Retinal detachment is when the retina detaches from the supporting tissue at the back of the eye. Secondary, or exudative, retinal detachment occurs in response to another condition, such as inflammation, blood vessel problems, or injury.
Since retinal cells are necessary for vision, retinal detachment can cause permanent vision loss and is only avoidable with prompt treatment. Surgery and anti-inflammatory medications are ways to treat secondary retinal detachment.
This article provides an overview of secondary retinal detachment before discussing its symptoms and causes. It also details the diagnosis and treatment for this condition.
According to a
Doctors and scientists do not generally use the term secondary retinal detachment. Instead, they may
A 2018 study states that according to other studies, for certain forms of retinal detachment, there is a
According to the
Retinal detachment can affect one or both eyes. Some common symptoms include:
- impaired vision
- a lot of new floaters in the field of vision
- flashes of light
- a dark shadow, or “curtain,” affecting the sides or middle of the field of vision
Anyone with symptoms of retinal detachment needs to seek medical attention immediately. This could be from an eye specialist or emergency room staff.
Exudative retinal detachment
- inflammatory bowel disease
- idiopathic orbital inflammatory disease, an inflammatory lesion of the eye orbit
- Behçet disease
Other conditions may include:
Exudative retinal detachment may also result from injury, trauma, or surgical procedures.
Research has shown that a second retinal detachment is a possible complication of surgery for retinal detachment. However, a second retinal detachment can arise for the same reasons as the first.
A
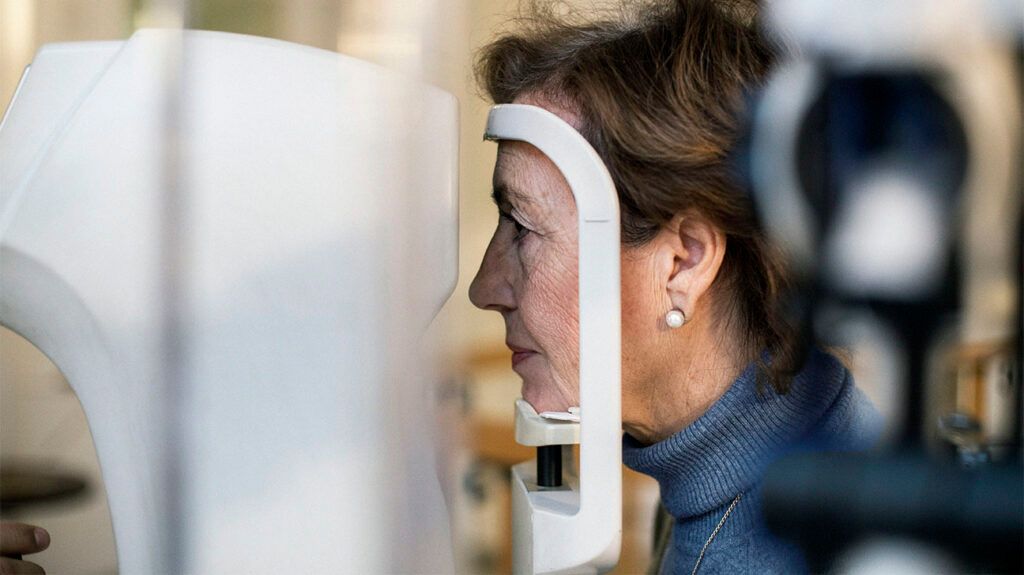
A funduscopic exam is when healthcare professionals use a device called an ophthalmoscope to examine the back of the inner eye. This part of the eye is the fundus, which contains the retina. A dilated funduscopic exam is when they first administer special eye drops into the eyes. These eye drops dilate the pupils, allowing a better look at the fundus.
Other diagnostic tools include ultrasound, CT scans, and MRI scans. For people with a history of retinal detachment, healthcare professionals will generally also examine the individual’s medical history.
Exudative retinal detachment is the result of inflammation. This means that treatment often involves anti-inflammatory medications.
However,
Surgical treatment options for retinal detachment include:
- A vitrectomy: This method involves replacing the gelatinous substance inside the eye.
- Scleral buckling: This involves placing a small band around the eye, which pushes the retina closer to the back of the eye.
- Pneumatic retinopexy: This refers to injecting a gas bubble into the eye, which pushes the retina back.
- Laser surgery or cryosurgery: These techniques involve using lasers or freezing instruments to seal any retinal tears.
It
The following are answers to common questions about retinal detachment.
What are the chances of a second retinal detachment?
After effective treatment for retinal detachment, there may be a
Can a retina detach twice in the same eye?
Yes, the same eye can experience multiple consecutive retinal detachments.
Eye health resources
Visit our dedicated hub for more research-backed information and in-depth resources on eye health.
Retinal detachments occur when the retina pulls apart from the back of the eye. This condition requires immediate treatment, which usually involves surgery.
However, surgical complications can sometimes cause a second retinal detachment. The same is true of injuries and various health conditions. However, surgery remains the main treatment for recurrent retinal detachment.
Secondary, or exudative, retinal attachment occurs due to fluid buildup behind the eye that may be due to an injury, trauma, or another condition. If a person experiences retinal detachment, they need to contact a healthcare professional right away.
