- Hip replacements are common in conditions such as osteoarthritis, and obesity is a well-known risk factor.
- People who have obesity and receive a hip replacement are more likely to experience complications after the procedure than those at a healthy weight.
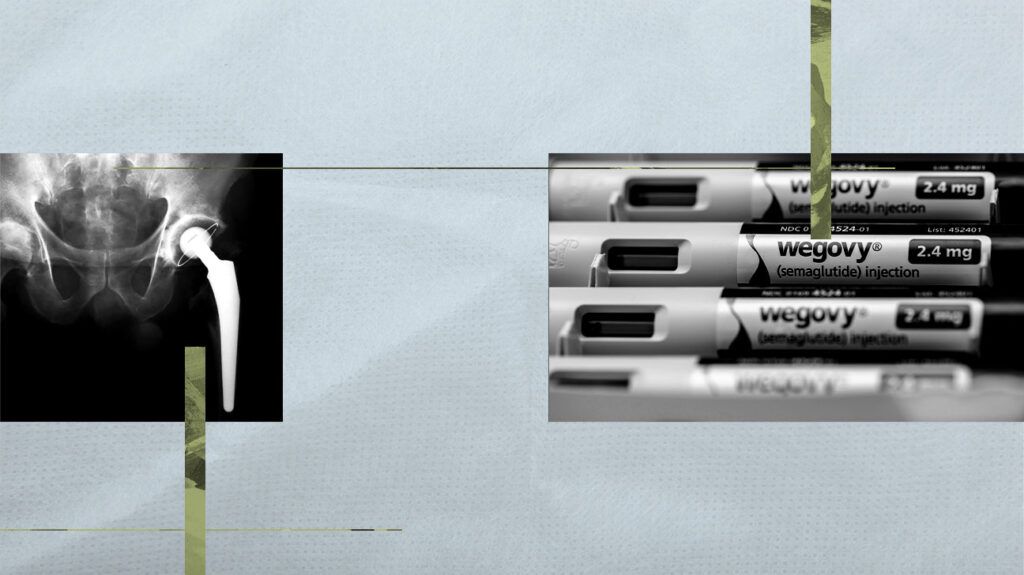
- New research reports people taking semaglutide — the active ingredient in Wegovy and Ozempic — had similar or improved postoperative outcomes after a total hip replacement than those who did not take the drug.
About
People who have osteoarthritis or rheumatoid arthritis may need a total hip replacement, as well as anyone experiencing damage to their hip joint.
As with any surgery, there are some risks of complications. Past studies show that people who have obesity and receive a total hip arthroplasty are more likely to experience complications compared to those who are at a healthy weight.
For this reason, doctors may suggest a person who has obesity lose some weight before having hip replacement surgery.
Now, two studies recently presented at the American Academy of Orthopaedic Surgeons’ 2024 Annual Meeting examine the use of
Researchers reported that people taking semaglutide had similar or improved postoperative outcomes after a total hip replacement to those who did not take the drug.
According to Dr. Matthew L. Magruder, a third-year resident at Maimonides Health in Brooklyn, NY and lead author of one of the presented studies, with the approval of semaglutide for the treatment of obesity by the FDA in 2021, and the surrounding media attention, it was clear that this medication was going to explode in popularity.
“Given that many of our patients undergoing total hip arthroplasty [have obesity], it is inevitable that a growing percentage will be taking it in the perioperative period,” Dr. Magruder explained to Medical News Today.
“Therefore, we figured it would be important to review the data we already had on its effect (on) total hip arthroplasty. It will be increasingly important to understand the effect of this medication on our patients as orthopedic surgeons,” he said.
“In particular, for patients who [have obesity] and in chronic pain due to hip osteoarthritis, it can be very hard to lose weight in order to be indicated for total hip arthroplasty,” added Dr. Daniel Pereira, an orthopedic surgery resident at Washington University Barnes-Jewish Hospital and co-lead author of the second presented study.
“[Having obesity] and [being] in pain makes it much harder to burn calories through traditional means such as exercise or calorie cutting. However, the high risk for complications for [patients with obesity] receiving total hip replacements makes it so that many of these patients do not receive this procedure — for good reason.”
— Dr. Daniel Pereira
“Thus, we need to understand if there were any effects on the outcomes following total hip arthroplasty in patients who took semaglutide when compared to controls,” Dr. Pereira told MNT.
Dr. Pereira’s study examined hip replacement postoperative complications among patients with obesity who used semaglutide compared to those who did not use the medication.
Scientists recruited 616 people in each cohort with an average BMI of 35.5. Upon analysis, the researchers found postoperative complications after a hip replacement — including hip arthroplasty revision, prosthesis infection, and surgical site infections — were similar between people have obesity taking semaglutide compared to those not using the drug.
Dr. Pereira said they were not surprised by these findings.
“We hypothesized that patients who were on semaglutide and received total hip replacements would have the same outcomes, for better or worse, than those who maintained or lost weight by traditional means — we found this to be the case,” he explained.
“The implications are obvious — patients who otherwise would be at a higher risk profile for this surgery can take semaglutide to lose weight and be at a better chance at an equivalent outcome as anyone else. They do not need to receive bariatric surgery or go through other more rigorous means of weight loss in order to be indicated for the procedure,” he added.
Dr. Magruder’s research evaluated whether diabetic patients taking semaglutide at the time of their hip replacement surgery had fewer medical complications, fewer implant-related complications, fewer readmissions, and lower costs than those who were not taking the medication.
Researchers reported people with diabetes taking semaglutide had lower rates of readmission within 90 days of their total hip arthroplasty and lower rates of prosthetic joint infection compared to the control group.
“These findings were not expected but make sense given the medication’s mechanism of action,” Dr. Magruder explained. “Two of its known actions are increasing insulin secretion, thereby decreasing blood glucose levels and slowing gastric emptying, thereby decreasing caloric intake and decreasing weight.”
“Given that poorly controlled diabetes and obesity are independent risk factors for prosthetic joint infection, it makes sense that this medication’s use might decrease its risk after total hip arthroplasty,” he added. “Furthermore, with less prosthetic joint infections, it would follow that there would be fewer readmissions.”
Scientists also found those taking semaglutide did not show statistically significant higher rates of complications compared to those not taking the drug. There was also no difference between the two groups for any other implant-related complication, lengths of stay, same-day surgical costs, or 90-day episode of care costs.
After reviewing these studies, Dr. Timothy Gibson, a board-certified orthopedic surgeon and medical director of the MemorialCare Joint Replacement Center at Orange Coast Medical Center in Fountain Valley, CA, told MNT these findings gave him both feelings of excitement and relief.
“It is reassuring to know that patients with obesity and diabetes who took semaglutide prior to hip replacement surgery do not have higher risks, and in some circumstances have lower risks of complication,” Dr. Gibson continued. “Obesity is a known issue for those undergoing hip replacement surgery. We encourage patients with a very high BMI to lose weight before proceeding with surgery to improve their safety profile.”
“Most, however, are unsuccessful, and often the surgery is never performed,” he added. “This new class of medications may open the door for many more [patients with obesity] to have the opportunity to enjoy the benefits of this typically very successful surgery and to resume a more pain-free and active lifestyle.”
MNT also spoke with Dr. Gregg R. Klein, vice-chair of the Department of Orthopedic Surgery at Hackensack University Medical Center in New Jersey, about these two studies.
Dr. Klein also expressed excitement over these research results.
“Historically, it is well-known that obesity and poor diabetic control have been significant risk factors for patients undergoing total hip replacement,” he detailed. “It has been a challenge for surgeons to optimize a patient with these conditions.”
“The use of semaglutide has become another way that physicians and surgeons can help patients treat obesity and lose weight before surgery. Clinically we have seen patients lose a significant amount of weight using these medications. Hopefully, the weight loss will translate to less complications and better outcomes,” Dr. Klein added.