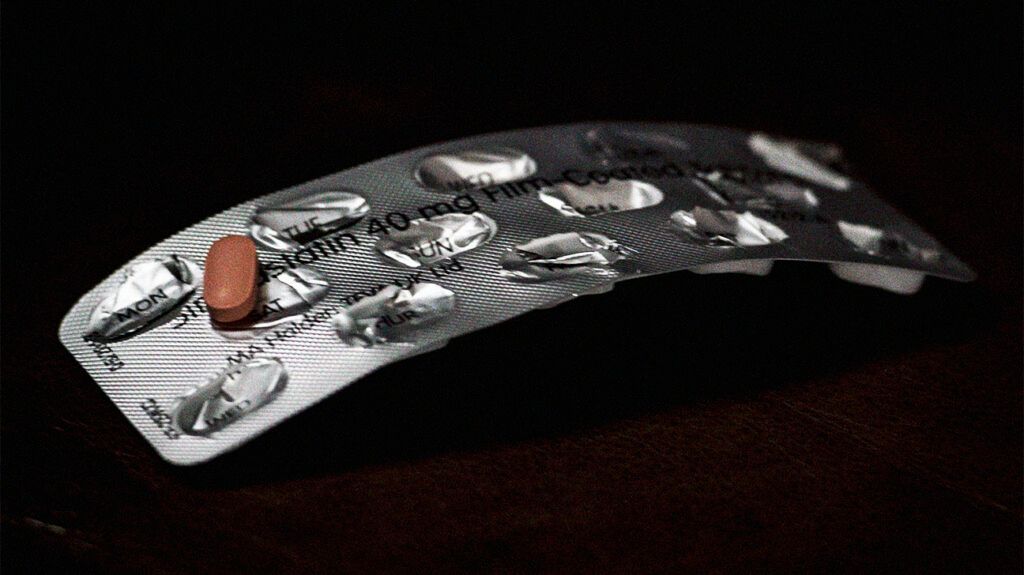
In most cases, taking statins is a lifelong commitment, and ceasing therapy will cause cholesterol levels to return to pre-therapy levels.
It is important to discuss coming off statins with a doctor before attempting to do so. The doctor may recommend lowering the dosage or taking a different medication.
Statins are some of the only cholesterol-lowering drugs that demonstrably
This article explores why a person may want to come off statins and the risks of stopping this type of medication. We also provide a list of alternative treatment options.
Statins reduce LDL cholesterol levels in the blood. LDL cholesterol is a waxy, fatty substance that builds up in the walls of arteries. These deposits restrict blood flow through the arteries and cause inflammation, which increases the risk of heart attack and stroke.
Statins work in
A person may want to come off statins for various reasons, including side effects and a perceived lack of need. However, taking statins is typically a lifelong commitment.
The majority of people who take statins do not experience any side effects. As with all drugs, however, a small minority experience mild to severe side effects when taking statins.
The adverse effects that they most
Muscle problems
In rare cases, people taking statins report muscle pains, tenderness, or weakness. In rare cases, statins may damage the muscles.
If a person taking statins experiences muscle aches, pains, or weakness and cannot link these symptoms to an obvious cause, such as exercise or physical labor, they should speak to a doctor.
A doctor can test a person’s blood creatine kinase (CK) levels. The body releases CK when the muscles are damaged or inflamed. If a person has a high CK level, a doctor may advise stopping statin treatment.
Type 2 diabetes
Hyperglycemia, or increased blood sugar, is a
A
In a person with normal baseline blood glucose levels, statins are highly unlikely to cause diabetes. The benefits of taking statins to prevent a cardiac event usually outweigh the risk of developing diabetes.
Pregnancy
The risk of statins causing pregnancy and birth complications is rare. However,
Exceptions to this include people with pre-established cardiovascular disorders, who may require statin use through pregnancy to ensure their health.
Perceived reduced need
Some lifestyle changes can help people manage their cholesterol levels. Examples include exercising regularly, maintaining a healthy weight, and eating a balanced diet.
However, people who adopt these lifestyle changes should not assume that they can stop taking statins. To determine whether this is the case, a doctor can use blood tests to check that cholesterol levels are within a healthy range.
People who are considering coming off statins should discuss this with their doctors. Stopping statin treatment can be dangerous for certain people, especially those who have a history of stroke, heart attack, or stenting.
A
The study included a total of 45,151 participants. It found that people who quit taking statins 3–6 months after having an IS were 42% more likely to experience a second stroke within 6–18 months.
There was no increased risk for people who continued to take statins at a reduced dose.
Anyone considering coming off statins should first discuss it with their doctor. A medical professional can assess a person’s health and medical history to determine whether reducing or discontinuing statin therapy is safe.
Taking a lower dosage of statins may mean incorporating another cholesterol-lowering drug into the treatment plan. However, this will not always be possible, and in some instances, people will need to take statins for life.
In rare cases, a doctor may suggest stopping statin treatment altogether and replacing it with a different cholesterol-lowering drug. A doctor may prescribe any of the following drugs as an alternative to statins:
PCSK9 inhibitors
PCSK9 is a protein that reduces the liver’s ability to absorb LDL cholesterol from the blood.
PCSK9 inhibitors bind to and inactivate the protein. This allows the liver to absorb more LDL cholesterol and reduce its levels in the blood. Drugs in this class include alirocumab (Praluent) and evolocumab (Repatha).
Selective cholesterol absorption inhibitors
These drugs mainly reduce LDL cholesterol. They may also slightly increase high-density lipoprotein, or “good” cholesterol.
Other treatment options
Other complementary treatment options include lipid-lowering therapies, which reduce levels of triglyceride fats in the blood.
Examples of lipid-lowering drugs and supplements include:
- fibrates, such as gemfibrozil (Lopid), fenofibrate (Tricor), and clofibrate (Atromid-S)
- niacin, which is a form of vitamin B-3
- vascepa, which is a type of omega-3 fatty acid
Statins reduce LDL cholesterol, lowering the risk of heart attack and stroke. There are many reasons that a person may want to come off statins. Some people experience or are concerned about side effects. Others may feel that they no longer need to take this type of drug.
Anyone who wants to stop taking a statin should talk with a doctor. In some cases, coming off these drugs can be dangerous.
The doctor may suggest reducing the dosage, combining the statin with another cholesterol-lowering drug, or switching to another drug entirely.
