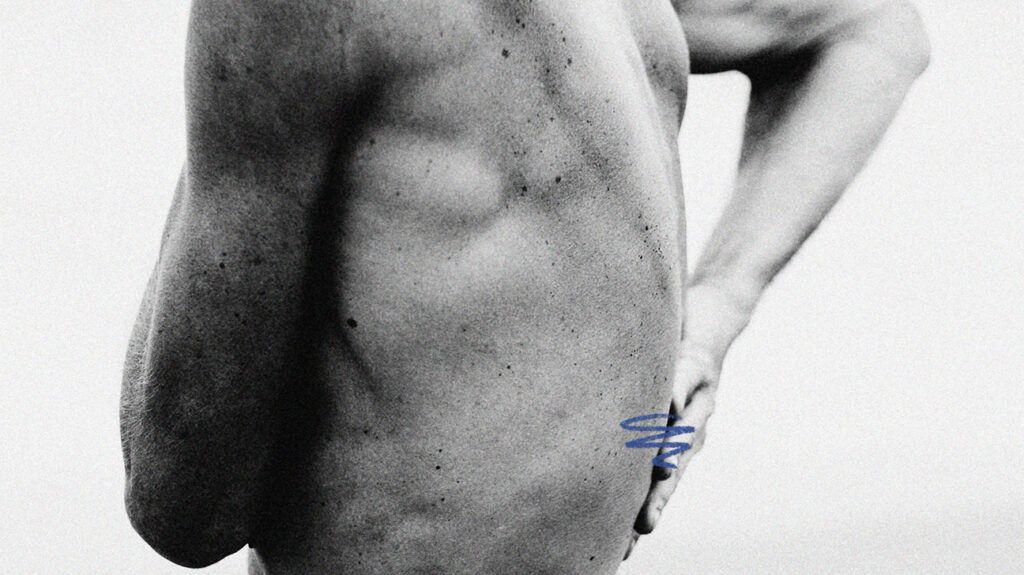
Irritable bowel syndrome (IBS) primarily affects the digestive system. However, many people with IBS also experience back pain and other symptoms.
IBS is a complex gastrointestinal condition that involves various symptoms, including abdominal discomfort, bloating, and irregular bowel movements. While these digestive issues are commonly recognizable, other issues can also present unexpectedly.
One seemingly unrelated but common symptom is back pain.
In this article, we explore the connection between IBS and back pain. We discuss the underlying mechanisms, potential triggers, and strategies for managing this uncommon aspect of IBS.
IBS can cause back pain and various other symptoms. Primarily, people with IBS experience:
- gas
- cramping
- abdominal pain
- diarrhea
- constipation
Symptoms vary in severity, and people may have symptom-free periods.
Experts do not fully understand what causes IBS, although they believe it involves the gut-brain connection, which is how the brain interacts with the digestive system. Additionally, it is unclear why some experience back pain with IBS. However, it is a fairly common issue, affecting between 28% and
Experts believe back pain may be referred pain, meaning it originates elsewhere, but a person can feel it in the back.
One possible reason
Another possibility is that the digestive symptoms of IBS, such as gas pressure, spasms of the colon, or painful, swollen intestines, could trigger pain in the abdomen and lower back.
Something else could also be responsible for the pain. Individuals with IBS tend to have other health issues, including:
- interstitial cystitis, which is a chronic condition causing bladder pressure and pain
- fibromyalgia, a chronic pain syndrome
- other inflammatory conditions, such as rheumatoid arthritis
Any of these conditions could be causing the back pain.
If a person experiences back pain related to IBS, they need to reach out to a doctor in the following situations:
- symptoms worsen, or new ones develop
- the pain is persistent or severe, or there are also other concerning symptoms, such as numbness, weakness, or changes in bowel or bladder habits
- unexplained weight loss occurs
Also, if back pain or IBS symptoms interfere with daily activities, sleep, or quality of life, people can consult a doctor about managing these.
Treating back pain relating to IBS may be challenging, but various management approaches exist.
An effective regimen may involve a combination of the
At-home measures
These include:
- Maintaining a balanced diet: Pay attention to diet and consider dietary modifications, such as reducing trigger foods that worsen IBS symptoms. Avoiding gluten and following alow FODMAP diet may also be helpful.
- Undergoing stress management: Practice stress-reduction techniques, such as relaxation exercises, meditation, or yoga, as stress can worsen IBS and back pain.
- Maintaining posture and ergonomics: Maintain good posture and ensure ergonomic support while at work or engaging in activities that may strain the back.
Medical treatment
These include:
- Medications: Doctors may prescribe medications to manage IBS symptoms, which can indirectly ease associated back pain. These medications include the below:
- Loperamide, rifaximin (Xifaxan), and eluxadoline (Viberzi) may help with diarrhea.
- Lubiprostone (Amitiza), linaclotide (Linzess), and plecanatide (Trulance) can ease constipation.
- Antispasmodics and low dose antidepressants may also be an option for some.
- Physical therapy: Certain exercises and stretches can help improve posture, reduce muscle tension, and alleviate back pain.
- Pain management: Over-the-counter or prescription pain relief medications and injections may help manage back pain.
Complementary treatment
These include:
- Hypnotherapy: Hypnosis begins with gradual relaxation and then the introduction of calming mental images or sensations that help address IBS symptoms. A person may require weekly sessions over several months before they can notice results.
- Biofeedback: This therapy aims to teach people to control certain bodily functions,
potentially helping with pain management. - Other therapies: Acupuncture, traditional Chinese medicine, or herbal remedies may relieve IBS-related symptoms and back pain.
People can work closely with their healthcare professionals to develop a personalized treatment plan for their specific needs and symptoms. They may need to try various approaches before settling on a management plan that works for them.
Back pain can be an unexpected and challenging symptom for individuals with IBS.
While health experts do not fully understand the exact link between IBS and back pain, effective strategies can help manage this discomfort.
Monitoring symptoms, seeking medical advice, and adopting a holistic treatment approach can help individuals with IBS-related back pain minimize the effect of these issues on their daily routines.
