Emflaza is a brand-name oral liquid suspension and oral tablet prescribed for Duchenne muscular dystrophy (DMD). Emflaza contains the active drug deflazacort and belongs to the corticosteroid drug class.
Emflaza is FDA-approved to treat DMD in adults and children ages 2 years and older. DMD is a genetic (inherited) condition that causes muscle weakness.
For details about this condition and how the drug treats it, see the “Emflaza uses” section below.
Drug details
You’ll find key information about Emflaza below.
- Drug forms: Oral liquid suspension, oral tablet
- Generic available? No
- Prescription required? Yes
- Controlled substance? No
- Year of FDA approval: 2017
Emflaza contains the active drug deflazacort. Emflaza is available only as a brand-name medication. It’s not currently available in generic form.
A generic drug is an exact copy of the active drug in a brand-name medication. Generics typically cost less than brand-name drugs.
As with all medications, the cost of Emflaza can vary. The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
Keep in mind that you may be able to get a 90-day supply of Emflaza. If approved by your insurance company, getting a 90-day supply of the drug could reduce your number of trips to the pharmacy and help lower the cost. If you’re interested in this option, check with your doctor, pharmacist, or insurance company.
It’s important to note that you’ll have to get Emflaza at a specialty pharmacy. This type of pharmacy is authorized to carry specialty medications. These are drugs that may be expensive or may require help from healthcare professionals to be taken safely and effectively.
Before approving coverage for Emflaza, your insurance company may require you to get prior authorization. This means that your doctor and insurance company will need to communicate about your prescription before the insurance company will cover the drug. The insurance company will review the prior authorization request and decide if the drug will be covered.
If you’re not sure whether you’ll need to get prior authorization for Emflaza, contact your insurance company.
Financial and insurance assistance
If you need financial support to pay for Emflaza, or if you need help understanding your insurance coverage, help is available.
PTC Therapeutics, the manufacturer of Emflaza, offers a support program called PTC Cares. For more information and to find out if you’re eligible for support, call 844-478-2227 or visit the program website.
To learn more about saving money on prescriptions, check out this article.
Mail-order pharmacies
Emflaza may be available through a mail-order pharmacy. Using this service may help lower the drug’s cost and allow you to get your medication without leaving home.
If recommended by your doctor, you may be able to receive a 90-day supply of Emflaza, so there’s less concern about running out of the medication. If you’re interested in this option, check with your doctor, pharmacist, or insurance company. Some Medicare plans may help cover the cost of mail-order medications.
If you don’t have insurance, you can ask your doctor or pharmacist about online pharmacy options.
Generic version
Emflaza is not available in a generic form. A generic drug is an exact copy of the active drug in a brand-name medication. Generics tend to cost less than brand-name drugs.
Emflaza can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Emflaza. These lists do not include all possible side effects.
For more information about the possible side effects of Emflaza, talk with your doctor or pharmacist. They can give you tips on how to manage any side effects that may be concerning or bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs it has approved. If you would like to notify the FDA about a side effect you’ve had with Emflaza, you can do so through MedWatch.
Mild side effects
Mild side effects* of Emflaza can include:
- abdominal pain
- changes in levels of electrolytes such as sodium, calcium, and potassium
- cough
- hirsutism (unusual hair growth on your body)
- frequent urination
- increased appetite
- irritability
- runny nose
- water retention
- weight gain or increased abdominal fat
- mild infection†
Most of these side effects may go away within a few days or a couple of weeks. However, if they become more severe or don’t go away, talk with your doctor or pharmacist.
* This is a partial list of mild side effects from Emflaza. To learn about other mild side effects, talk with your doctor or pharmacist, or view Emflaza’s prescribing information.
† For more information about this side effect, see “Side effect details” below.
Serious side effects
Serious side effects from Emflaza aren’t common. However, they can occur. Call your doctor right away if you have serious side effects. Call 911 or your local emergency number if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include:
- Blood clots. Symptoms vary depending on where the blood clot occurs. They can include:
- warmth, pain, or swelling in your arms or legs
- shortness of breath
- chest pain
- Eye problems such as eye infection, cataracts, or glaucoma. Symptoms vary depending on the exact eye problem. They can include:
- blurry vision
- vision loss
- trouble seeing in dim lighting
- severe eye pain
- Bone loss. Symptoms can include:
- joint pain
- fractures (broken bones)
- High blood sugar. Symptoms can include:
- Kaposi sarcoma (a rare type of cancer). Symptoms can include:
- skin nodules (bumps), plaques, or patches, typically on the face or legs
- skins spots that are red, purple, brown, or otherwise discolored
- Mood or behavior changes. Symptoms can include:
- depression
- euphoria (feeling “high”)
- mania (moments of extremely high energy and excitement)
- High blood pressure. Symptoms may not occur unless the condition is severe. They can include:
- sweating
- headache
- nosebleeds
- Allergic reaction.*
- Cushing’s syndrome.*
- Serious infection.*
- Serious rash.*
* For more information about this side effect, see “Side effect details” below.
Side effects in children
Emflaza is approved to treat Duchenne muscular dystrophy in children ages 2 years and older.
Most side effects of Emflaza in children are expected to be the same as those in adults. (For details, see “Mild side effects” and “Serious side effects” above.)
In addition, long-term treatment with corticosteroids may slow growth in children. (Emflaza is a type of corticosteroid.) However, this side effect wasn’t reported in clinical trials of Emflaza. Your child’s doctor will recommend the length of time your child can safely take the drug.
If you have questions about how Emflaza may affect your child, talk with their doctor.
Side effect details
Here’s some detail on certain side effects this drug may cause. To find out how often side effects occurred in clinical trials, see the prescribing information for Emflaza.
Cushing’s syndrome
Cushing’s syndrome is the most common side effect of Emflaza. This condition is caused by a high level of cortisol in the blood. Cortisol is a hormone your body produces naturally. However, corticosteroids (such as Emflaza) also mimic the activity of cortisol in your body.
Over time, a high level of cortisol in your blood can lead to Cushing’s syndrome. Symptoms of this condition include:
- weight gain
- moon face (swelling that makes your face appear puffy and round)
- buffalo hump (buildup of fat on the back of the shoulders and neck)
- thinning skin
- bruising more easily than is typical
What you can do
If you’re concerned about Cushing’s syndrome while taking Emflaza, talk with your doctor. They can recommend ways to lower your risk of this side effect, such as taking the drug for only a short time.
Infection
Emflaza can lessen the activity of the immune system, which could increase your risk of infection.
The most common infections reported in clinical trials of Emflaza were upper respiratory infections. An example of an upper respiratory infection is the common cold.
Examples of less common mild infections reported in trials include urinary tract infection, influenza (flu), and ear infections.
The exact symptoms you experience will depend on the specific infection you may have. However, common symptoms of infection include:
In rare cases, Emflaza may cause more serious cases of certain infections. Examples include chickenpox and measles.
What you can do
Talk with your doctor about your risk of infection with Emflaza. Be sure to tell them if you’ve been around anyone who has an infection, especially chickenpox or measles. Also, let them know if you have hepatitis B virus (HBV) or have had it in the past. Taking Emflaza may worsen HBV or cause it to come back.
Your doctor will watch you closely for symptoms of an infection while you take Emflaza.
Serious rash
A serious rash is a rare side effect of Emflaza.
Keep in mind that a serious rash can be a symptom of toxic epidermal necrolysis (TEN). TEN is a rare, potentially life threatening condition. With TEN, you may have a rash that occurs along with painful skin blistering or peeling. You may also have flu-like symptoms such as body aches, fever, or runny nose.
In people who developed TEN in clinical trials, symptoms typically appeared within the first 8 weeks of starting treatment with Emflaza.
What you can do
If you develop a rash with Emflaza, stop taking the drug and tell your doctor right away. It is particularly important to tell them if you have other symptoms of TEN along with a rash.
Your doctor can advise if you may have TEN. If they find you do, they’ll likely have you go to a hospital right away for treatment.
Allergic reactionAs with most drugs, some people can have an allergic reaction after taking Emflaza. This side effect wasn’t reported in initial clinical trials of the drug. However, allergic reaction has been reported after Emflaza became available for prescription.
Symptoms of a mild allergic reaction can include:
A more severe allergic reaction is rare. However, it is possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
Call your doctor right away if you have an allergic reaction to Emflaza, as the reaction could become severe. Call 911 or your local emergency number if your symptoms feel life threatening or if you think you’re having a medical emergency.
The Emflaza dosage your doctor prescribes will depend on several factors. These include:
- your body weight
- the form of Emflaza you take
- other medications you may take
The following information describes dosages that are commonly prescribed or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosing to fit your needs.
Drug forms and strengths
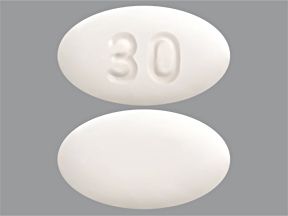
Emflaza comes in two forms. Each form comes in different strengths:
- oral liquid suspension: 22.75 milligrams per milliliter (mg/mL)
- oral tablet: 6 mg, 18 mg, 30 mg, and 36 mg
Dosage for Duchenne muscular dystrophy
The typical dosage of Emflaza for Duchenne muscular dystrophy (DMD) is 0.9 mg per kilogram (kg)* of body weight, given once per day.
For example, a person who weighs 66 kg (about 145 lb) will take 60 mg of Emflaza once per day.
* 1 kg is about 2.2 pounds (lb).
Children’s dosage
Emflaza is approved to treat DMD in children ages 2 years and older.
The dosage of Emflaza for children is the same as the dosage prescribed for DMD in adults.
For more information, see the “Dosage for Duchenne muscular dystrophy” section directly above.
What if I miss a dose?
The manufacturer of Emflaza hasn’t provided recommendations for what to do if you miss a dose of Emflaza.
If you do miss a dose, talk with your doctor or pharmacist. They can recommend if you should take the missed dose or skip it.
To help make sure that you don’t miss a dose, try using a medication reminder. This can include setting an alarm or using a timer. You could also download a reminder app on your phone.
Will I need to take this drug long term?
Emflaza is meant to be a long-term treatment. If you and your doctor determine that Emflaza is safe and effective for you, you’ll likely take it long term.
For a detailed look at Emflaza and dosage, including how to take the drug, see this article.
Other drugs are available that can treat your condition. Some may be a better fit for you than others. If you’re interested in finding an alternative to Emflaza, talk with your doctor. They can tell you about other medications that may work well for you.
Note: Some of the drugs listed here are prescribed off-label to treat these specific conditions. Off-label drug use is when a drug that’s approved by the Food and Drug Administration (FDA) is prescribed for a purpose other than what it’s approved for.
Alternatives for Duchenne muscular dystrophy
Examples of other drugs that may be prescribed to treat Duchenne muscular dystrophy include:
- casimersen (Amondys 45)
- eteplirsen (Exondys 51)
- golodirsen (Vyondys 53)
- viltolarsen (Viltepso)
- other corticosteroids such as prednisone (Rayos)
Emflaza is approved to treat Duchenne muscular dystrophy (DMD) in adults and children ages 2 years and older.
DMD is a genetic (inherited) condition. It occurs because the body has trouble making enough of a protein that helps strengthen and protect muscles. Without enough of this protein, muscles become weak and damaged.
Emflaza’s mechanism of action (how it works) for treating DMD isn’t fully understood. It’s thought to help slow down the muscle weakness and damage that happen with DMD.
How long does it take to work?
Emflaza starts working right away to treat DMD. However, it may take a few weeks for the symptoms of your condition to ease.
The Food and Drug Administration (FDA) approves prescription drugs such as Emflaza to treat certain conditions.
Emflaza for Duchenne muscular dystrophy
Emflaza is FDA-approved to treat Duchenne muscular dystrophy (DMD) in adults and children ages 2 years and older.
DMD is a genetic (inherited) condition that typically affects male* children. However, in rare cases, DMD can also affect female* children and young adults.
DMD occurs because the body has trouble making enough dystrophin. This is a protein that helps strengthen muscles and protect them from injury. However, without enough dystrophin, muscles become damaged and weakened over time.
Symptoms of DMD include:
- fatigue
- muscle weakness
- trouble walking or inability to walk
- enlarged calves
- learning difficulties such as dyslexia
* Sex and gender exist on spectrums. Use of the terms “male” and “female” in this article refers to sex assigned at birth.
Effectiveness for DMD
Emflaza has been found to be an effective treatment for DMD.
Treatment guidelines from the Centers for Disease Control and Prevention (CDC) include corticosteroids (such as Emflaza) as a recommended treatment option.
It’s important to note that although Emflaza is approved for use in adults and children, clinical trials of Emflaza only included male children ages 5 to 15 years old. The trials didn’t include female children or adults.
For information about how the drug performed in clinical trials, see Emflaza’s prescribing information.
Emflaza and children
Emflaza is approved to treat DMD in adults and children ages 2 years and older.
To learn more about this condition, see “Emflaza for Duchenne muscular dystrophy” above.
There aren’t any known interactions between Emflaza and alcohol.
If you drink alcohol, talk with your doctor about the amount you can safely consume while taking Emflaza.
Emflaza can interact with several other medications. It can also interact with certain supplements as well as certain foods.
Different interactions can cause different effects. For instance, some interactions can interfere with how well a drug works. Other interactions can increase side effects or make them more severe.
Emflaza and other medications
Below is a list of medications that can interact with Emflaza. This list does not contain all drugs that may interact with Emflaza.
Before taking Emflaza, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also, tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Types of drugs that can interact with Emflaza include:
- Certain antibiotics, such as clarithromycin. These drugs are prescribed to treat infections caused by bacteria. Taking Emflaza with these medications can increase your risk of side effects with Emflaza.
- Certain antifungals, such as fluconazole (Diflucan). These medications are prescribed to treat infections caused by fungi. Taking Emflaza with these drugs can increase your risk of side effects with Emflaza.
- Certain calcium channel blockers, such as diltiazem (Cardizem, Cartia XT) or verapamil (Calan SR, Verelan). These drugs are prescribed to treat heart conditions, such as high blood pressure. Taking Emflaza with these medications can increase your risk of side effects with Emflaza.
- Certain antiretroviral drugs, such as efavirenz (Sustiva). These drugs are prescribed to treat HIV. Taking Emflaza with these medications can make Emflaza less effective.
- Certain antiepileptic drugs, such as carbamazepine (Carbatrol, Tegretol) and phenytoin (Dilantin). These medications are prescribed to treat seizures. Taking Emflaza with these drugs can make Emflaza less effective.
Emflaza and herbs and supplements
There aren’t any herbs or supplements that have been specifically reported to interact with Emflaza. However, you should still check with your doctor or pharmacist before using any of these products while taking Emflaza.
Emflaza and foods
You should not eat grapefruit or drink grapefruit juice while taking Emflaza. Grapefruit may increase your risk of side effects from the drug.
If you have questions about eating certain foods while you’re taking Emflaza, talk with your doctor.
Emflaza and vaccines
It’s recommended that you don’t receive live vaccines while taking Emflaza. (Live vaccines are made from a weakened form of the virus or bacteria the vaccine protects against.)
Emflaza can lessen the activity of your immune system. And this could increase your risk of getting the infection that live vaccines are meant to protect you from.
Examples of vaccines that should be avoided with Emflaza include:
- yellow fever
- measles, mumps, rubella (MMR)
- chickenpox
- nasal flu spray (FluMist)
The manufacturer of Emflaza hasn’t provided recommendations for inactive (non-live) vaccines.
Talk with your doctor about whether you’re up to date on all recommended vaccines before starting Emflaza. To be safe, you should avoid getting a live vaccine in the 4 to 6 weeks before starting the drug. Your doctor will advise if it’s safe to get inactive vaccines with Emflaza.
You should take Emflaza according to the instructions your doctor gives you.
Emflaza comes as an oral tablet or oral liquid suspension. For more information about how to take Emflaza, visit the drug manufacturer’s website.
When to take
You’ll likely take Emflaza once a day. Try to take your Emflaza doses at the same time each day. This helps make sure you have a steady level of the drug in your body, which helps it work most effectively.
To help make sure that you don’t miss a dose, try using a medication reminder. This can include setting an alarm or using a timer. You could also download a reminder app on your phone.
Accessible labels and containers
Some pharmacies offer labels that have large print, braille, or a code you scan with a smartphone to convert text to speech. If your local pharmacy doesn’t have these options, your doctor or pharmacist may be able to direct you to one that does.
If you have trouble opening medication bottles, ask your pharmacist if they can put Emflaza tablets in an easy-open container. They also may be able to recommend tools that can make it simpler to open lids.
Taking Emflaza with food
Emflaza can be taken with or without food.
Can Emflaza be crushed, split, or chewed?
If possible, Emflaza tablets should be swallowed whole. Emflaza tablets should not be chewed or crushed.
However, if you (or your child) have trouble swallowing Emflaza tablets, you can crush them and mix the crushed tablets with applesauce. Or you can ask your doctor if the Emflaza oral liquid suspension is a better option.
It’s not known if Emflaza is safe to take while pregnant. The drug hasn’t been trialed during pregnancy.
However, corticosteroids may cause side effects in children born to people who took the drug during pregnancy. (Emflaza is a type of corticosteroid.) Examples include low birth weight or having cleft lip and cleft palate.
If you’re pregnant or planning to become pregnant while taking Emflaza, talk with your doctor. They’ll discuss the risks and benefits of Emflaza treatment with you.
It’s not known whether Emflaza is safe to take during pregnancy. If you’re planning a pregnancy or you or your partner can become pregnant, talk with your doctor about your birth control needs while you’re taking Emflaza.
For more information about taking Emflaza during pregnancy, see the “Emflaza and pregnancy” section above.
It’s not known whether it’s safe to take Emflaza while breastfeeding. Taking this drug while breastfeeding hasn’t been trialed.
However, corticosteroids are known to pass into breast milk. Emflaza is a corticosteroid. So it’s possible that Emflaza may pass into breast milk. This could cause side effects in a child who is breastfed.
If you’re breastfeeding or planning to breastfeed, talk with your doctor before taking Emflaza.
Here are answers to some frequently asked questions about Emflaza.
Is weekend dosing an option with Emflaza treatment?
The manufacturer of Emflaza hasn’t recommended a weekend dosing schedule for the drug. However, in some cases, doctors may prescribe weekend doses of Emflaza for Duchenne muscular dystrophy (DMD) instead of daily doses.
A weekend dosing schedule is when your doctor recommends taking your medication on the weekends only, instead of every day. The dose you receive for weekend dosing will usually be higher than the dose you received daily.
Weekend dosing might be prescribed because daily, long-term treatment with corticosteroids such as Emflaza can increase the risk of side effects from these drugs. Examples include slowed growth in children and bone loss. It’s thought that weekend dosing may lower the risk of side effects from corticosteroids while still being effective for DMD treatment.
If you’re interested in learning about weekend dosing with Emflaza, talk with your doctor.
Is Emflaza a steroid?
Yes, Emflaza is a corticosteroid.
To learn about its use for DMD, see the “Emflaza uses” section above. And to learn how the drug works to treat DMD, see “How Emflaza works” above.
Is it safe for older adults to take Emflaza?
It isn’t known whether it’s safe for older adults to take Emflaza.
Emflaza is prescribed to treat DMD, which typically affects male* children. However, in rare cases, DMD can also affect female* children and young adults.
Because DMD doesn’t typically affect older adults (ages 65 years and over), people of this age weren’t included in clinical trials of Emflaza.
To learn more about possible uses of Emflaza in older adults, talk with your doctor or pharmacist.
* Sex and gender exist on spectrums. Use of the terms “male” and “female” in this article refers to sex assigned at birth.
This drug comes with several precautions.
Before taking Emflaza, talk with your doctor about your health history. Emflaza may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Eye problems. Before starting Emflaza treatment, tell your doctor if you have eye problems. The drug could worsen certain eye problems, including cataracts and glaucoma. If you have eye problems, your doctor can recommend if it’s safe for you to take Emflaza.
- Diabetes. Before starting Emflaza, tell your doctor if you have diabetes. Emflaza may cause high blood sugar. This could worsen your diabetes or make your diabetes medications less effective. Your doctor will advise if it’s safe for you to take Emflaza.
- Stomach problems. Before taking Emflaza, tell your doctor if you have stomach problems. This includes conditions such as diverticulitis, ulcers, and ulcerative colitis. Emflaza may cause perforation (holes) in the stomach or intestines in people who have these conditions. Your doctor can recommend if it’s safe for you to take Emflaza.
- Heart failure. Before starting treatment with Emflaza, tell your doctor if you have heart failure. Emflaza may cause changes in levels of electrolytes such as sodium and potassium, which could worsen your condition. Your doctor may prescribe potassium supplements or suggest you limit your sodium intake while taking Emflaza.
- High blood pressure. Before you start taking Emflaza, tell your doctor if you have high blood pressure. Emflaza may cause changes in your body’s sodium level, which could worsen your condition. Your doctor may suggest that you limit your sodium intake while taking Emflaza.
- Kidney problems. Tell your doctor if you have any kidney problems before starting treatment with Emflaza. The drug may affect the levels of sodium, calcium, and potassium in your body. And having kidney problems could worsen this side effect. Your doctor can advise if it’s safe to take Emflaza.
- Osteoporosis. Before taking Emflaza, tell your doctor if you have osteoporosis. The drug may cause bone loss, which could worsen this condition. Your doctor can determine if it’s safe for you to take Emflaza.
- Hepatitis B virus (HBV). Before taking Emflaza, tell your doctor if you have HBV. Emflaza may reactivate HBV, which could lead to symptoms of hepatitis B. (Reactivation happens when a virus that’s already inside your body causes symptoms.) If you have HBV, your doctor can advise whether Emflaza is right for you.
- Pheochromocytoma. If you have pheochromocytoma (a type of tumor on your adrenal gland), taking Emflaza may worsen your condition. Tell your doctor if you have pheochromocytoma before starting treatment with Emflaza. They may want to prescribe a treatment other than Emflaza for you.
- Thyroid problems. If you have thyroid problems, such as overactive or underactive thyroid, taking Emflaza may worsen your condition. Tell your doctor if you have thyroid problems before taking Emflaza. They may adjust your thyroid medications or prescribe a drug other than Emflaza for you.
- Allergic reaction. If you’ve had an allergic reaction to Emflaza or any of its ingredients, your doctor will likely not prescribe Emflaza. Ask your doctor what other medications are better options for you.
- Pregnancy. It may not be safe to take Emflaza during pregnancy. For more information, see the “Emflaza and pregnancy” section above.
- Breastfeeding. It isn’t known for sure whether Emflaza passes into breast milk during breastfeeding. For more information, see the “Emflaza and breastfeeding” section above.
Note: For more information about the potential negative effects of Emflaza, see the “Emflaza side effects” section above.
Do not take more Emflaza than your doctor recommends. For some drugs, doing so may lead to unwanted side effects or overdose.
What to do in case you take too much Emflaza
If you think you’ve taken too much of this drug, call your doctor. You can also call America’s Poison Centers at 800-222-1222 or use its online tool. However, if your symptoms are severe, call 911 or your local emergency number or go to the nearest emergency room right away.
There haven’t been clinical trials on whether Emflaza can cause drug dependence. (With dependence, your body gets used to a drug and needs it to feel as you typically do.)
You may have withdrawal symptoms if you suddenly stop taking corticosteroids such as Emflaza. Withdrawal symptoms are uncomfortable effects that occur when you stop taking a drug or substance that your body is used to. In rare cases, withdrawal from corticosteroids may be life threatening.
Symptoms of withdrawal from corticosteroids such as Emflaza may include:
These symptoms may last a few days or up to several months after you stop taking Emflaza.
It’s important that you do not stop taking Emflaza unless your doctor recommends it. If you both agree it’s safe to stop the drug, your doctor can suggest ways to lessen your risk of withdrawal symptoms. For example, they’ll likely decrease your dosage slowly over time.
If you’re concerned about your risk of withdrawal and dependence while taking Emflaza, talk with your doctor.
When you get Emflaza from the pharmacy, the pharmacist will add an expiration date to the label on the container. This date is typically 1 year from the date they dispensed the medication.
The expiration date helps guarantee that the medication is effective during this time. The current stance of the
Storage
How long a medication remains good to take can depend on many factors, including how and where you store the medication.
Emflaza tablets and suspension should be stored at a room temperature between 68°F to 77°F (20°C to 25°C). The drug can be temporarily stored at temperatures between 59°F to 86°F (15°C to 30°C), such as when traveling. Dispose of any unused Emflaza oral suspension 1 month after you first opened the bottle. Avoid storing Emflaza in areas where it could get damp or wet, such as bathrooms.
Disposal
If you no longer need to take Emflaza and have leftover medication, it’s important to dispose of it safely. This helps prevent others, including children and pets, from taking the drug by accident. It also helps keep the drug from harming the environment.
This article provides several useful tips on medication disposal. You can also ask your pharmacist for information about how to dispose of your medication.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.