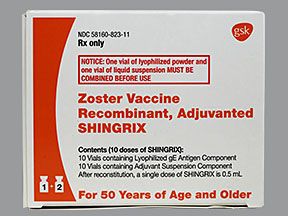
Shingrix is a brand-name vaccine. It helps prevent shingles (herpes zoster).
It’s approved for use in people:
- ages 50 years and older
- ages 18 years and older who have an increased risk of shingles
Shingrix isn’t used to prevent chickenpox (varicella).
Shingrix is given as an intramuscular injection, typically in your upper arm. You’ll receive two separate doses of the vaccine.
A healthcare professional will give you the injections in your doctor’s office or at a pharmacy.
Shingrix is a recombinant vaccine. This means it’s made up of parts of the shingles virus.
To learn more about Shingrix for preventing shingles, see the “Shingrix uses” section. And for more information about how the vaccine works, see “How Shingrix works” below.
FDA approval
The Food and Drug Administration (FDA) approved Shingrix in 2017.
Effectiveness
For information about the effectiveness of Shingrix, see the “Shingrix uses” section below.
Shingrix is available only as a brand-name medication. It’s not currently available in generic form.
Shingrix can cause mild or serious side effects. The following lists contain some of the key side effects that you may have while taking Shingrix. These lists do not include all possible side effects.
For more information on the possible side effects of Shingrix or tips on how to deal with a troubling side effect, talk with your doctor or pharmacist.
More common side effects
The more common side effects of Shingrix can include:
- pain, redness, and swelling at site of injection*
- headache*
- muscle pain
- nausea
- vomiting
- diarrhea
- upset stomach
- dizziness or fainting
- flu-like symptoms, including fever, shivering, and tiredness
Most of these side effects may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk to your doctor or pharmacist.
* For more information about this side effect, see “Side effect details” below.
Serious side effects
Serious side effects from Shingrix aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include the following:
- Severe allergic reaction. See “Side effect details” below for more information.
Note: Since Shingrix was approved for use, there have been reports of Guillain-Barré syndrome in people who’ve had Shingrix. This is a rare condition that causes your immune system to damage your nerves, resulting in muscle weakness.
Side effect details
You may wonder how often certain side effects occur with Shingrix. Here’s some detail on certain side effects this drug may cause.
Injection site reactions
You may have discomfort in the area of your arm where you get Shingrix. Symptoms may include:
- redness
- swelling
- itching
- rash
It’s not known how often these symptoms occur.
Headaches
In some
To find out how often this side effect occurred in clinical studies, see the drug’s
Allergic reaction
As with most drugs, some people can have an allergic reaction after receiving Shingrix. Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (warmth and redness in your skin)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- angioedema (swelling under your skin, typically in your eyelids, lips, hands, or feet)
- swelling of your tongue, mouth, or throat
- trouble breathing
- low blood pressure
Call your doctor right away if you have a severe allergic reaction to Shingrix. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
As with all medications, the cost of Shingrix can vary.
The actual price you’ll pay depends on your insurance coverage and the pharmacy you use.
Financial and insurance assistance
If you need financial support to pay for Shingrix, help is available.
GlaxoSmithKline Biologicals, the manufacturer of Shingrix, offers a program called GSKforyou. For more information and to find out if you’re eligible for support, call 866-728-4368 or visit the program website.
A live vaccine is one that contains a weakened form of a germ. Shingrix is not a live vaccine. It’s an inactive vaccine, which is a vaccine that’s made from a germ that’s been killed.
Because Shingrix is inactive, more people can receive it. This includes people with a weakened immune system (the body’s defense against disease).
People with weakened immune systems are typically advised against receiving live vaccines. This is because on very rare occasions, live vaccines can mutate (change) back to the full-strength germ that causes a disease.
If this happens, people with weakened immune systems would have a much higher risk for developing the disease that the vaccine is meant to prevent.
Shingrix is also a recombinant vaccine. This means that it’s made of parts of the shingles virus, such as protein, sugar, or capsid (a casing around the germ).
There used to be an alternative shingles vaccine to Shingrix. This other vaccine was called Zostavax.
Like Shingrix, it was approved to prevent shingles (herpes zoster). However, Zostavax is
Like Shingrix, Zostavax was a vaccine used to help prevent shingles (herpes zoster). However, Zostavax is
Below, we briefly describe the similarities and differences between these two vaccines.
Uses
Shingrix is approved for use in people:
- ages 50 years and older
- ages 18 years and older who have an increased risk of shingles
Zostavax, on the other hand, was only approved for use in people ages 50 years and older.
Neither vaccine has been approved for preventing chickenpox (varicella). They also haven’t been approved for treating shingles or postherpetic neuralgia, a complication of shingles that causes burning pain.
Live shingles vaccine vs. non-live shingles vaccine
A live vaccine is one that contains a weakened form of a germ. Shingrix is not a live vaccine. It’s an inactive vaccine, which is a vaccine that’s made from a germ that’s been killed.
Because Shingrix is inactive, more people can receive it. This includes people with a weakened immune system (the body’s defense against disease).
Zostavax was a shingles vaccine that was live.
People with weakened immune systems are typically advised against receiving live vaccines. This is because on very rare occasions, live vaccines can mutate (change) back to the full-strength germ that causes a disease. If this happens, people with weakened immune systems would have a much higher risk for developing the disease that the vaccine is meant to prevent.
CDC recommendation for the shingles vaccine
The CDC found that Shingrix was more effective than Zostavax. It recommends that you receive Shingrix, even if you’ve had Zostavax in the past.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to suit your needs.
Drug forms and strengths
Shingrix is given as an intramuscular injection, typically in your upper arm. You’ll receive two separate doses of the vaccine. Each dose contains 0.5 mL of vaccine solution.
A healthcare professional will give you the injections in your doctor’s office or at a pharmacy.
Dosage for shingles prevention
Shingrix is given as two 0.5-mL injections in your upper arm. You’ll receive two doses of this vaccine.
Over time, some vaccines’ protection begins to fade, so may you need booster doses. They help keep the vaccine working. But you don’t need a booster dose after getting the two doses of Shingrix.
Shingrix dosing schedule for people ages 50 years and older
For people ages 50 years and older taking Shingrix, the second dose is given 2 to 6 months after the first dose.
Shingrix dosing schedule for people ages 18 years and older with an increased risk of shingles
For people ages 18 years and older with an increased risk of shingles who are taking Shingrix, the second dose may be given 1 to 2 months after the first dose.
What if I wait too long to take the second Shingrix dose?
Also, if you get the second dose within 4 weeks after the first dose, it should not be counted. You should get your follow-up dose at least 1 to 2 months after the first dose, per your doctor’s recommendation.
There aren’t any specific warnings or guidelines about alcohol and Shingrix. If you have concerns about drinking alcohol and getting the Shingrix vaccine, talk with your doctor.
Shingrix can interact with several other medications.
Different interactions can cause different effects. For instance, some interactions can affect how well a drug works, while others can cause increased side effects.
Shingrix and other medications
Below are medications that can interact with Shingrix. These are not all the drugs that may interact with Shingrix.
Before taking Shingrix, be sure to tell your doctor and pharmacist about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Immunosuppressive drugs such as prednisone
Taking Shingrix with drugs that suppress your immune system can cause problems with the way your body responds to Shingrix. Examples of immunosuppressive medications include:
- corticosteroids, such as:
- prednisone (Deltasone)
- budesonide (Pulmicort)
- monoclonal antibodies, such as:
- adalimumab (Humira)
- etanercept (Enbrel)
- rituximab (Rituxan)
- other medications, such as:
- azathioprine (Azasan, Imuran)
- cyclosporine (Neoral, Sandimmune)
- methotrexate (Otrexup, Rasuvo, Rheumatrex, Trexall)
- mycophenolate (CellCept, Myfortic)
- tacrolimus (Astagraf XL, Envarsus XR, Prograf)
- sirolimus (Rapamune)
- tofacitinib (Xeljanz)
If you take any of these medications, talk with your doctor or pharmacist before getting Shingrix.
Shingrix and other vaccines
Shingrix is generally safe to use with or after administration of certain other vaccines. If you have concerns about whether other vaccines might interact with Shingrix, ask your doctor.
Shingrix after Zostavax
There used to be another shingles (herpes zoster) vaccine called Zostavax. Like Shingrix, it was approved to prevent shingles.
However, Zostavax is
If you’ve had Zostavax in the past, you should still receive Shingrix, according to
Shingrix and the flu shot
There is no evidence showing any negative effects from taking Shingrix together with the flu vaccine. According to a
Here are answers to some frequently asked questions about Shingrix.
Can I get the Shingrix vaccine if I have an egg allergy?
Yes. It’s safe for you to get the Shingrix vaccine if you’re allergic to eggs. Shingrix doesn’t contain any egg protein. But certain flu vaccines may contain egg protein.
If you have an egg allergy, be sure to tell your doctor before getting any vaccines.
I’m living with HIV. Is it safe for me to get Shingrix?
The Centers for Disease Control and Prevention (CDC) hasn’t made a recommendation about the use of Shingrix in people living with HIV.
However, one study looked at healthy adults ages 18 and older who were living with HIV and had an HIV dosing schedule that was customized to their needs. These people received the Shingrix vaccine, and the study results did not report any safety issues.
If you’re living with HIV, talk with your doctor about the risks and benefits of getting Shingrix.
What’s the age range for getting the Shingrix vaccine?
Shingrix is approved for use people:
- ages 50 years and older
- ages 18 years and older who have an increased risk of shingles
There’s no upper age limit for getting Shingrix, so there isn’t a set age range.
How safe is Shingrix?
The FDA has approved Shingrix for preventing shingles (herpes zoster) in adults. The results of several
There have been concerns about ingredients, such as thimerosal, that may be added to vaccines. Thimerosal is a kind of preservative that contains mercury. It’s added then taken out of some vaccines to keep other germs and bacteria from growing. The concern arose when early research connected thimerosal to autism. This link has since been found to be false. Shingrix doesn’t contain thimerosal.
Can I receive Shingrix if I have shingles or if I had shingles in the past?
The
If you’ve have had shingles in the past, you can take Shingrix. It may help prevent future shingles infections.
Can I get Shingrix if I’ve never had chickenpox?
If you’ve never had chickenpox (varicella), the
If you can’t recall whether you’ve had chickenpox, you may need to be screened for it. But this will depend on your age.
It’s assumed that people born in the United States and elsewhere before 1980 have been exposed to chickenpox. Therefore, you may be able to receive Shingrix. You should check with your doctor first to make sure.
Can Shingrix cause a rash?
It’s unlikely that a Shingrix injection will cause a rash. But note that an injection site reaction is different from a shingles rash. (See “Injection site reactions” in the “Shingrix side effects” section above.)
A shingles rash, which is caused by shingles itself, is often painful. It commonly appears as blisters around the torso, neck, or face.
People who received Shingrix in
However,
The Food and Drug Administration (FDA) approves vaccines such as Shingrix to prevent certain conditions.
Shingrix for prevention of shingles
Shingrix is a vaccine that’s used to prevent shingles (herpes zoster). It’s approved for use in people:
- ages 50 years and older
- ages 18 years and older who have an increased risk of shingles
People with an increased risk of shingles include those with a weakened immune system, such as people with HIV.
Shingrix is not meant for use in preventing chickenpox (varicella).
Effectiveness for prevention of shingles
Shingrix has been found to be effective in helping to prevent shingles. For details on how the drug performed in clinical studies, see Shingrix’s
- all adults ages 50 years and older
- adults ages 18 to 50 years with a weakened immune system
Your body responds to germs by making antibodies. These are proteins that fight off specific germs. Antibodies also help prevent future infections by remembering the germs so they can fight them off more quickly.
Vaccines are made from germs, or pieces of germs, that help your body imitate an actual disease. This prompts your body to create antibodies.
Shingrix introduces proteins from the shingles (herpes zoster) virus to your body. Your body responds by protecting itself from infection by the shingles virus. This is called an immune response.
How long does it take to work?
It takes time for your body to make enough antibodies to fight off germs and protect you from certain diseases.
Results from
How long Shingrix takes to work may not be the same for everyone. The timing for you will depend on your body chemistry. In general, you should be protected from shingles soon after the second dose.
There haven’t been any studies in humans to know if it’s safe to get the Shingrix vaccine when you’re pregnant.
If you’re pregnant or planning to become pregnant, wait until after you’ve had your baby to get the Shingrix vaccine. Talk with your doctor if you have any concerns.
There haven’t been enough studies to show whether Shingrix appears in breast milk.
Until more is known, it’s best to wait until you’ve finished breastfeeding before getting Shingrix.
Before receiving Shingrix, talk with your doctor about your health history. Shingrix may not be right for you if you have certain medical conditions. These include:
- Allergic reactions to vaccines. People who have had allergic reactions to vaccines in the past may be at risk again for an allergic reaction to Shingrix. If you have had an allergic reaction to vaccines before, talk with your doctor and have them review your immunization history. You may need additional treatment and supervision to receive Shingrix.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up-to-date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.