Plegridy is a brand-name prescription drug. It’s approved for certain uses in adults with multiple sclerosis (MS).
MS may cause symptoms such as trouble walking or vision changes. It can also cause numbness or tingling in your arms, legs, or other areas of your body.
Specifically, Plegridy is approved to treat MS symptoms caused by the following conditions:
- Clinically isolated syndrome (CIS). With CIS, you have a first episode of MS-like symptoms that lasts at least 24 hours. The episode is caused by inflammation or demyelination (loss of the protective covering on your nerve cells). CIS may or may not lead to the development of MS.
- Relapsing-remitting MS. With this form of MS, you have relapses (flare-ups) of MS symptoms, followed by periods of remission (when your disease doesn’t worsen).
- Active secondary progressive disease. With this form of MS, your MS symptoms continually get worse, and you don’t have any periods of remission.
Plegridy contains the active drug peginterferon beta-1a. It belongs to a class of medications called interferon betas.
Interferons are proteins that are naturally made in your body. They work to decrease your immune response and to reduce inflammation. Because it affects how your immune system works, Plegridy is also called an immunomodulator.
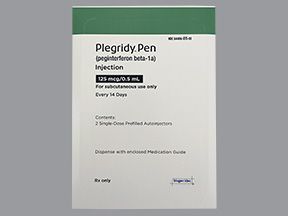
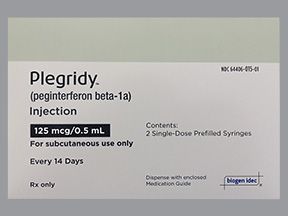
Plegridy comes as a liquid solution in prefilled, single-dose syringes and pens. It’s given as an injection under your skin (called a subcutaneous injection). Your doctor will show you how to administer Plegridy injections to yourself. This medication is typically given every couple of weeks.
Effectiveness
In a clinical trial, Plegridy was shown to be effective in treating MS and preventing the condition from getting worse. In the trial, people were considered to have a relapse of their MS when they had an increased level of disability caused by the condition. Their level of disability was assessed using test scores from the Expanded Disability Status Scale (EDSS).
The study showed that over 48 weeks of treatment, people taking Plegridy were 36% less likely to have a relapse of their MS than were people taking a placebo (no active drug).
Also, in this study, Plegridy decreased the number of people who had a relapse of their MS. For example, of people taking Plegridy, 18.7% had a relapse within 48 weeks of treatment. In comparison, 29.1% of people taking a placebo had a relapse within the same period of time.
Plegridy is available only as a brand-name medication. It’s not currently available in generic form. A generic drug is an exact copy of the active drug in a brand-name medication.
Plegridy contains the active drug peginterferon beta-1a.
Plegridy can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Plegridy. These lists don’t include all possible side effects.
For more information on the possible side effects of Plegridy, talk with your doctor or pharmacist. They can give you tips on how to deal with any side effects that may be bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs they’ve approved. If you would like to report to the FDA a side effect you’ve had with Plegridy, you can do so through MedWatch.
Mild side effects
The mild side effects of Plegridy that are more common* can include:
- redness, pain, or itching at your injection site
- flu-like symptoms, such as headache or fever
- muscle pain
- chills
- weakness
- joint pain
The mild side effects of Plegridy that are less common** can include:
- nausea
- vomiting
- swelling or warmth at your injection site
* occurred in 10% or more of people in clinical studies
** occurred in less than 10% of people in clinical studies
Most of these side effects may go away within a few days or a couple of weeks. But if they become more severe or don’t go away, talk with your doctor or pharmacist.
Serious side effects
Serious side effects from Plegridy aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include:
- Liver injury, such as hepatitis (inflammation in your liver). Symptoms can include:
- jaundice (yellowing of your skin or the whites of your eyes)
- dark colored urine
- belly pain
- weight gain
- Depression. Symptoms can include:
- feeling hopeless
- feeling nervous or upset
- having weight loss or weight gain
- Thoughts of suicide. Symptoms can include:
- having thoughts of harming yourself
- Seizures. Symptoms can include:
- moving your arms and legs uncontrollably
- losing consciousness
- feeling confused or not being able to remember things
- Serious reactions, such as necrosis (cell death), at the site of your injections. Symptoms can include:
- pain in area of your injection
- dark purple or black colored skin in the area of your injection site
- peeling skin at the area of your injection
- Congestive heart failure. Symptoms can include:
- trouble breathing
- swelling in your arms or legs
- fatigue (lack of energy)
- weight gain
- Decreased level of either white blood cells or platelets (cells that help your blood to clot). Symptoms can include:
- fever
- taking longer to recover from an infection than usual
- cough
- bleeding more easily than usual
- Autoimmune diseases, such as increased or decreased thyroid function. Symptoms can include:
- increased heart rate
- weight loss or weight gain
- lump in your neck
- fatigue (lack of energy)
- feeling cold
- Thrombotic microangiopathy (a condition that causes blood clots inside your small blood vessels). Symptoms can include:
- confusion
- swelling in your legs
- increased blood pressure
- dizziness
- Severe allergic reaction, which is explained in more detail below in “Side effect details.”
Side effect details
You may wonder how often certain side effects occur with this drug, or whether certain side effects pertain to it. Here’s some detail on some of the side effects this drug may or may not cause.
Allergic reaction
As with most drugs, some people can have an allergic reaction after taking Plegridy. Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (warmth and redness in your skin)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
- hives
In one clinical trial, less than 1% of people taking Plegridy had a serious allergic reaction to the drug. Everyone in the trial who had an allergic reaction to Plegridy responded well to treatment with certain medications. These medications included steroids, such as prednisone, and antihistamines, such as diphenhydramine (Benadryl).
Call your doctor right away if you have a severe allergic reaction to Plegridy. But call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Depression
While you’re taking Plegridy, it’s possible to become depressed. With depression, you may feel hopeless, anxious, or have trouble concentrating. You may also not want to do things that used to excite you.
People taking Plegridy also have an increased risk for suicide and thoughts of suicide. In fact, anyone using an interferon beta injection (which is the type of drug that Plegridy is) may have an increased risk for depression or thoughts of suicide.
However, in clinical trials, people taking Plegridy didn’t have an increased risk for depression or thoughts of suicide.
About 8% of people taking either Plegridy or a placebo (no active drug) had depression or thoughts of suicide. And less than 1% of people taking either Plegridy or a placebo had serious depression or suicidal thoughts or actions.
If you feel depressed or have thoughts of suicide, it’s important that you call your doctor as soon as possible. If you can’t talk with your doctor, but you need help right away, call 911.
Suicide prevention
If you know someone at immediate risk of self-harm, suicide, or hurting another person:
- Ask the tough question: “Are you considering suicide?”
- Listen to the person without judgment.
- Call 911 or the local emergency number, or text TALK to 741741 to communicate with a trained crisis counselor.
- Stay with the person until professional help arrives.
- Try to remove any weapons, medications, or other potentially harmful objects.
If you or someone you know is having thoughts of suicide, a prevention hotline can help. The 988 Suicide and Crisis Lifeline is available 24 hours a day at 988. During a crisis, people who are hard of hearing can use their preferred relay service or dial 711 then 988.
Weight loss or weight gain
Changes in weight weren’t reported as side effects in people using Plegridy during clinical trials. However, weight loss or weight gain can be a side effect of other medications that you may be taking for multiple sclerosis (MS) treatment. For example, some other medications used to treat MS, such as steroids, can cause weight gain.
It’s also possible that MS itself can cause changes in your weight. With MS, you may feel tired or have pain, which can make it hard for you to exercise. For some people, this may lead to weight gain. The condition may also limit how well you’re able to move your body, which can cause your muscle mass to decrease. This may lead to weight loss.
Weight changes may also occur during Plegridy treatment due to other side effects of the drug. For example, if Plegridy causes an increase or decrease in your thyroid function, you may have weight loss or weight gain.
Depression, which is another possible side effect of Plegridy, may also cause weight changes in some people. Sometimes, if you’re depressed, you may not feel like eating. This can lead to weight loss. But other times, depression may cause you to eat more food, which may lead to weight gain.
In addition, liver damage and congestive heart failure are other possible side effects of Plegridy that may cause weight gain.
Although weight loss and weight gain haven’t been directly caused by Plegridy, it’s possible to have changes in your weight during treatment with the drug. If you notice a change in your weight while you’re taking Plegridy, talk with your doctor. They can help you manage a body weight that’s healthy for you.
Injection site reactions
You may have a reaction to Plegridy in the area where you inject the drug into your body. These reactions are called injection site reactions. They can cause redness, pain, swelling, or itching in the affected area.
In people taking Plegridy during clinical trials, about 66% had an injection site reaction. Of people using a placebo injection (no active drug), 11% had a reaction.
Sometimes, injection site reactions may be severe. These severe reactions can cause severe swelling or pain. Necrosis (cell death) can also occur in severe cases. (With necrosis, the area affected may appear black or purple in color.)
In clinical trials, 3% of people taking Plegridy had a severe injection site reaction. No one using a placebo injection had a severe reaction. Out of 1,468 people taking Plegridy, only 1 person developed necrosis at their injection site. No one using the placebo injection had necrosis.
If you have symptoms of an injection site reaction, talk with your doctor. They can recommend ways to decrease your symptoms.
But if you notice that the area around your injection becomes very painful or swollen, or looks dark purple or black, see your doctor as soon as possible. These changes may indicate a more serious injection site reaction that needs treatment right away.
Flu-like symptoms
It’s possible to have flu-like symptoms when you’re taking Plegridy. Examples of flu-like symptoms include headache, muscle aches, fever, chills, fatigue (lack of energy), and joint pain.
Most often, flu-like symptoms occur when you first start using Plegridy. However, once you’ve been taking the drug for a while, your flu-like symptoms may decrease or go away completely.
It’s important to note that if you do have flu-like symptoms while you’re taking Plegridy, the symptoms are probably not caused by the flu (influenza). While influenza is a viral infection that can be passed to other people, flu-like symptoms caused by Plegridy aren’t contagious. This means that you can’t pass the symptoms caused by Plegridy to other people and make them sick.
In one clinical trial, 47% of people taking Plegridy had flu-like symptoms. In comparison, only 13% of people using a placebo injection (no active drug) had flu-like symptoms.
If you have flu-like symptoms while you’re taking Plegridy, talk with your doctor. They’ll help make sure that the cause of your symptoms isn’t the influenza virus.And they’ll be able to recommend ways to reduce your symptoms, such as by having you take fever reducers or pain relievers.
How long do Plegridy side effects last?
Side effects from Plegridy are often mild and usually go away over time. As you continue taking Plegridy, your side effects may decrease with each dose. But it’s not known exactly how long your side effects will last. And each person using the drug may react differently to Plegridy.
If you’re concerned about how long you may have certain side effects of Plegridy, talk with your doctor.
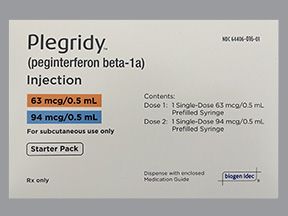
The Plegridy dosage your doctor prescribes to treat your multiple sclerosis (MS) will depend on several factors. These include how long you’ve been taking Plegridy and any other medical conditions you may have.
Typically, your doctor will start you on a low dosage. Then they’ll adjust it over time to reach the amount that’s right for you. Your doctor will ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to fit your needs.
Drug forms and strengths
Plegridy comes as a liquid solution that’s given as an injection under your skin (called a subcutaneous injection). It’s available in prefilled, single-dose syringes and pens. Plegridy comes in a 63-mcg, 94-mcg, or 125-mcg doses.
Your doctor will teach you how to self-inject your Plegridy doses. This medication can be injected into your belly area, the back of your arms, and your thighs. For each dose of the drug, you should change injection sites and rotate between these areas.
Dosage for MS
The typical dosage of Plegridy for MS is started low and slowly increased over time. Adjusting your dosage like this is called “titration.” It’s done to decrease the side effects that you may have when you’re starting Plegridy therapy.
Generally, Plegridy dosing is as follows:
- your first dose is 63 mcg
- 14 days later, you’ll receive a second dose of 94 mcg
- 14 days after your second dose, you’ll receive a third dose of 125 mcg
- after your third dose, you’ll continue to receive 125-mcg doses every 14 days
Note: If you have side effects from Plegridy such as fever, injection site pain, or headache, your doctor may recommend that you take another medication before taking your dose of Plegridy. Doing this may help reduce your side effects of Plegridy. For more information about this, see the section below called “Plegridy use with other drugs.”
What if I miss a dose?
If you forget to take your dose of Plegridy, take the missed dose as soon as you remember. But if it’s within a few days before your next scheduled dose, talk with your doctor or pharmacist about the best time to take your dose.
Never take more than one dose of Plegridy within a 7-day period to make up for a missed dose.
To help make sure that you don’t miss a dose, try setting a reminder in your phone. A medication timer may be useful, too.
Will I need to use this drug long-term?
Plegridy is meant to be used as a long-term treatment. In a clinical trial, over the course of 48 weeks, Plegridy reduced people’s risk of MS relapse by 36%. (In the trial, people were considered to have a relapse of their MS when they had an increased level of disability caused by the condition.)
If you and your doctor determine that Plegridy is safe and effective for you, you’ll likely take it long-term.
The Food and Drug Administration (FDA) approves prescription drugs such as Plegridy to treat certain conditions. Plegridy may also be used off-label for other conditions. Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.
Plegridy is FDA-approved for certain uses in adults with multiple sclerosis (MS). With MS, your immune system attacks the tissue around your nerves that’s called the myelin sheath. This can cause problems with how well the cells inside your brain and spinal cord can communication with each other.
MS may cause symptoms such as trouble walking or vision changes. It may also cause numbness or tingling in your arms, legs, or other areas of your body. However, MS affects each person differently, so these typical symptoms can differ greatly from person to person.
Specifically, Plegridy is approved to treat MS symptoms in the following situations:
- Clinically isolated syndrome (CIS). With CIS, you have a first episode of MS-like symptoms that lasts at least 24 hours. The episode is caused by inflammation or demyelination (loss of the protective covering on your nerve cells). CIS may or may not lead to the development of MS.
- Relapsing-remitting MS. With this form of MS, you have flare-ups of MS symptoms (called relapses), followed by a period of time in which your disease doesn’t worsen (called remission).
- Active secondary progressive disease. With this form of MS, your MS symptoms continually get worse, and you don’t have any periods of remission.
Plegridy is
Effectiveness for MS
In one clinical trial, Plegridy was shown to be effective in treating MS and preventing the condition from getting worse. In the trial, people were considered to have a relapse of their MS when they had an increased level of disability caused by the condition. Their level of disability was assessed using test scores from the Expanded Disability Status Scale (EDSS).
The study showed that over 48 weeks of treatment, people taking Plegridy were 36% less likely to have a relapse of their MS than were people taking a placebo (no active drug).
Also, in the study, Plegridy decreased the number of people who had a relapse of their MS. For example, of people taking Plegridy, 18.7% had a relapse within 48 weeks of treatment. In comparison, 29.1% of people taking a placebo had a relapse within the same period of time.
Plegridy use in children (under study)
Plegridy is only approved for use in adults. The drug hasn’t been studied in children, so it’s not known if Plegridy is safe or effective people younger than 18 years of age. However, a clinical trial is currently being done to see whether Plegridy can be used in children with relapsing-remitting MS.
Plegridy may cause bothersome side effects including flu-like symptoms, such as headache or fever. The drug can also cause injection site reactions, which cause pain or redness in the area of your injection.
Sometimes, your doctor may recommend that you take medications before taking your Plegridy dose to help prevent these side effects. Medications that may be recommended include fever reducers, such as acetaminophen (Tylenol) or pain relievers, such as ibuprofen (Advil, Motrin).
If you have questions about whether you need to take other drugs with Plegridy, talk with your doctor.
Other drugs are available that can treat multiple sclerosis (MS). Some may be a better fit for you than others. If you’re interested in finding an alternative to Plegridy, talk with your doctor. They can tell you about other medications that may work well for you.
Note: Some of the drugs listed below are used off-label to treat these specific conditions. Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.
Examples of drugs that may be used to treat relapsing forms of MS include:
You may wonder how Plegridy compares with other medications that are prescribed for similar uses. Here we look at how Plegridy and Avonex are alike and different.
Ingredients
Plegridy contains the active drug peginterferon beta-1a, while Avonex contains the active drug interferon beta-1a.
The difference between these two drugs is that the interferon contained in Plegridy is “pegylated.” (Pegylated interferons have a different chemical structure than non-pegylated interferons do).
Because Plegridy is pegylated, it stays in your body over a longer period of time. This means you don’t have to take doses of Plegridy as often as you’d have to take doses of certain other drugs.
Uses
Both Plegridy and Avonex have the same FDA-approved uses. Both drugs are approved to treat multiple sclerosis (MS) symptoms in the following situations:
- Clinically isolated syndrome (CIS). With CIS, you have a first episode of MS-like symptoms that lasts at least 24 hours. The episode is caused by inflammation or demyelination (loss of the protective covering on your nerve cells). CIS may or may not lead to the development of MS.
- Relapsing-remitting MS. With this form of MS, you have flare-ups of MS symptoms (called relapses), followed by a period of time in which your disease doesn’t worsen (called remission).
- Active secondary progressive disease. With this form of MS, your MS symptoms continually get worse, and you don’t have any periods of remission.
Drug forms and administration
Plegridy comes as a liquid solution inside prefilled, single-dose pens and syringes. It’s given as an injection under your skin (called a subcutaneous injection). And it’s taken once every 2 weeks.
Avonex comes as a powder that must be mixed with liquid to form a solution. In addition, it’s available in prefilled, single-dose syringes and autoinjectors that hold liquid solution of the drug. Avonex is given by injection into your muscle (called an intramuscular injection). And it’s taken once every week.
Both Plegridy and Avonex can be self-injected after your doctor has shown you how to administer the drug to yourself.
Side effects and risks
Plegridy and Avonex both contain interferon beta-1a. Therefore, these medications can cause very similar side effects. Below are examples of these side effects.
Mild side effects
These lists contain examples of mild side effects that can occur with Plegridy, with Avonex, or with both drugs (when taken individually).
- Can occur with Plegridy:
- vomiting
- Can occur with Avonex:
- few unique mild side effects
- Can occur with both Plegridy and Avonex:
- flu-like symptoms, such as headache or fever
- redness, pain, swelling, warmth, or itching at your injection site
- chills
- muscle pain
- weakness
- joint pain
- nausea
Serious side effects
These lists contain examples of serious side effects that can occur with Plegridy, with Avonex, or with both drugs (when taken individually).
- Can occur with Plegridy:
- serious injection site reactions, such as necrosis (death of cells) in the area of your injection
- Can occur with Avonex:
- mental health disorders, such as psychosis (a condition where you lose contact with reality) and schizophrenia (a condition where you may have hallucinations or delusions)
- Can occur with both Plegridy and Avonex
- depression and suicide
- liver injury, such as hepatitis (inflammation in your liver)
- severe allergic reaction
- thrombotic microangiopathy (a condition that causes blood clots in your small blood vessels)
- autoimmune diseases, such as increased or decreased thyroid function
Effectiveness
The only conditions both Plegridy and Avonex are used to treat certain forms of relapsing-remitting multiple sclerosis (MS).
These drugs haven’t been directly compared in clinical studies. But separate studies have found both Plegridy and Avonex to be effective in treating MS.
There’s currently a study being done that’s looking at using both Plegridy and Avonex in children with relapsing-remitting MS, but the study results haven’t been published yet. At this time, neither drug is approved for use in children with this condition.
Costs
Plegridy and Avonex are both brand-name drugs. There are currently no generic forms of either drug. Brand-name medications usually cost more than generics.
The actual price you’ll pay for either drug will depend on your insurance plan, your location, and the pharmacy you use.
You may wonder how Plegridy compares with other medications that are prescribed for similar uses. Here we look at how Plegridy and Tecfidera are alike and different.
Ingredients
Plegridy contains the active drug peginterferon beta-1a, while Tecfidera contains the active drug dimethyl fumarate.
Uses
Both Plegridy and Tecfidera have the same FDA approved uses. Both drugs are approved to treat multiple sclerosis (MS) symptoms in the following situations:
- Clinically isolated syndrome (CIS). With CIS, you have a first episode of MS-like symptoms that lasts at least 24 hours. The episode is caused by inflammation or demyelination (loss of the protective covering on your nerve cells). CIS may or may not lead to the development of MS.
- Relapsing-remitting MS. With this form of MS, you have flare-ups of MS symptoms (called relapses), followed by a period of time in which your disease doesn’t worsen (called remission).
- Active secondary progressive disease. With this form of MS, your MS symptoms continually get worse, and you don’t have any periods of remission.
Drug forms and administration
Plegridy comes as a liquid solution inside prefilled, single-dose pens and syringes. It’s given as an injection under your skin (called a subcutaneous injection). And it’s taken once every 2 weeks. Plegridy can be self-injected after your doctor has shown you how to administer the drug to yourself.
On the other hand, Tecfidera comes as capsules that are taken by mouth. It’s usually taken twice daily.
Side effects and risks
Plegridy and Tecfidera both contain drugs that are used to treat MS. Therefore, these medications can cause very similar side effects. Below are examples of these side effects.
Mild side effects
These lists contain examples of mild side effects that can occur with Plegridy, with Tecfidera, or with both drugs (when taken individually).
- Can occur with Plegridy:
- redness, pain, swelling, warmth, or itching at your injection site
- flu-like symptoms, such as headache or fever
- muscle pain
- chills
- weakness
- joint pain
- Can occur with Tecfidera:
- itching, rash, or flushing (redness) on your skin
- belly pain
- diarrhea
- indigestion
- Can occur with both Plegridy and Tecfidera:
- nausea
- vomiting
Serious side effects
These lists contain examples of serious side effects that can occur with Plegridy, with Tecfidera, or with both drugs (when taken individually).
- Can occur with Plegridy:
- depression and suicide
- serious injection site reactions, such as necrosis (death of cells) in the area of your injection
- autoimmune diseases, such as increased or decreased thyroid function
- thrombotic microangiopathy (a condition that causes blood clots in your small blood vessels)
- Can occur with Tecfidera:
- progressive multifocal leukoencephalopathy (a rare disease that can damage your brain) decreased level of lymphocytes (a type of white blood cell)
- severe infections, including herpes zoster (shingles)
- Can occur with both Plegridy and Tecfidera:
- severe allergic reaction
- liver injury, such as hepatitis (inflammation in your liver)
Effectiveness
The only conditions both Plegridy and Tecfidera are used to treat certain forms of relapsing-remitting MS.
These drugs haven’t been directly compared in clinical studies. But separate studies have found both Plegridy and Tecfidera to be effective in treating MS.
There’s currently an ongoing study comparing different treatments for MS. Both Plegridy and Tecfidera, along with other MS treatments, are being looked at in this study.
There’s also a study going on to test Plegridy versus Tecfidera in treating relapsing-remitting MS in children, but the results of this study haven’t been published yet. At this time, neither drug is approved for use in children with this condition.
Costs
Plegridy and Tecfidera are both brand-name drugs. There are currently no generic forms of either drug. Brand-name medications usually cost more than generics.
The actual price you’ll pay for either drug will depend on your insurance plan, your location, and the pharmacy you use.
You should take Plegridy according to your doctor or healthcare provider’s instructions.
Plegridy should be injected under your skin (called a subcutaneous injection). Your doctor or pharmacist will show you how to self-inject this medication.
The manufacturer of Plegridy provides written directions that show how to use the single-dose, prefilled pens and syringes. The manufacturer also offers an instructional video that shows how to use the single-dose, prefilled pen.
Always use a new pen or new syringe with each Plegridy injection. Never use a Plegridy pen or syringe more than once.
Plegridy should be stored in the refrigerator. (See the section below called “Plegridy expiration, storage, and disposal” for more information.)
When you’re ready to give yourself an injection of Plegridy, you should take the medication out of the refrigerator. And let the drug come to room temperature for about 30 minutes before injecting your dose.
Injection sites
Plegridy should be injected under the skin of your belly area, the back of your arms, or your thighs. It’s important to give yourself the injection into the tissue under your skin, being careful not to inject into your muscle.
You should alternate injection sites each time you inject Plegridy. This helps to decrease your risk of injection site reaction. (With an injection site reaction, you may have pain, redness, swelling, or other issues at the site of your injection.)
Be sure that you don’t inject Plegridy into any areas of your skin that look red, bruised, infected, or have any scarring.
When to take
Plegridy should be taken once every 14 days (2 weeks). You should inject your dose on the same day of the week for each treatment.
For example, if you take your first dose on a Sunday, you should take your next dose 14 days later on a Sunday. This is important to do because it helps to keep the same amount of medication in your body over time.
To help make sure that you don’t miss a dose, try setting a reminder on your phone. A medication timer may be useful, too.
Here are answers to some frequently asked questions about Plegridy.
What should I do if my Plegridy pen gets jammed?
You Plegridy pen might be jammed when the following situations occur:
- You don’t hear clicking sounds. When giving yourself a dose of Plegridy using a prefilled pen, you’ll hear the pen making a clicking sound during the injection. (You should continue holding the pen onto your skin until the clicking stops.) If you don’t hear the clicking sounds when attempting to inject the drug, your pen may be jammed.
- You don’t see green checkmarks in the injection site window on the pen. Before giving yourself a dose of Plegridy, you’ll see green stripes in the pen’s injection site window. (If you don’t see green stripes in the window before injecting, don’t use the pen.) After your dose has been injected, you should see green check marks in this window. If you don’t see green check marks after attempting to inject the drug, your pen may be jammed.
If your pen gets jammed, it’s hard to know how much of your dose you actually received. In this case, the best thing you can do is call your doctor or pharmacist. They can help you determine if you got any of your dose, or if you need to use another pen and try giving the dose a second time.
If you have questions or concerns, you can also call the manufacturer of Plegridy at 800-456-2255.
How long does Plegridy stay in your system?
Plegridy will stay in your body and work for 14 days after you take your dose. You’ll have the highest amount of medication in your body about 1 to 1.5 days after injecting your dose.
Over the following 2 weeks, the amount of medication in your body will slowly decrease, until it’s time for your next dose of Plegridy.
Will Plegridy cure my multiple sclerosis?
No, Plegridy doesn’t cure multiple sclerosis (MS). But the drug may decrease the number of relapses you have and help reduce your MS symptoms.
Is Plegridy an immunosuppressant?
Yes, it is. Although it’s not known exactly how Plegridy works, it’s
This helps to decrease the number of multiple sclerosis (MS) relapses that you have and to reduce your MS symptoms.
How can I lower my risk of having flu-like symptoms while I’m taking Plegridy?
Plegridy can sometimes cause bothersome side effects, including flu-like symptoms, such as headache and fever.
You can take certain medications before your dose of Plegridy to help lower your risk for flu-like symptoms.
For this use, your doctor may recommend that you take an over-the-counter fever reducer, such as acetaminophen (Tylenol). They may also recommend a pain reliever, such as ibuprofen (Motrin, Advil).
If you’re having flu-like symptoms during Plegridy treatment, talk with your doctor about ways to help relieve your discomfort.
There aren’t any known interactions between Plegridy and alcohol. However, liver injury is a possible side effect of Plegridy. Alcohol can also affect your liver and cause liver injury. Drinking alcohol during Plegridy treatment may increase your risk for liver problems.
Talk with your doctor about how much alcohol is safe to drink while you’re taking Plegridy.
Plegridy isn’t known to interact with any other medications. It’s also not known to interact with supplements or foods.
Plegridy and other medications
There aren’t any medications that are known to interact with Plegridy. This is because the active drug in Plegridy is a form of the interferon beta-1a protein. This protein is naturally made in your body. So even without taking Plegridy, you already have this interferon in your body.
However, before taking Plegridy, you should still talk with your doctor or pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you to avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Plegridy and herbs and supplements
There aren’t any herbs or supplements that have been specifically reported to interact with Plegridy. However, you should still check with your doctor or pharmacist before using any of these products while taking Plegridy.
Plegridy and foods
There aren’t any foods that have been specifically reported to interact with Plegridy. If you have any questions about eating certain foods with Plegridy, talk with your doctor.
It’s not known if Plegridy is safe to take while you’re pregnant. In fact, you shouldn’t use Plegridy during pregnancy unless the benefit of taking the drug is greater than the risk for harm to your pregnancy.
In animal studies, there wasn’t any effect in the development of fetuses when pregnant females were given interferon beta-1a every other day. (Plegridy is a form of interferon beta-1a.)
However, it’s possible that interferon beta-1a did increase the risk for miscarriage in these animals. But keep in mind that animal studies don’t always predict what’ll happen in humans.
If you’re pregnant or planning to become pregnant, talk to your doctor before taking Plegridy.
What if Plegridy is used during pregnancy?
If you do take Plegridy while you’re pregnant, or if you become pregnant while taking Plegridy, you should consider enrolling in the Plegridy pregnancy registry.
A pregnancy registry collects information about women who are taking certain medications during pregnancy. This information is helpful for doctors and other people considering using the drug while pregnant.
You can participate in the Plegridy registry by signing up online or calling 866-810-1462.
It’s not known if Plegridy is safe to take during pregnancy. If you’re sexually active and you or your partner can become pregnant, talk with your doctor about your birth control needs while you’re using Plegridy.
It’s not known if Plegridy is safe to take while you’re breastfeeding. It’s also not known if the drug is passed into breast milk when it’s taken by lactating women.
If you’re breastfeeding, talk with your doctor before taking Plegridy. They can recommend safe and healthy ways to feed your child.
As with all medications, the cost of Plegridy can vary.
The actual price you’ll pay will depend on your insurance plan, your location, and the pharmacy you use.
It’s important to note that you’ll have to get Plegridy at a specialty pharmacy. This type of pharmacy is authorized to carry specialty medications. These are drugs that may be expensive or may require help from healthcare professionals to be used safely and effectively.
Your insurance plan may require you to get prior authorization before they approve coverage for Plegridy.
This means that your doctor and insurance company will need to communicate about your prescription before the insurance company will cover the drug. The insurance company will review the request and let you and your doctor know if your plan will cover Plegridy.
If you’re not sure if you’ll need to get prior authorization for Plegridy, contact your insurance plan.
Financial and insurance assistance
If you need financial support to pay for Plegridy, or if you need help understanding your insurance coverage, help is available.
Biogen, the manufacturer of Plegridy, offers a program called Above MS. Through this program, you can find out information about your insurance coverage and ways to save on Plegridy. For more information and to find out if you’re eligible for support, call 800-456-2255 or visit the program website.
Plegridy is approved for certain uses in adults with multiple sclerosis (MS). With MS, your immune system attacks the tissue around your nerves, which is called the myelin sheath. This can cause problems with how well the cells inside your brain and spinal cord can communicate with each other.
MS may cause symptoms such as trouble walking or vision changes. It may also cause numbness or tingling in your arms, legs, or other areas of your body.
It’s not known for sure how Plegridy works to treat MS. However, it’s
How long does it take to work?
Plegridy will start working as soon as you take your first dose. However, it may take a few doses of Plegridy before you begin to notice a decrease in your MS symptoms. (And keep in mind that Plegridy doses are typically given every 2 weeks.)
Before taking Plegridy, talk with your doctor about your health history. Plegridy may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Seizure disorders. Seizures are a rare, but possible, side effect of Plegridy. If you already have a seizure disorder, you may have an increased risk for seizures when taking Plegridy. If you have epilepsy (a seizure disorder) or a history of seizures, talk with your doctor before starting Plegridy.
- Heart conditions, such as congestive heart failure. While taking Plegridy, it’s possible to develop a heart condition, such as congestive heart failure. If you already have heart problems, you have an increased risk of developing heart-related symptoms or your condition getting worse. Talk with your doctor about any heart issues you have before taking Plegridy. If you do have a heart problem, your doctor may monitor you more often than usual during treatment to be sure that your heart condition doesn’t worsen.
- Depression or mental illness. If you’ve had a mental illness or depression in the past, you may have an increased risk for depression or thoughts of suicide when taking Plegridy. It’s very important that if you feel depressed or have thoughts of suicide, call your doctor right away. They can recommend ways to improve your condition. They may also recommend that you use a medication other than Plegridy.
- Liver conditions. It’s possible that Plegridy may cause injury to your liver. If you already have liver problems, taking Plegridy may worsen your condition. Talk with your doctor about any liver problems you have before starting Plegridy. During treatment, your doctor may monitor your liver more often than usual to be sure that your liver condition doesn’t worsen.
- Low blood counts. Plegridy may decrease the level of certain blood cells in your body, especially of white blood cells or platelets. If you already have a condition that causes a low white blood cell level, you may have an increased risk for infection when using Plegridy. If your white blood cell level gets too low, it can be dangerous to your health. Your doctor will monitor your blood cell levels while you’re taking Plegridy. This helps them to be sure that your levels don’t get too low.
- Pregnancy. It’s not known if Plegridy is safe to take while you’re pregnant. If you’re pregnant, or planning to become pregnant, talk with your doctor before starting Plegridy. For more information, please see the “Plegridy and pregnancy” section above.
- Breastfeeding. It’s not known if Plegridy is safe to take while you’re breastfeeding. If you’re currently breastfeeding, talk with your doctor before starting Plegridy. For more information, please see the “Plegridy and breastfeeding” section above.
- Allergic reaction. Plegridy shouldn’t be used by anyone who’s had an allergic reaction to interferon beta-1a, pegylated interferon, or any ingredient in Plegridy. If you have a history of allergic reaction to any of these ingredients, you shouldn’t take Plegridy. Talk with your doctor about other treatment options that are safe for you.
Note: For more information about the potential negative effects of Plegridy, see the “Plegridy side effects” section above.
Using more than the recommended dosage of Plegridy may lead to serious side effects. To help prevent overdose, never use more Plegridy than your doctor recommends.
Overdose symptoms
It’s not known what symptoms may occur if you take too much Plegridy. In clinical trials, no one using Plegridy overdosed on the drug.
What to do in case of overdose
If you think you’ve taken too much of this drug, call your doctor. You can also call the American Association of Poison Control Centers at 800-222-1222 or use their online tool. But if your symptoms are severe, call 911 or go to the nearest emergency room right away.
When you get Plegridy from the pharmacy, your pharmacist will add an expiration date to the label on the box. This date is typically 1 year from the date they dispensed the medication.
The expiration date helps guarantee that the medication is effective during this time. The
If you have unused medication that has gone past the expiration date, talk to your pharmacist about whether you might still be able to use it.
Storage
How long a medication remains good can depend on many factors, including how and where you store the medication.
Plegridy should be stored in a refrigerator, at a temperature between 36°F and 46°F (2°C and 8°C). The drug should be kept in its original carton until you’re ready to use it. It should also be protected from light. Plegridy should never be frozen.
If you don’t have access to a refrigerator, Plegridy can be stored between 36°F and 77°F (2°C and 25°C) for a up to 30 days. (It’s still important to protect the drug from light during this time.)
You shouldn’t store Plegridy outside of the refrigerator for longer than 30 days. And after these 30 days, you’ll need to dispose of the medication.
Before injecting doses of Plegridy, you’ll need to take the medication out of the refrigerator. Let it come to room temperature for about 30 minutes before taking your dose. Never heat Plegridy with hot water or sunlight to bring it to room temperature.
Disposal
If you no longer need to take Plegridy and have leftover medication, it’s important to dispose of it safely. This helps prevent others, including children and pets, from taking the drug by accident. It also helps keep the drug from harming the environment.
Be sure to dispose of used Plegridy syringes and pens in a sharps disposal container. For more information about how to get rid of your used needles, see the
The
The following information is provided for clinicians and other healthcare professionals.
Indications
Plegridy is indicated for use in adults with MS symptoms in the following situations:
- clinically isolated syndrome
- relapsing-remitting disease
- active secondary progressive disease
Mechanism of action
It’s not known exactly how Plegridy works to treat MS. However, the drug is
Overall, interferon beta is believed to decrease inflammation and block the immune system from being overactive. However, it’s not fully understood how the drug works to treat MS.
Pharmacokinetics and metabolism
Maximum concentration of Plegridy is reached about 1 to 1.5 days post-dose. It’s eliminated mainly by renal pathways. Plegridy has a half-life of about 78 hours when tested in people with MS.
Contraindications
Plegridy is contraindicated in people who have had an allergic reaction to interferon beta-1a, peginterferon, or any ingredients in Plegridy.
Storage
Plegridy should be kept refrigerated, between 36°F and 46°F (2°C and 8°C). Until use, the drug should be stored in its original carton and protected from light. Plegridy should never be frozen.
Plegridy can also be stored between 36°F and 77°F (2°C and 25°C) for a maximum of 30 days. It’s still important to protect Plegridy from light during this time. Plegridy shouldn’t be kept outside of the refrigerator for longer than 30 days.
When the drug is needed for injection, it should be taken out of the refrigerator and allowed to come to room temperature for approximately 30 minutes before the dose is injected. Never heat Plegridy with hot water or sunlight to bring it to room temperature.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up-to-date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.