dosage of insulin or the insulin-increasing drug.
Each Ozempic package has an expiration date listed on the label. Do not use Ozempic if the date is beyond the expiration date listed on the label.
Ozempic should be stored in the refrigerator at 36°F to 46°F until you’re ready to use it. Ozempic should never be frozen. If Ozempic freezes, it can no longer be used.
After the first use, the Ozempic pen can be stored in the refrigerator or at room temperature. However, it can only be used for up to 56 days after the first injection. After this time, the pen should be discarded.
The Ozempic pen needle should be removed after each injection. The Ozempic pen should not be stored with the needle attached.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.