Heel pain and tenderness is a common symptom in people with ankylosing spondylitis. This is because inflammation can affect tendons and ligaments in the heel area.
Ankylosing spondylitis is a type of arthritis that primarily affects the spine, though it can also affect other areas, including the heel.
Ankylosing spondylitis causes inflammation of the spinal joints (vertebrae) that can lead to severe, chronic pain and discomfort.
This article examines heel pain and ankylosing spondylitis, why it happens, how to treat it, and more.
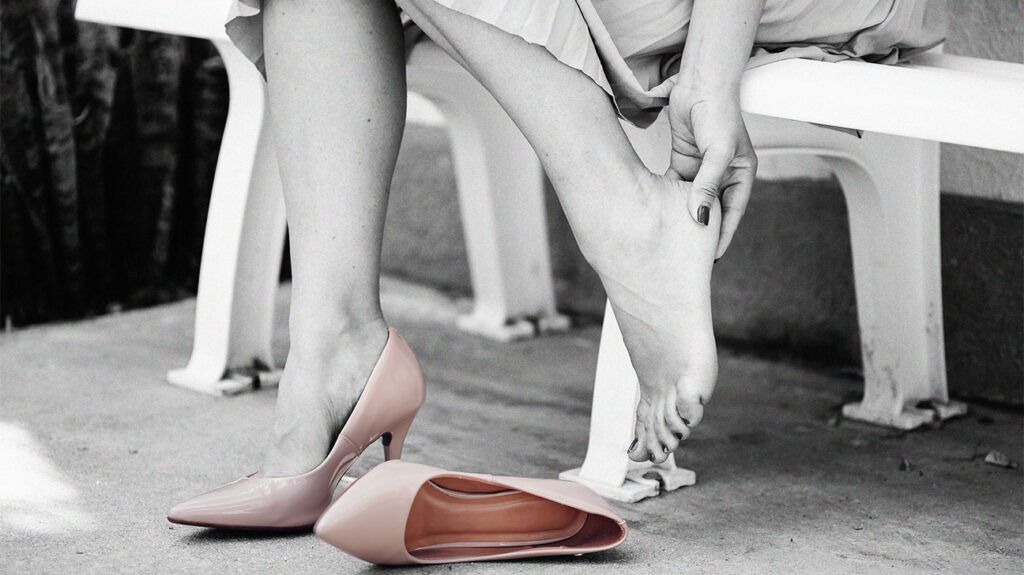
Heel pain is a common symptom in people with ankylosing spondylitis. This pain is often due to enthesitis, which is inflammation where tendons and ligaments attach to bone.
This inflammation can cause pain and tenderness in the heel, making it difficult to walk or stand.
In the case of ankylosing spondylitis, this inflammation often occurs at two key locations in the heel:
- Achilles tendon: This is the prominent tendon at the back of the heel. Inflammation here
can cause pain and stiffness in the Achilles area. - Plantar fascia: This is a band of tissue at the bottom of the foot. Inflammation of the plantar fascia
can lead to pain under the heel, which is especially noticeable when standing or walking after a period of rest.
This heel pain can be a significant symptom for many individuals with ankylosing spondylitis, affecting mobility and quality of life.
Treating the underlying ankylosing spondylitis may alleviate some of the symptoms, such as heel pain.
Treatment and management of ankylosing spondylitis involves multiple approaches specific to the individual’s symptoms and overall health. Treatment may include the following:
Medication
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These
are often the first line of treatment. They help reduce inflammation and alleviate ankylosing spondylitis pain, such as heel pain. - Biologic agents: For more severe cases of ankylosing spondylitis, biologic medications, such as TNF inhibitors, can be effective in managing inflammation. Doctors recommend these if NSAIDs are inadequate.
- Disease-modifying antirheumatic drugs (DMARDs): In some cases, these drugs
can slow the progression of the disease. - Corticosteroids: Doctors
occasionally recommend these for short-term relief of severe inflammation. They administer them via injection. However, they would not inject them in the Achilles area due to a risk of tendon damage.
Physical therapy
- Exercise regimen: Regularly performing certain exercises, especially those that focus on stretching and strengthening,
can help maintain joint flexibility and muscle strength. - Posture training: Maintaining proper posture can
help reduce strain on affected areas. - Pain management techniques: These may
include hot and cold therapy, ultrasound therapy, or electrical stimulation to manage pain.
Orthotics and supportive devices
- Custom orthotics: Specially designed shoe inserts
can provide better arch support and cushioning, reducing heel stress. - Heel cups or pads: These can alleviate pressure and cushion the heel area.
- Supportive footwear: Shoes with good cushioning and support can be beneficial in reducing heel pain.
Lifestyle modifications
- Regular exercise: Low impact activities such as swimming or cycling can help a person maintain flexibility and strength without putting too much strain on the joints.
- Weight management: Maintaining a moderate weight
can reduce stress on the joints. - Smoking cessation: Smoking can exacerbate symptoms and potentially worsen the disease progression.
People with ankylosing spondylitis may consider working closely with their healthcare team to manage symptoms and maintain mobility.
It is best to contact a doctor if a person experiences any of the following situations related to ankylosing spondylitis and heel pain:
- New or worsening symptoms: if someone experiences new symptoms, such as increased heel pain, stiffness, or swelling, or if their existing symptoms worsen significantly
- Difficulty in daily activities: if heel pain or other symptoms of ankylosing spondylitis interfere with a person’s daily activities, such as walking, standing, or working
- Side effects of medications: if someone experiences concerning side effects from medications prescribed for ankylosing spondylitis
- Symptoms affecting other parts of the body: if a person notices symptoms such as vision changes, chest pain, or breathing difficulties, as ankylosing spondylitis can affect other parts of the body, including the eyes, heart, and lungs
- No improvement with current treatment: if the current treatment plan is not providing relief or if symptoms continue to progress despite treatment
Here are the answers to some commonly asked questions about ankylosing spondylitis and heel pain.
What autoimmune disease causes heel pain?
There are a few different autoimmune diseases that can cause heel pain, including:
- Ankylosing spondylitis: This condition can cause heel pain due to enthesitis, which is inflammation where tendons and ligaments attach to bones. Enthesitis may affect the Achilles tendon and the plantar fascia.
- Rheumatoid arthritis (RA): This is another autoimmune disorder that can cause heel pain. It can affect the ankle joint and the joints connecting the toe to the forefoot. RA leads to inflammation in these joints, causing foot and heel pain.
- Psoriatic arthritis: Often associated with psoriasis, this condition can also affect the tendons and ligaments in the feet and heels, leading to pain and inflammation. It can also cause swelling in the toes.
- Reactive arthritis: This condition
can lead to inflammation of the joints and tendons, including those in the heel, often triggered by an infection in another part of the body.
What does ankylosing spondylitis do to the feet?
Ankylosing spondylitis can lead to several issues in the feet:
- Enthesitis: Inflammation at the sites where tendons and ligaments attach to the bones. This can affect the Achilles tendon, causing Achilles tendinitis and leading to pain and stiffness in the back of the heel.
- Arthritis: Joint inflammation can occur in the feet, leading to pain, stiffness, and swelling.
- Bone formation: In advanced cases, abnormal bone growth
can lead to deformity and impaired function in the feet. - Achilles tendinitis: Inflammation of the Achilles tendon can cause pain and stiffness in the back of the heel.
Does ankylosing spondylitis cause pain walking?
Yes, ankylosing spondylitis can cause pain while walking. This can be due to several reasons:
- Stiffness and inflammation: Stiffness in the spine, hips, or feet can make walking uncomfortable or painful.
- Enthesitis: Inflammation at the Achilles tendon or plantar fascia can make each step painful, especially in the heel area.
- Reduced flexibility: Reduced flexibility in the spine can
affect overall posture and gait, leading to discomfort while walking.
Managing heel pain due to ankylosing spondylitis may involve medications, such as NSAIDs and DMARDs, physical therapy, and sometimes surgery in severe cases.
Experts recommend that people with ankylosing spondylitis stay active and maintain a healthy lifestyle to manage their symptoms effectively.
