- The effects of climate change are known to have potentially negative impacts on health.
- Researchers from the University of California San Francisco are reporting on 10 climate-related hazards that may have a negative impact on eczema.
- The scientists also created maps showing the past, present, and future projected burden of eczema relative to climatic hazards, highlighting areas where research is still needed.
For years, scientists have been studying how the effects caused by climate change may impact health.
Previous studies show climatic effects such as extreme heat can increase a person’s risk for
In addition, air pollution from things such as smog and wildfires can impact the
Many of the effects of climate change also have the potential to lead to
Now, researchers from the University of California San Francisco (UCSF) have found hazards created by climate change can also negatively affect the chronic skin condition atopic dermatitis, also known as eczema.
Their
For this study, researchers focused on how 10 climate hazards related to greenhouse gas emissions impact atopic dermatitis.
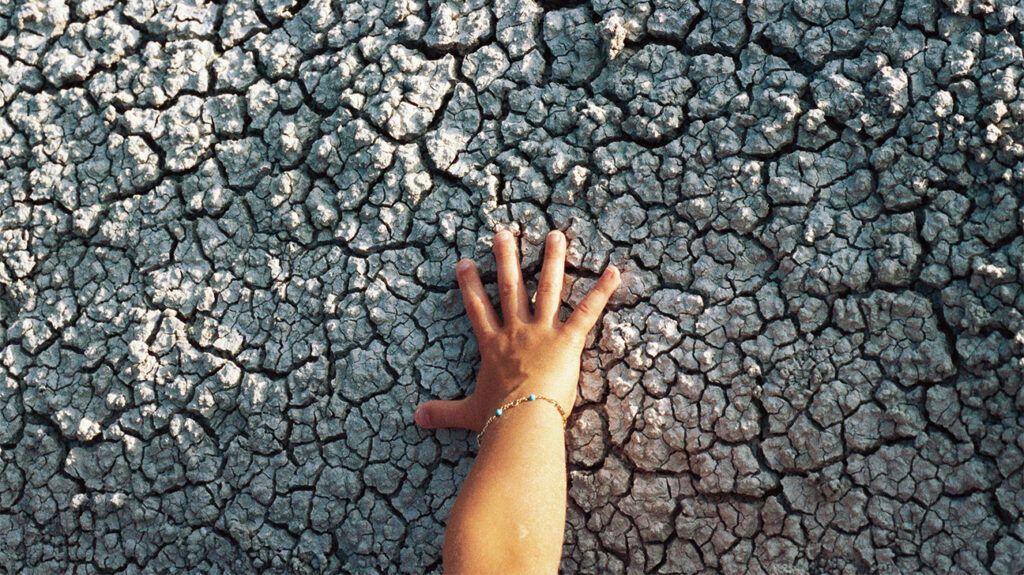
These climate hazards included global warming, heat waves, wildfires, drought, floods, and rising sea levels.
“We’ve known for a long time that atopic dermatitis is particularly sensitive to environmental factors, but there was not a clear consensus on how the increasing prevalence of climatic hazards due to climate change might impact atopic dermatitis. Therefore, we set out to review the literature through a systematic search and provide a narrative summary,” Dr. Katrina Abuabara, an associate professor of dermatology at the UCSF School of Medicine and a senior author of this study, explained to Medical News Today.
“For many patients with atopic dermatitis, the unpredictability of disease flares can be particularly challenging,” Abuabara explained. “Understanding how climatic factors impact disease could lead to better strategies to address disease triggers. Moreover, because atopic dermatitis is so common, it is important from a public health perspective to understand how climate change and climatic hazards could impact disease trends in the population.”
For this study, Abuabara and her team analyzed data from 18 studies providing evidence for the aggravation of eczema by one of the 10 identified climatic hazards.
Overall, researchers said there was evidence linking most climate-related hazards to aggravation of atopic dermatitis.
Some were direct effects, such as particulate matter from wildfires. Others were indirect effects such as drought-induced food insecurity, poverty, and subsequent migration that could disrupt regular healthcare and cause stress that could impact a person’s eczema.
The scientists also created maps showing the past, present, and future projected burden of eczema relative to climatic hazards. Maps were created plotting cumulative exposure to climatic hazards in 2005 and 2017 as well as predictions for 2053.
“The maps from 2005 and 2017 show that there is overlap between geographic areas with more exposure to climatic hazards and increased prevalence of atopic dermatitis,” Abuabara said. “The projections for 2053 were used to illustrate the areas most likely to be impacted in the future, which tend to be more equatorial and do not overlap with countries where most of the existing research has been done, highlighting important areas for future work.”
After reviewing this research, Dr. Jordan Talia, an assistant professor at Mount Sinai Dermatology as well as the director of Complex Medical Dermatology and director of the Skin of Color Center in New York, told Medical News Today that he thought the study was an interesting and helpful summary of existing literature examining the impact of different climatic factors on atopic dermatitis.
“Increased understanding (of how climate change can affect atopic dermatitis) will help doctors and patients take steps to mitigate the impact that certain climatic factors can have on exacerbating atopic dermatitis,” Talia said.
“Atopic dermatitis causes a tremendous amount of suffering, not just for the patient, but often for the whole family,” Dr. Peter Lio, a clinical assistant professor of dermatology and pediatrics at Northwestern University Feinberg School of Medicine in Chicago, explained to Medical News Today: “It is complex and involves the skin barrier, the microbiome — both on the skin and in the gut — the nerve endings, the immune system, and is truly a ‘mind-body’ problem since it causes stress and discomfort.”
“Increased heat, humidity, more variable weather, wildfires, and pollution — all of these can trigger or worsen atopic dermatitis, at least in some individuals,” Lio added. “We all need to work fast to understand how we can push back against these forces to minimize the development and severity of atopic diseases.”
Medical News Today also spoke with Dr. Alexis Young, a dermatologist with Hackensack University Medical Center in New Jersey, who said as a person’s skin is the body’s largest organ and is their first line of defense against the elements, it makes perfect sense that climate change would have an impact.
“Now that we have data supporting the notion that climate-related hazards due to greenhouse gas emissions or particulate matter can have direct effects on eczema, patients can take action to better protect themselves or offset the impacts,” she said. “For example, if we have another summer with heavy smoke drifting from Canadian wildfires, it might be better to stay indoors during these events.”
Dermatology experts provided the following tips for people looking to protect their skin from climatic hazards:
- See a dermatologist for a yearly skin screening.
- Always wear sunscreen and sun-protective clothing, even in the winter.
- Check the air quality before going outside.
- Use moisturizers to help protect the skin from airborne pollutants that can harm the skin barrier.
- Stay hydrated.
- Eat well, get proper sleep, and exercise.
- Wash with gentle cleansers.
- Be mindful of the ingredients in some skin care products that may also lead to unnecessary flare-ups
- Check the National Eczema Association’s database for products suitable for those with eczema and sensitive skin in their Seal of Acceptance program
“Most of all, for those who do have atopic dermatitis, it’s important to find a healthcare practitioner that is experienced and that they have a good relationship with to personalize the recommendations and use medications when needed to keep the skin in its optimal health,” Lio said.