Agnosia is a rare condition in which a person cannot recognize and identify objects, people, or sounds through one or more senses, even though their sensory functions are otherwise typical.
Agnosia is a rare neurological disorder that impairs a person’s ability to recognize and identify familiar objects, people, or sounds despite having functioning senses.
In agnosia, the sensory organs — the eyes or ears — are not impaired. However, problems arise from a disconnect between what the organs perceive and how the brain interprets the information.
Agnosia usually
This article examines agnosia, including the types, causes, and outlook.
There are three common types of agnosia.
Visual agnosia
Visual agnosia is a neurological condition in which people have difficulty identifying objects, even though they have typical vision. This difficulty is not due to a lack of basic visual acuity or intellectual capacity but rather a disconnect in the brain’s ability to process and interpret what the eyes see.
Visual agnosia has three subtypes:
Apperceptive agnosia
A person with apperceptive agnosia has trouble perceiving the shapes, sizes, or forms of objects. For example, they may not be able to tell the difference between a circle and a square. This makes it challenging to perform basic tasks such as sorting objects by shape or navigating environments filled with various items.
The underlying cause
Associative agnosia
In associative agnosia, there is a disconnect between the perception of an object and the understanding of its significance or use. For example, a person might see a key but
Unlike in apperceptive agnosia, people with associative agnosia may be able to describe what they see in terms of shape and color but may not recognize the object’s identity or purpose.
People with other forms of associative agnosia may have difficulty recognizing or using objects.
Associative agnosia often results from damage to the parts of the brain involved in higher level visual processing and memory integration.
Prosopagnosia (face blindness)
Prosopagnosia involves difficulty recognizing familiar faces, sometimes even including a person’s own face in the mirror. It can lead to significant social challenges, as recognizing others is crucial for personal interactions.
Prosopagnosia is typically
Auditory verbal agnosia
A person with auditory agnosia has typical hearing but has difficulty interpreting or understanding the meaning of sounds. This disconnect is
Auditory verbal agnosia has two subtypes:
Pure word deafness
People with pure word deafness can hear sounds but have a specific impairment in recognizing spoken words. It is as if they hear words as unintelligible noise.
This
Pure word deafness is associated with damage to the brain’s language processing areas or disruptions in the neural pathways connecting these areas to the auditory cortex.
Nonverbal auditory agnosia
This subtype
Nonverbal auditory agnosia typically involves damage to the parts of the brain responsible for processing complex auditory stimuli. This damage could be due to a stroke, a head injury, or another neurological condition.
Tactile agnosia
In tactile agnosia, a person has difficulty recognizing objects through touch alone despite having typical tactile sensation. This
Autotopagnosia
Autotopagnosia is a subtype of tactile agnosia in which a person cannot visually orient or recognize the parts of their own body. This condition results from a disconnect between a person’s visual-perceptual image of their body and their cognitive understanding or awareness of it.
Possible causes of agnosia include:
- stroke
- head injury
- neurodegenerative diseases
- brain tumors
- infections
- inflammation and damage to brain tissue
- lack of oxygen to the brain (anoxia)
- surgical removal of brain tissue
- developmental disorders
- neurotoxicity
- cerebrovascular disease
Read about traumatic brain injuries.
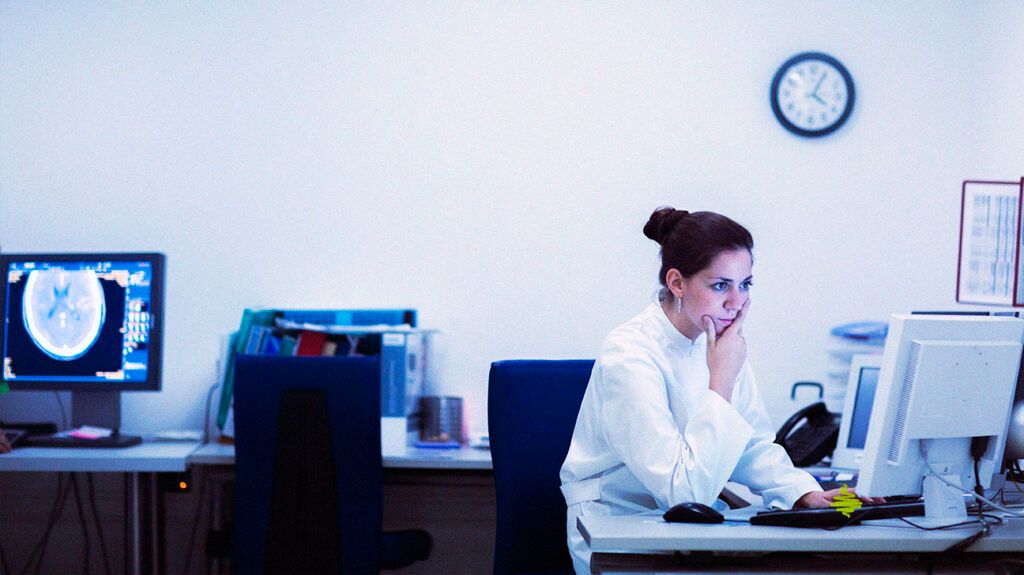
Diagnosing agnosia involves comprehensive neurological evaluations, including brain imaging techniques such as MRI or CT scans, to identify the affected brain areas.
Specific tests for agnosia may involve asking a person to name or describe objects, recognize faces, interpret sounds, and use objects. These tests help determine the type and severity of agnosia.
There is no cure for agnosia. Treatment focuses on managing symptoms and helping people adapt to the condition. The treatment approach is often multidisciplinary, and doctors tailor it to the specific type of agnosia and the person’s individual needs.
Treatment may
- occupational therapy
- speech and language therapy
- physical therapy
- use of other senses
- use of memory aids
- environmental modifications
- exercises to improve recognition
- problem-solving skills
People should speak with a doctor if they experience symptoms that could indicate agnosia or any related neurological issues.
Contacting a doctor early on can be crucial for diagnosis and management. Early intervention can help identify the underlying cause, which can be essential for effective treatment and adaptation strategies. Additionally, some causes of agnosia,
Healthcare professionals can guide people through the necessary steps for diagnosis and treatment, including referrals to specialists such as neurologists or neuropsychologists.
The outlook for someone with agnosia varies widely based on several factors,
If agnosia is due to a stroke or head injury, there might be some potential for recovery, especially with early intervention and rehabilitation.
In cases where agnosia is caused by a progressive neurodegenerative disease, such as Alzheimer’s disease, the condition may gradually worsen over time.
People who have agnosia can find support from many sources,
- Neurologists and neuropsychologists: These specialists can offer medical advice, ongoing care, and guidance on managing agnosia.
- Occupational therapists: These professionals can help people develop strategies to adapt daily tasks and improve quality of life.
- Speech and language therapists: People with auditory agnosia or communication challenges may benefit from speech and language therapy.
- Local or online support groups: By connecting with others who are experiencing similar challenges, a person can find emotional support and practical advice. Online forums and social media groups can be valuable resources. The Brain Injury Association of America lists support groups by state.
- Rehabilitation centers: Facilities specializing in neurological rehabilitation may offer programs tailored for people with agnosia, providing therapy and training to help them cope with the condition.
Agnosia is a rare neurological condition that affects people’s interpretation of sensory information, such as sights and sounds. It results from damage to specific areas of the brain and presents significant challenges.
Neurologists and neuropsychologists may use imaging scans and other tests to determine the nature of a person’s agnosia. Treatment typically involves a multidisciplinary team, including occupational, speech, and physical therapists.
The outlook largely depends on the underlying cause. In some cases, people may experience some recovery, particularly with early diagnosis and intervention.
