- MindMed, a biotech company specializing in psychedelic-inspired medicines, has revealed promising results from its MM-120 drug candidate in the treatment of Generalized Anxiety Disorder (GAD).
- The results from a recent clinical trial showed that the MM-120 — a hallucinogen better known as LSD — could become a potential new treatment for GAD, a condition that affects millions of people worldwide.
- The trial highlight that the drug candidate, particularly at the 100 µg dose, demonstrated effectiveness, significantly reducing anxiety symptoms.
Generalized anxiety disorder (GAD) is characterized by persistent and excessive worry or nervousness about everyday life, frequently causing disruptions in daily tasks and personal connections.
Potential treatments include psychotherapy, medication, and lifestyle adjustments.
GAD, categorized as an anxiety disorder, is prevalent, affecting 3.1% of the United States population in a given year, equivalent to 6.8 million adults. It is more frequently diagnosed in women.
Coping with anxiety can present difficulties, but like other anxiety disorders, GAD is eminently manageable and responsive to treatment.
Mind Medicine (MindMed) Inc., a clinical-stage biopharmaceutical company specializing in innovative treatments for brain health conditions, has just released promising findings from its Phase 2b clinical trial involving MM-120 (lysergide d-tartrate) for generalized anxiety disorder (GAD).
Dr. Daniel Karlin, chief medical officer of MindMed, explained the key findings to Medical News Today:
“MindMed conducted this study with participation from 198 patients, all of whom suffered with a primary psychiatric diagnosis of generalized anxiety disorder (GAD), across 20 clinical sites in the United States.”
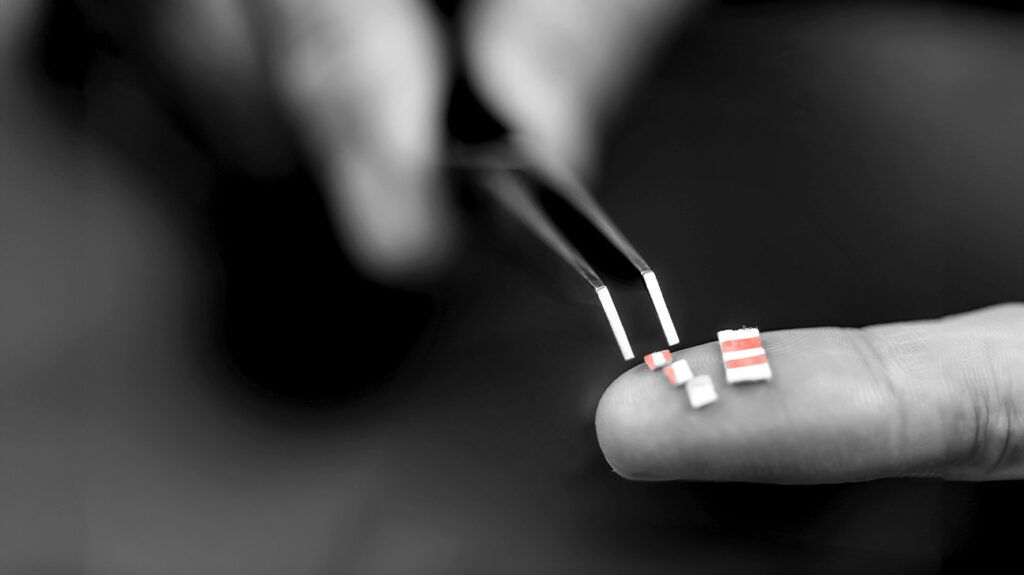
“Participants were divided into 5 study arms; each arm received a single dose of a lysergide-based drug candidate, called MM-120 (lysergide d-tartrate), or a placebo,” Dr. Karlin continued.
“Among the four groups that received a dose of MM-120, doses were 25, 50, 100, or 200 µg of MM-120. Importantly, no form of additional therapy was given to any participant. The study design evaluated the stand-alone effects of the drug candidate, MM-120,” he further explained.
“The data available to us at this time show that patients experienced meaningful and lasting symptom reduction. Four weeks following a single dose of MM-120, 78% of participants who received either a 100 or 200 µg dose measured as having a clinically significant response to the drug. 50% of participants who received the 100 µg dose were considered to be in clinical remission at Week 4, meaning that the patient no longer suffered from clinically significant symptoms of GAD.”
— Dr. Daniel Karlin
The research results have yet to be published in a peer-reviewed journal; however, the company plans to submit the study for publication soon.
Heather Tarbet, Ph.D., vice president of research & development at Amani Ag, told MNT that “this research presents several compelling implications, especially in mitigating the challenges associated with psychedelic therapy.”
“The study demonstrates the tolerability of MM-120, which shortens psychedelic effects while preserving the therapeutic benefits. This approach could alleviate safety and logistical concerns, thereby making psychedelic therapies more accessible and widely accepted among diverse patient groups.”
— Dr. Heather Tarbet
Dr. Tarbet noted that “the study’s insights could inspire progress in the broader field of psychedelic research, potentially enhancing treatments for various complex mental health conditions.”
“Moreover, by altering LSD to lessen its intensity and duration, these treatments could gain broader acceptance among patients, healthcare providers, and regulatory authorities, paving the way for wider adoption in medical practice,” she said.
The preliminary findings from early-phase studies should be corroborated and validated through real-world evidence. This process ensures the reliability and applicability of the trial results.
Dr. Walker Porterfield of Clarity Hyperbarics urged caution about making definitive conclusions, telling MNT that “although on the surface this trial seems to be quite beneficial to patients[experiencing] Generalized Anxiety Disorder (GAD), I see some potential issues.”
Dr. Porterfield highlighted the sample size and trial duration, saying, “the trial was a very small group for a very short duration (198 participants and only four weeks long).”
In addition, Dr. Porterfield noted there was also improvement for patients who were part of the placebo group (31% compared to 78% in the active group).”
Considering this, it’s reasonable to infer that some of the favorable outcomes could be attributed to a placebo-like response. Further studies will need to be completed to assess the actual effectiveness of the medication.
Dr. Karlin told MNT that “MindMed has evaluated the effects of MM-120 in study participants through 12 weeks post-dosing and are currently awaiting those data.”
“We expect to share [more] of that data in the first quarter of 2024. We intend to present the full study results at a scientific conference next year. MindMed also plans to hold an ‘End of Phase 2’ meeting with the FDA in the first half of 2024,” he said.
“Pending the outcome of that meeting, we expect to initiate Phase 3 clinical trials in the second half of 2024,” he added.
“Patients and individuals impacted by GAD largely have been left behind in recent decades; the last approval of a new GAD treatment came in 2004. The most widely prescribed treatments for the disorder often fail to stimulate significant or long-lasting improvement, while exposing patients to side effects that can range from unpleasant to unbearable.”
— Dr. Daniel Karlin
Dr. Karlin explained that “the strong, rapid, and durable clinical activity observed following a single dose of MM-120 is extremely promising for patients who are underserved by current treatment options.”
“The data from this study represents a major step forward in our goal to bring a paradigm-shifting treatment to the millions of people impacted by this debilitating condition,” he said.
